The coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus -2 (SARS-CoV-2), originated in China and rapidly spread across the world, causing a pandemic.1 The well-recognized symptoms of COVID-19 include fever, cough, dyspnea, sputum production, myalgia, arthralgia, headache, diarrhea, nausea/vomiting, and sore throat. It appears that a subset of patients with COVID-19 also develop other symptoms, such as ageusia/dysgeusia.2 We performed a systematic review of the available literature to assess the presence of ageusia/dysgeusia among patients with COVID-19.
Methods
We performed a systematic review of the databases PubMed/Medline, Embase, Cochrane, and Web of Science from January 1 to April 21, 2020, to identify relevant articles reporting ageusia/dysgeusia as a symptom in patients with laboratory-confirmed COVID-19. Relevant articles reporting data on ageusia/dysgeusia in the form of case series, case-control, and cohort studies were included. Studies were excluded if they did not report the symptoms of interest, that is, ageusia/dysgeusia. Pooled analysis (where applicable) was performed using a random-effects model and DerSimonian-Laird approach. Study heterogeneity was assessed using the I 2 statistic.
Results
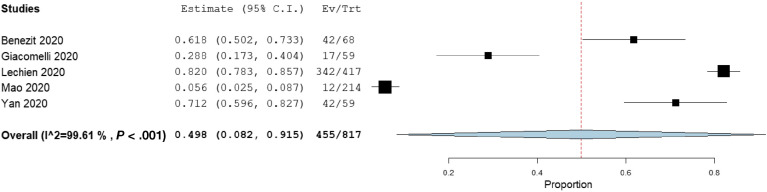
The initial search yielded a total of 33 articles, and after screening for duplicates and excluding irrelevant articles, a total of 5 studies with 817 patients were finally included.2, 3, 4, 5, 6 Four of these studies were single-nation studies, and 1 study was a multinational study from Europe. The study period ranged from January 16, 2020, to March 29, 2020. The proportion of female patients was reported in 3 studies (60.7%, 95% confidence interval 51.3%–70.1%). We found the prevalence of ageusia/dysgeusia was 49.8% (95% confidence interval 8.2%–91.5%, I 2 = 99.6%) across these 5 studies (Figure 1 ).
Figure 1.
Forrest plot demonstrating the pooled prevalence of ageusia/dysgeusia in patients with COVID-19. C.I., confidence interval; Ev/Trt, patients with symptoms/total patients.
Discussion
In our pooled analysis, almost half of the patients (49.8%) with COVID-19 have altered taste sensation. Taste disorders are well known to be related to a wide variety of viral illnesses.7 The suggested mechanism of SARS-CoV-2 causing altered taste is its ability to bind to angiotensin-converting enzyme-2 receptor, which is readily expressed on multiple organ systems, including the surface of the tongue and oral cavity. The oral cavity can act as a gateway to infection and lead to the development of ageusia/dysgeusia.8 Given the lack of access to diagnostic tests for COVID-19, particularly in the developing world, the utility of distinctive clinical features (such as ageusia/dysgeusia) in identifying patients with suspected COVID-19 is of paramount significance.
Reporting of gustatory and olfactory disturbances is subjective in nature, and patients with COVID-19 (without a history of ear, nose, and throat disorders) should be actively evaluated for these symptoms at presentation. Our study has multiple limitations. First, there is a lack of data comparing ageusia/dysgeusia in laboratory-confirmed COVID-19–positive and –negative patients. Only one study, by Bénézit et al,2 compared the prevalence of altered taste in COVID-19–positive and –negative patients who underwent testing based on suspicion.2 A significantly increased proportion of patients reported ageusia/dysgeusia (62% vs 11%, odds ratio 7.4, P < .01) in the COVID-19–positive arm.2 There was also a lack of studies reporting an association of ageusia/dysgeusia with severe COVID-19. Mao et al5 also compared the presence of altered taste sensations in severe and nonsevere COVID-19 cases. A somewhat lower prevalence of ageusia/dysgeusia was seen in severe cases and was not statistically significant (P = .24).
Second, the inclusion of observational studies can undoubtedly lead to several biases, including but not limited to selection bias, information bias, recall bias, and confounding bias. Third, no study reported the association of acute respiratory distress syndrome, mortality, intensive care unit admission, need for a ventilator, and length of intensive care unit stay with ageusia/dysgeusia. Significant heterogeneity was noted in our analysis of prevalence. This is likely because of the reason mentioned previously, that is, the observational nature of the study. The data were retrospectively collected from medical files, and the presence of ageusia/dysgeusia might have been underestimated. Fourth, the presence of these symptoms may not be reported in the presence of other severe symptoms, such as dyspnea, fever, and productive cough. For these reasons, the true prevalence of ageusia/dysgeusia might be significantly higher (than reported in our analysis) and should be included as a screening question for patients evaluated for suspected COVID-19.
Currently, there is weak evidence if the taste or smell changes could prognosticate COVID-19–related severity and mortality. More epidemiological studies are needed to assess the prevalence of ageusia/dysgeusia in patients with COVID-19, as well as comparing mild to moderate and severe cases. Recognizing these distinctive clinical features can raise the suspicion of COVID-19, leading to early testing and diagnosis of the disease.
CRediT Authorship Contributions
Muhammad Aziz, MD (Formal analysis: Lead; Writing – original draft: Equal). Abhilash Perisetti, MD FACP (Writing – review & editing: Equal). Wade M. Lee-Smith, MLS, BS (Data curation: Lead). Mahesh Gajendran, MD, MPH, FACP (Writing – review & editing: Equal). Pardeep Bansal, MD FACG (Writing – review & editing: Supporting). Hemant Goyal, MBBS, MD, FACP (Conceptualization: Lead; Writing – review & editing: Lead).
Footnotes
Conflict of interest The authors disclose no conflicts.
Author names in bold designate shared co-first authorship.
References
- 1.World Health Organization https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ Available at:
- 2.Bénézit F. Published online ahead of print April 15, 2020. Lancet Infect Dis. 10.1016/S1473-3099(20)30297-8
- 3.Giacomelli A. Clin Infect Dis. 2020;71:889–890. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lechien J.R. Eur Arch Otorhinolaryngol. 2020;277:2251–2261. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mao L. JAMA Neurol. 2020;77:1–9. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan C.H. Int Forum Allergy Rhinol. 2020;10:806–813. doi: 10.1002/alr.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang H. Ann N Y Acad Sci. 2009;1170:596. doi: 10.1111/j.1749-6632.2009.04480.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu H. Int J Oral Sci. 2020;12:1–5. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]