Abstract
Children with congenital heart disease (CHD) are at risk for both COVID-19 and secondary cardiovascular outcomes. Their increased cardiovascular risk may be mitigated through physical activity, but public health measures implemented for COVID-19 can make physical activity challenging. We objectively measured the impact of the COVID-19 pandemic on physical activity, continuously measured by Fitbit step counts, in children with CHD. Step counts were markedly lower in late March and early April 2020, compared with 2019 and early March 2020. It is vital to understand how precautions for COVID-19 will affect the health of children with CHD, especially if they persist long term.
Résumé
Les enfants atteints d’une cardiopathie congénitale (CC) sont exposés au risque de la COVID-19 et à des issues cardiovasculaires secondaires. L’augmentation de leurs risques cardiovasculaires peut être atténuée par l’activité physique, mais les mesures de santé publique mises en place dans le contexte de la COVID-19 peuvent rendre difficile la pratique de l’activité physique. Nous avons évalué de manière objective les répercussions de la pandémie de la COVID-19 sur l’activité physique, mesurée en continu par le compte-pas Fitbit, chez les enfants atteints de CC. À la fin de mars et au début d’avril 2020, le nombre de pas était nettement inférieur à 2019 et au début de mars 2020. Il est essentiel de comprendre comment les mesures préventives mises en place dans le contexte de la COVID-19 nuiront à la santé des enfants atteints de CC, particulièrement si la situation persiste à long terme.
There are minimal data available about COVID-19 in children, especially those with underlying medical conditions who are at increased risk of severe infection. The April 6, 2020, report from the Centers for Disease Control and Prevention COVID-19 Response Team showed that children with underlying medical conditions represent 23% of the total pediatric COVID-19 cases and 77% of those hospitalized.1 In addition to this increased COVID-19 risk common to children with underlying medical conditions, those with congenital heart disease (CHD) are known to be at higher risk of secondary cardiovascular outcomes long term.2 , 3 Physical activity is a modifiable risk factor that is particularly important for this high-risk population.4 The impact of public health measures on vulnerable populations, such as children with CHD, is important to quantify. The duration of the public health measures is unknown but may last for a year or more. Data about collateral health impacts are needed to help inform policy makers about the pros and cons of such measures as the epidemiology of COVID-19 evolves.
Physical activity is important for cardiovascular health as well as general health and quality of life, especially in patients with CHD.4 During the COVID-19 pandemic, physical activity may be even more crucial, especially for at-risk groups, owing to its physical and mental health benefits.5 , 6 Unfortunately, because of public health orders, recommendations to stay at home, school and park closures, and self-isolation by high-risk groups, it is more challenging than usual to continue normal physical activity patterns.5 , 6 In addition, because of patient and family concern about CHD children being particularly vulnerable, their social isolation and physical inactivity may be exacerbated more than the general population’s. To date, there are no objective data to demonstrate how physical activity patterns in children with CHD may have changed due to COVID-19, or what impact this may have on these patients’ health over the short and long terms.
In the present study, we aimed to quantify the change in physical activity observed during the early phase of the COVID-19 pandemic in children with CHD.
Methods
Data were collected as part of an ongoing prospective cohort study in children with moderate to severe CHD. The study was approved by the University of British Columbia Research Ethics Board (no. H17-01233). Children aged 9-16 years with coarctation of the aorta (COA), tetralogy of Fallot (TOF), transposition of the great arteries (TGA), or Fontan circulation (FON) were recruited from April 2017 to March 2020 at the British Columbia Children’s Hospital (BCCH) Heart Centre in Vancouver or partnership clinics throughout British Columbia and the Yukon. BCCH is the only pediatric tertiary hospital for the province, and almost all patients with CHD in BC are followed in one of these settings. Participants were provided a Fitbit Charge 2 (Fitbit, San Francisco, CA), and were asked to wear and sync the device regularly for 24 months. Wristband size and placement were in accordance with manufacturer guidelines. Fitbit data were collected and managed with the use of Research Electronic Data Capture (REDCap) tools hosted at BCCH.7 , 8 Fitbit data were autoexported to REDCap with the use of the application programming interface.
In the absence of any consensus on wear time validation for commercial trackers in children, we considered a day to be valid if they had at least 1000 steps. Weekly (Monday-Sunday) step counts were calculated by averaging the step counts from all the valid days of each week. We have previously validated this device for quantifying physical activity in children with CHD.9 We defined meeting physical activity guidelines as having ≥ 12,000 steps per day.9 , 10 Step count data were taken from the beginning of 2020 to April 5 and compared with corresponding weeks in 2019.
Descriptive statistics (n [%] or mean ± SD) were calculated for applicable variables. Distributions of continuous variables were assessed visually. The “lowess” function in R was used to generate a physical activity lines of best fit from the Fitbit step counts. Between-week differences were assessed via 1-way analysis of variance (with post hoc Bonferroni correction). Student t tests were used for continuous variables and chi-square tests for categoric variables. All analyses were performed in R (v. 3.6.3) using R Studio (v. 1.1.463), and significance was set at P < 0.05.
Results
A total of 109 children had valid data during the measurement periods; 56 participants had valid data available for both the 2019 and 2020 periods, 83 had valid data for the 2019 period (age 13.0 ± 2.3 years, 48 [57.8%] male), and 82 for 2020 (age 13.2 ± 2.3 years, 43 [52.4%] male). There were no significant differences in participant characteristics between the 2019 and 2020 groups; overall data are presented in Table 1 .
Table 1.
Patient demographics and Fitbit step counts
| Variable | 2019 | 2020 | P value |
|---|---|---|---|
| N | 83 | 82 | 0.938 |
| Age | 13.0 ± 2.3 | 13.2 ± 2.3 | 0.711 |
| Male | 48 (58%) | 43 (52) | 0.589 |
| Diagnosis | 0.983 | ||
| Coarctation of the aorta | 21 (25%) | 22 (27%) | |
| Tetralogy of Fallot | 23 (28%) | 22 (27%) | |
| Transpositon of the great arteries | 17 (21%) | 18 (22%) | |
| Fontan circulation | 22 (27%) | 20 (24%) | |
| Step counts | |||
| Week 1 | (n = 46) 7598 ± 3345 | (n = 59) 7564 ± 3838 | 0.961 |
| Week 2 | (n = 51) 9130 ± 3042 | (n = 60) 9300 ± 4187 | 0.806 |
| Week 3 | (n = 58) 8880 ± 3494 | (n = 58) 8057 ± 3683 | 0.220 |
| Week 4 | (n = 49) 9026 ± 2860 | (n = 54) 9287 ± 4237 | 0.712 |
| Week 5 | (n = 48) 8969 ± 3561 | (n = 49) 9479 ± 4259 | 0.523 |
| Week 6 | (n = 49) 8732 ± 3008 | (n = 53) 9459 ± 3941 | 0.295 |
| Week 7 | (n = 48) 9147 ± 3705 | (n = 53) 8953 ± 4162 | 0.805 |
| Week 8 | (n = 52)8550 ± 3095 | (n = 59)9447 ± 4095 | 0.193 |
| Week 9 | (n = 57) 9154 ± 3253 | (n = 59) 9635 ± 3616 | 0.452 |
| Week 10 | (n = 58) 9924 ± 3676 | (n = 63) 10,079 ± 3930 | 0.823 |
| Week 11 | (n = 54) 10,098 ± 3752 | (n = 61) 10,329 ± 3958 | 0.749 |
| Week 12 | (n = 48) 9008 ± 4110 | (n = 53) 8048 ± 4162 | 0.244 |
| Week 13 | (n = 51) 8240 ± 4297 | (n = 50) 6474 ± 3468 | 0.025∗ |
| Weekday | 8409 ± 4143 | 6417 ± 3442 | 0.015∗ |
| Weekend | 8338 ± 4830 | 7540 ± 4161 | 0.427 |
| Week 14 | (n = 61) 10,005 ± 4544 | (n = 43) 7569 ± 4742 | 0.010∗ |
| Weekday | 10,657 ± 4404 | 7362 ± 4419 | 0.001∗ |
| Weekend | 9239 ± 5298 | 8508 ± 8801 | 0.608 |
Results are reported as n (%) or mean ± SD. Weeks run Monday to Sunday. Week 1 in 2019 began on December 31, 2018, and in 2020 on December 30, 2019.
Significant difference.
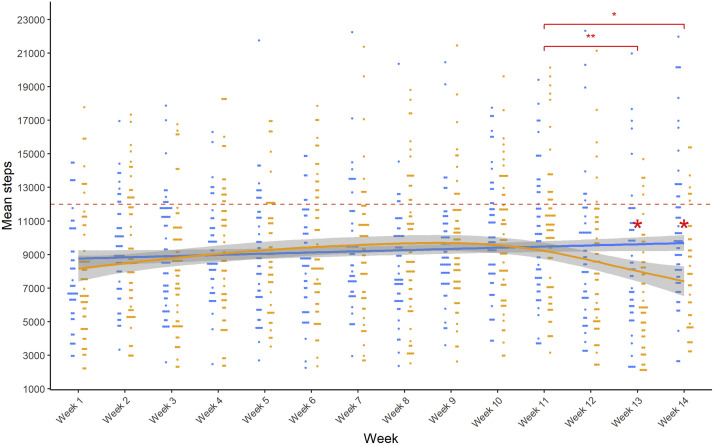
In both 2019 and 2020 there was a slight trend toward increasing step counts from January through early March (Fig. 1 ). Step counts in matched weeks were not significantly different between the groups until the last week of March (week 13; P = 0.025) and the first week of April (week 14; P = 0.010); both were significantly lower in 2020 (Table 1; Fig. 1). Weekday mean step counts differed from 2019 to 2020 (P = 0.015 [week 13] and P = 0.001 [week 14]), although weekends did not (P = 0.427 [week 13] and P = 0.608 [week 14]).
Figure 1.
Weekly Fitbit step counts in 2019 and 2020. Weeks run Monday to Sunday. Week 1 in 2019 began on December 31, 2018, and in 2020 on December 30, 2019. Dots (blue = 2019; orange = 2020) indicate individual participants’ weekly average step counts, lines show the line of best fit for each year, and shading indicates the standard error. The red dashed line indicates 12,000 steps, which approximates the Canadian physical activity guidelines (60 minutes per day of moderate-to-vigorous physical activity).9,10 Weekly step counts were significantly lower in 2020 than in 2019 in weeks 13 (March 23-29, 2020; P = 0.03) and 14 (March 30-April 5, 2020; P = 0.01). Weekly step counts for weeks 13 (P < 0.001) and 14 (P = 0.02) in 2020 were also lower than week 11 (March 9-15, 2020) of the same year. ∗P < 0.05; ∗∗P < 0.001.
All mean step counts were < 12,000 (Canadian physical activity guidelines equivalent) in both 2019 and 2020.9 , 10 Boys had higher step counts than girls; no significant time-sex interactions were observed (Supplemental Fig. 1).
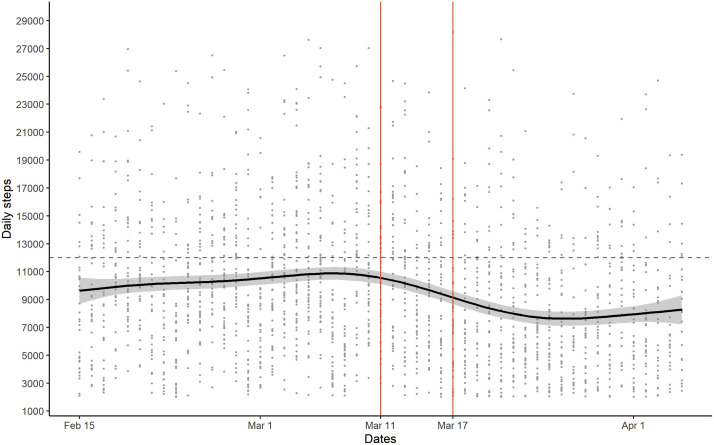
In 2020, step counts began to decrease around March 11, when the World Health Organisation declared the COVID-19 outbreak a pandemic (Fig. 2 ). A significant reduction in step counts occurred from the week of March 9 (week 11; 10,329 ± 3958 steps) to the weeks of March 23 (week 13, 6474 ± 3468 steps; P < 0.001) and March 30 (week 14, 7569 ± 4742 steps; P = 0.021). This significant decline occurred after British Columbia’s declaration of a public health emergency, implementation of 2-metre physical distancing, and suspension of K-12 schools (March 17). It began during Spring Break (March 16-27 for most BC schools), and persisted into week 14.
Figure 2.
Daily Fitbit step counts and important COVID-19–related dates in 2020. Dots indicate individual participants’ daily step count, the black line shows the line of best fit, and shading indicates the standard error. The blue dashed line indicates 12,000 steps, which approximates the Canadian physical activity guidelines (60 minutes per day of moderate-to-vigorous physical activity).9,10 The vertical red lines show important dates related to COVID-19: March 11, World Health Organisation declared pandemic; March 17, British Columbia declared a public health emergency, ordered physical distancing, and suspended K-12 schools.
Discussion
During the early phase of the COVID-19 pandemic in Canada, children with CHD had a decline of 21%-24% of their overall daily step counts. This reduction was likely due to COVID-19 measures and not Spring Break. Step counts during weeks 12 and 13 (corresponding to Spring Break in both 2019 and 2020) were reduced in 2020 only, and this reduction persisted into April. Step counts throughout the study period were < 12,000 per day (approximation of the Canadian physical activity guidelines).9 , 10 This was unsurprising given that only one-third of Canadian children, and only 25% of those with CHD, meet the guidelines.11 , 12 Therefore, reduced physical activity due to COVID-19 may not have severe long-term health impacts if the implemented measures to prevent a catastrophic pandemic are reasonably brief. However, it will be important to understand and model the long-term impact of significantly reduced physical activity on health for these patients should the present approach need to be maintained for months, as indicated by Prime Minister Trudeau on April 8, 2020.13 These children are already at increased cardiovascular risk and physical inactivity which has many other negative health consequences (eg, bone health, motor skill development, body composition) that warrant consideration when making future public health decisions.4 , 14 The impact of reduced physical activity on this population will depend on the duration of measures and the magnitude of reduction, so careful monitoring is required.
In addition to potential negative impacts on physical and cardiovascular health in this already at-risk population, mental health impacts of reduced physical activity must be considered. Physical activity is an important coping mechanism during the significant disruptions to normal routine caused by COVID-19.6 In children with CHD, this is particularly important, because they may have already had lower quality of life than their healthy peers before COVID-19, and physical activity has been associated with quality of life in children with CHD.15 , 16 Therefore, it is necessary to evaluate the change in physical activity patterns due to COVID-19 and their potential long-term impacts on both the physical and the mental health of this high-risk cardiac population.
Moving forward, it will be important to consider how these children and their families may adapt to the public health precautions and resume higher levels of physical activity. If this is possible, or could be with appropriate intervention, then long-term negative health impacts due to reduced physical activity could be avoided. From January through early March 2019 and 2020, step counts are similar and increasing. Later in March 2020, step counts were significantly lower than in 2019, despite seasonal match between the cohorts. It appears that this reduction was driven by reduced weekday step counts, likely reflecting COVID-19–related disruptions to parents’ and children’s routines (work, school, extracurricular activities). Week 14 step counts, though still lower than 2019, suggest a slight increase in physical activity from the previous week, which may reflect expected springtime increase in physical activity or adaptive measures taken by families as COVID-19 measures continued.17 The objective measurement of physical activity in this study provides the basis for future investigation of the long-term impacts of reduced physical activity during COVID-19 and how best to mitigate these. It will provide baseline data to investigate the necessity and effectiveness of supports for physical activity during and after the pandemic. This may provide an opportunity to assist children with CHD and their families in developing life-long physical activity habits that are less reliant on external factors (eg, school, extracurricular physical activities), which are currently cancelled but normally contribute to physical activity levels in school-age children.18 Physical activity monitoring throughout the COVID-19 pandemic and after will permit better understanding of the adaptability of children with CHD and their families, and may help generate and test hypotheses about individual- and family-based physical activity interventions.
To our knowledge, this is the first study to report change in objectively measured physical activity in response to COVID-19 and associated precautions. A key strength of this study is the longitudinal data capture enabled by using Fitbits and the comparison data from both 2019 and early 2020. The main limitation to the study is that we used a single method to quantify physical activity and as such it is limited to only physical activity patterns indicated by step counts, which do not reflect physical activity mode or intensity. A second limitation is the lack of healthy control comparison data, which were unavailable owing to the nature of the ongoing cohort study limited to children with CHD. Therefore, the generalizability of these data to healthy children may be limited.
This study provides important objective physical activity data in children with CHD, which will allow for future modelling of the potential impacts of COVID-19 on physical activity, and subsequently health, depending on the duration and nature of public health measures going forward. Future studies will be needed to model these impacts and explore potential strategies for mitigation. Continuous physical activity monitoring data during this pandemic provides unique insight about the impact of COVID-19 and public health precautions on daily habits of children with CHD, which will hopefully inform clinicians about potential health impacts and help in developing interventions if necessary, both during the pandemic and in the future.
Conclusion
There is a paucity of pediatric COVID-19 data, specifically among children with underlying medical conditions, including CHD. Clinicians, policy makers, and other stakeholders need to consider the potential long-term and indirect health impacts of public health precautions in response to COVID-19. Children with CHD have significantly reduced physical activity compared with before the pandemic. The short- and long-term health impacts of this cardiovascular risk behaviour change have not yet been elucidated and are in part dependent on the duration of the health measures and any action taken to mitigate the adverse effects of these measures.
Acknowledgements
The authors thanks the participants in this study and their families, as well as the clinical staff of the Children’s Heart Centre who make clinically integrated research recruitment possible.
Funding Sources
This project was supported by a Grant-in-Aid from Heart & Stroke Canada (grant no. G-17-0018284).
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 1134 for disclosure information.
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at https://doi.org/10.1016/j.cjca.2020.04.038.
Supplementary Material
Supplemental Figure S1. Daily Fitbit step counts for male and female participants, and important COVID-19–related dates in 2020. Dots indicate individual participants’ daily step count (blue = male, orange = female), the lines show the lines of best fit for male (blue) and female (orange) participants, and shading indicates the standard error. The blue dashed line indicates 12,000 steps, which approximates the Canadian physical activity guidelines (60 minutes per day of moderate-to-vigorous physical activity). 9,10The vertical red lines show important dates related to COVID-19: March 11, World Health Organization declared pandemic; March 17, British Columbia declared a public health emergency, ordered physical distancing, and suspended K-12 schools.
References
- 1.Centers for Disease Control and Prevention COVID-19 Response Team Coronavirus disease 2019 in children—United States, February 12–April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouma B.J., Mulder B.J.M. Changing landscape of congenital heart disease. Circ Res. 2017;120:908–922. doi: 10.1161/CIRCRESAHA.116.309302. [DOI] [PubMed] [Google Scholar]
- 3.Kavey R.-E.W., Allada V., Daniels S.R., et al. Cardiovascular risk reduction in high-risk pediatric patients. Circulation. 2006;114:2710–2738. doi: 10.1161/CIRCULATIONAHA.106.179568. [DOI] [PubMed] [Google Scholar]
- 4.Longmuir P.E., Brothers J.A., de Ferranti S.D., et al. Promotion of physical activity for children and adults with congenital heart disease. Circulation. 2013;127:2147–2159. doi: 10.1161/CIR.0b013e318293688f. [DOI] [PubMed] [Google Scholar]
- 5.Chen P., Mao L., Nassis G.P., et al. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9:103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiménez-Pavón D., Carbonell-Baeza A., Lavie C.J. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog Cardiovasc Dis. 2020;63:386–388. doi: 10.1016/j.pcad.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris P.A., Taylor R., Thielke R., et al. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voss C., Gardner R.F., Dean P.H., Harris K.C. Validity of commercial activity trackers in children with congenital heart disease. Can J Cardiol. 2017;33:799–805. doi: 10.1016/j.cjca.2016.11.024. [DOI] [PubMed] [Google Scholar]
- 10.Colley R.C., Janssen I., Tremblay M.S. Daily step target to measure adherence to physical activity guidelines in children. Med Sci Sports Exerc. 2012;44:977–982. doi: 10.1249/MSS.0b013e31823f23b1. [DOI] [PubMed] [Google Scholar]
- 11.Colley R.C., Carson V., Garriguet D., Janssen I., Roberts K.C., Tremblay M.S. Physical activity of Canadian children and youth 2007 to 2015. Health Rep. 2017;28:8–16. [PubMed] [Google Scholar]
- 12.Lopez JR, Voss C, Kuan MTY, et al. Physical activity is associated with better vascular function in children and adolescents with congenital heart disease. Can J Cardiol 36:1474-81. [DOI] [PubMed]
- 13.Chase S., Perreaux L. Return to work will be graduated and likely months off, Trudeau says. The Globe and Mail. April 8, 2020 https://www.theglobeandmail.com/politics/article-return-to-work-will-be-graduated-and-likely-months-off-trudeau-says/ Available at: [Google Scholar]
- 14.Poitras V.J., Gray C.E., Janssen X., et al. Systematic review of the relationships between sedentary behaviour and health indicators in the early years (0-4 years) BMC Public Health. 2017;17:868. doi: 10.1186/s12889-017-4849-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mellion K., Uzark K., Cassedy A., et al. Health-related quality of life outcomes in children and adolescents with congenital heart disease. J Pediatr. 2014;164:781–788.e1. doi: 10.1016/j.jpeds.2013.11.066. [DOI] [PubMed] [Google Scholar]
- 16.Dean P.N., Gillespie C.W., Greene E.A., et al. Sports participation and quality of life in adolescents and young adults with congenital heart disease. Congenit Heart Dis. 2015;10:169–179. doi: 10.1111/chd.12221. [DOI] [PubMed] [Google Scholar]
- 17.Kuan M.T.Y., Voss C., Lopez J., Hemphill N.M., Harris K.C. Capturing seasonality in physical activity with commercial physical activity tracker, accelerometer, and questionnaire in children with congenital heart disease. Appl Physiol Nutr Metab. 2019;44:S85. [Google Scholar]
- 18.Ridgers N.D., Stratton G., Fairclough S.J. Physical activity levels of Hungarian children during school recess. Sport Med. 2006;36:359–371. doi: 10.2165/00007256-200636040-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1. Daily Fitbit step counts for male and female participants, and important COVID-19–related dates in 2020. Dots indicate individual participants’ daily step count (blue = male, orange = female), the lines show the lines of best fit for male (blue) and female (orange) participants, and shading indicates the standard error. The blue dashed line indicates 12,000 steps, which approximates the Canadian physical activity guidelines (60 minutes per day of moderate-to-vigorous physical activity). 9,10The vertical red lines show important dates related to COVID-19: March 11, World Health Organization declared pandemic; March 17, British Columbia declared a public health emergency, ordered physical distancing, and suspended K-12 schools.