Food protein–induced enterocolitis syndrome (FPIES) is a non–immunoglobulin E (IgE)–mediated food allergy that manifests with predominantly gastrointestinal symptoms characterized by repetitive emesis starting 1 to 4 hours (typically 2 hours) after food ingestion with or without watery diarrhea that may follow within 6 to 10 hours.1 It usually starts in the first year of life; the most commonly reported triggers of FPIES in infants include cow’s milk, soy, rice, and oat, followed by fruits, vegetables, egg, and fish (in Mediterranean countries). In adults, seafood is a common trigger.
Although FPIES is traditionally regarded as a rare food allergy, a recent population-based study estimated the prevalence in the United States as 0.51% in people younger than 18 years, which is in line with previously reported cumulative incidence rates of FPIES in infancy between 0.34% (Israel) and 0.7% (Spain).2
In addition, FPIES can be associated with systemic manifestations such as lethargy, hypotension, and hypovolemic shock. Because of the potential for severe symptoms, acute FPIES is recognized as a medical emergency that may require prompt management with intravenous fluids, antiemetics, and anti-inflammatories (eg, methylprednisolone) in the medical setting. Rarely, life support including intubation, ventilation, and vasopressors may be necessary. Under regular circumstances, acute FPIES reactions are preferably managed in the medical facility unless symptoms are mild and the patient can be effectively monitored and rehydrated at home.1
The unprecedented circumstances of the coronavirus disease 2019 (COVID-19) pandemic present unique challenges for patients with food allergy, including FPIES.2 The risk of exposure to COVID-19 in a potentially overcrowded emergency department demands modification of existing practices to balance the risk and benefits of treatment in the setting of a high likelihood of extended wait times for care.
The members of the medical advisory board of the International FPIES Association are providing expert, opinion-based, consensus recommendations for managing FPIES during the COVID-19 pandemic.
Modified Protocol for Managing Food Protein–Induced Enterocolitis Syndrome Emergencies
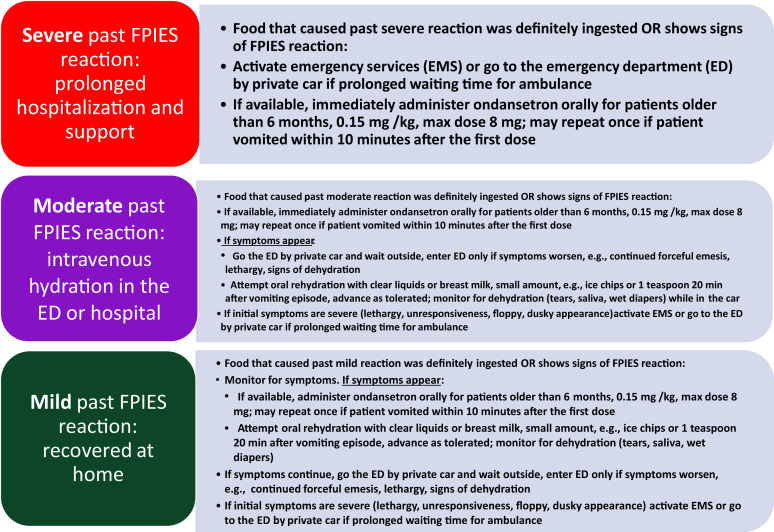
The recommendations for modifying the management of acute FPIES reactions are shown in Figure 1 . The implementation of these recommendations will vary based on the local circumstances and access to care owing to the COVID-19 burden. For patients with past severe reactions, it is prudent to proactively discuss management through telemedicine, if feasible.
Figure 1.
Modified management algorithm for acute food protein–induced enterocolitis syndrome during the coronavirus disease 2019 pandemic stratified by the severity of the past reactions. The contact number to activate emergency medical services is 911 in the United States and Canada; 999 in the United Kingdom; 112 in the countries of the European Union; and 119 in Japan and South Korea.
For patients with FPIES who are older than 6 months, with no known cardiac problems, and no family history of syncope suggestive of prolonged QT syndrome, consider providing a prescription for oral ondansetron to be used at home in case of an acute reaction. Ondansetron is a serotonin 5-HT receptor antagonist indicated for the prevention and treatment of chemotherapy-induced nausea and emesis in patients older than 6 months. It is available in oral forms as a tablet, rapidly disintegrating tablet, oral film, and liquid. Ondansetron is recognized to be associated with prolongation of the QT interval on electrocardiogram, but is considered safe and is widely used in pediatric emergency departments to symptomatically manage emesis. There is limited experience with ondansetron in FPIES, suggesting that it may be useful in alleviating emesis in mild to moderate acute FPIES reactions.3 , 4 Controlled trials using ondansetron for FPIES-induced emesis and comparison of the parenteral vs enteral route are lacking. Although current data suggest that intravenous and intramuscular ondansetron forms have better efficacy, it is impractical in the home setting. The dose of ondansetron is 0.15 mg/kg, with a maximum dose of 8 mg. The dose may be repeated once if patient vomits within 10 minutes after the first dose (Figure 1).
The approach to managing present FPIES reactions is influenced by the severity of the past reactions, as depicted in Figure 1. The patients and or caregivers might attempt to contact their physician on an urgent basis; however, access to their physician may be limited during the COVID-19 pandemic.
Introduction of New Foods
It is prudent to delay the introduction of new high-risk foods until the COVID-19 pandemic resolves to minimize the risk of acute FPIES reactions, particularly in patients with moderate to severe FPIES or those with multiple food FPIES. Caregivers should discuss with their physician whether food introduction can be continued. In the case of exclusively breastfed or formula-fed young infants, when the time window of the preferred introduction of solid foods is closing, the introduction should be done cautiously over a longer-than-usual period (eg, 5-10 days), starting from a very small amount, then doubling this amount with every feeding given twice daily until full serving is reached. The caregivers should be educated to discontinue the introduction if gastrointestinal symptoms appear, such as diarrhea, intermittent vomiting, or increased gastroesophageal reflux, and to contact their physician to discuss whether food introduction should be continued. Foods with the lowest risk, such as vegetables (eg, broccoli, cauliflower, parsnip) should be chosen during the introduction.1 The goal should be to introduce 1 or 2 different foods and serve them in various forms and textures. For patients with mild FPIES or single-food FPIES who have already been introduced to several foods, a careful discussion with caregivers is warranted regarding the following: (1) their preferences for new foods, (2) establishment of a protocol for the slow introduction, and (2) layout of a contingency plan in the event of an adverse reaction.
Evaluation for Resolution of Food Protein–Induced Enterocolitis Syndrome
Evaluation for resolution of FPIES through oral food challenge should be deferred until the COVID-19 pandemic resolves to minimize the risk of acute reactions.
Atypical Food Protein–Induced Enterocolitis Syndrome
Patients with detectable food-specific IgE antibody through skin prick test or serologic measurement are referred to as atypical FPIES. Most of these patients exhibit classic FPIES symptoms during reactions but a small subset might transition to immediate symptoms such as hives, skin rashes, or very rarely, anaphylaxis. Depending on the physician’s assessment of the likelihood of an immediate IgE-mediated reaction, emergency medications may be prescribed and management of anaphylaxis can be discussed proactively.2
Managing Comorbidities
Patients with FPIES have high rates of allergic comorbidities, including IgE-mediated food allergy to foods other than FPIES triggers, asthma, atopic dermatitis, allergic rhinitis, and eosinophilic esophagitis.5 It is important to maintain optimal control of these comorbid conditions during the COVID-19 pandemic.
Resources for the Patients and Caregivers
Even under normal circumstances, FPIES poses a great burden for the patients and caregivers. To address the added stress of the COVID-19 pandemic, the limited access and supply of safe foods, and anxiety from potential reactions, the International FPIES Association website (www. fpies.org) provides valuable advice for the day-to-day management of FPIES and can be used as an important educational resource to complement medical management of FPIES.
In summary, effective management of FPIES during the COVID-19 pandemic requires modification of the existing treatment paradigm to minimize the need for emergency department intervention and reduce the risk of acquiring COVID-19.
Acknowledgments
The authors thank Fallon Schultz-Matney, MSW, LCSW, CAM, the founder and chief executive officer of the International Food Protein–Induced Enterocolitis Syndrome Association and the following members of the Medical Advisory Board of the International Food Protein–Induced Enterocolitis Syndrome Association for their helpful feedback: Stefania Arasi, MD; Ashis V Barad, MD; Theresa Bingemann, MD; Terri Brown-Whitehorn, MD; Raquel Durban, MS, RD, LD/N; Todd Green, MD; George Konstantinou, MD; Stephanie Leonard, MD; Jennifer Lightdale, MD; Antonella Muraro, MD, PhD; Ichiro Nomura, MD, PhD; Jonathan Spergel, MD, PhD; and Carina Venter, RD, PhD.
Footnotes
Disclosures: Dr Nowak-Wegrzyn reports to have received research support from the National Institute of Allergy and Infectious Diseases, DBV Technologies, Astellas Pharma, and Danone and Nestle; received consultancy fees from Regeneron and Gerber Institute; serves as the deputy editor for the Annals of Allergy, Asthma, and Immunology; and serves as Chair of the Medical Advisory Board of the International Food Protein–Induced Enterocolitis Syndrome Association. Dr Fiocchi reports receiving research support from Danone, Sanofi, Hipp, Ferrero, and Galbusera S.p.A.; and has served on advisory boards for Danone, Stallergenes, Abbott, DBV, Novartis, Hipp, and International Food Protein–Induced Enterocolitis Syndrome Association. Dr Bird reports receiving research support from National Institute of Health–National Institute of Allergy and Infectious Diseases, Genentech, Food Allergy Research and Education, Aimmune Therapeutics, Astellas, and DBV Technologies; and has served on advisory boards for AllerGenis, Prota Therapeutics, and Food Allergy Research and Education. The remaining authors have no conflicts of interest to report.
Funding: The authors have no funding sources to report.
Contributor Information
Anna Nowak-Wegrzyn, Email: anna.nowak-wegrzyn@nyulangone.org.
Medical Advisory Board of the International FPIES Association:
Stefania Arasi, Ashis V. Barad, Theresa Bingemann, Terri Brown-Whitehorn, Raquel Durban, Todd Green, George Konstantinou, Stephanie Leonard, Jennifer Lightdale, Antonella Muraro, Ichiro Nomura, Jonathan Spergel, and Carina Venter
References
- 1.Nowak-Wegrzyn A., Chehade M., Groetch M.E. International consensus guidelines for the diagnosis and management of food protein-induced enterocolitis syndrome: executive summary-workgroup report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol. 2017;139(4):1111–1126.e4. doi: 10.1016/j.jaci.2016.12.966. [DOI] [PubMed] [Google Scholar]
- 2.Nowak-Wegrzyn A., Warren C.M., Brown-Whitehorn T., Cianferoni A., Schultz-Matney F., Gupta R.S. Food protein-induced enterocolitis syndrome in the US-population-based study. J Allergy Clin Immunol. 2019;144(4):1128–1130. doi: 10.1016/j.jaci.2019.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blackman A.C., Anvari S., Davis C.M., Anagnostou A. Emerging triggers of food protein-induced enterocolitis syndrome: lessons from a pediatric cohort of 74 children in the United States. Ann Allergy Asthma Immunol. 2019;122(4):407–411. doi: 10.1016/j.anai.2019.01.022. [DOI] [PubMed] [Google Scholar]
- 4.Miceli Sopo S., Bersani G., Monaco C. Ondansetron in acute food protein-induced enterocolitis syndrome, a retrospective case-control study. Allergy. 2017;72(4):545–551. doi: 10.1111/all.13033. [DOI] [PubMed] [Google Scholar]
- 5.Cianferoni A., Warren C.M., Brown-Whitehorn T., Schultz-Matney F., Nowak-Wegrzyn A., Gupta R.S. Eosinophilic esophagitis and allergic comorbidities in a US-population-based study [e-pub ahead of print]. Allergy. https://doi.org/10.1111/all.14148 accessed May 9, 2020. [DOI] [PMC free article] [PubMed]