Clinical Implications.
-
•
Several cutaneous manifestations have been recently linked to coronavirus disease 2019. We report a case of urticaria with angioedema in a coronavirus disease 2019–affected patient.
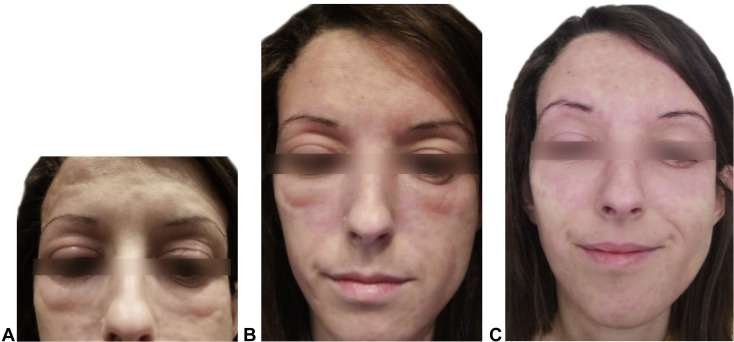
This is the case of a 30-year-old female physician with no relevant past medical history except for pine seeds allergy, following a strict nut-free diet since she was diagnosed. Lipid transfer protein syndrome was ruled out at diagnosis. She did not have a family history of hereditary angioedema, and she was not on any medication. In March 2020, she presented with symptoms of odynophagia and dry cough, with rapid onset of fever. The day after the symptoms appeared, a PCR of upper-airway secretions (by nasopharyngeal swab) was performed, revealing severe acute respiratory syndrome coronavirus 2 infection. With this positive result, she was instructed to remain in strict home isolation. She evolved satisfactorily, with 4 days of fever and dry cough, followed by 5 days of total anosmia and ageusia from which she completely recovered. On day +11 of disease evolution, after resolution of the previous symptoms, rapidly spreading wheals developed in various locations on her body: face, trunk, abdomen, and limbs. In a few hours, face wheals promptly converted to facial angioedema (Figure 1 ), with preferential involvement of periocular region and mild edema of the lips, without compromise of the tongue, uvula, vocal cords, or the airway. No other symptoms were noted. The appearance of the lesions was not related to food intake (she had not eaten nuts). She had not taken nonsteroidal inflammatory drugs or angiotensin-converting enzyme inhibitors the previous 15 days. She had not exercised, had not drunk alcohol, nor was on menstrual period. As symptomatic treatment, only an antihistamine was taken (ebastine 10 mg ter in die). Twenty-four hours after the onset of the cutaneous symptoms, both the wheals and angioedema started to fade off, turning into erythematous macules until complete resolution. From there on, she remained asymptomatic. On day +15, upper-airway secretion PCR was performed again, persisting still positive for severe acute respiratory syndrome coronavirus 2 and therefore proving the presence of this virus in the respiratory tract. After 7 more days of home isolation, repeated PCR on day +22 was finally negative.
Figure 1.
(A) The first stages of acute urticaria: wheals at the forehead and cheeks, as well as incipient periorbital edema. (B) Evolution of this manifestation, showing fading of wheals and apparent periorbital edema. (C) Last stage of evolution, 24 hours after the onset, where periorbital edema has disappeared and erythematous macules are visible.
Coronavirus disease 2019 (COVID-19) is one of the greatest challenges that the health sector and the entire population have had to face in recent decades.
Its high contagiousness (transmission rate or R0 of 2.24-3.58)1 has led to its rapid expansion worldwide, with more than 2.7 million cases from December 2019 to date.2
The symptoms and syndromes caused by this disease are diverse. The most frequent symptoms are fever, cough, dyspnea, as well as fatigue and malaise.3 Diarrhea, anosmia, and ageusia have also been described. Furthermore, this disease can cause severe syndromes such as pneumonia, respiratory distress syndrome, multiple organ failure secondary to sepsis, and death.3
There is only 1 study describing cutaneous manifestations of COVID-19 so far. This recently published work was carried out in a hospital of Lombardy region, Italy, and studied 88 patients affected by coronavirus infection who had not taken any new drug in the previous 15 days. Of these 88 patients, 18 patients (20.4%) developed cutaneous manifestations. These were erythematous rash (14 patients, 16%), widespread urticaria (3 patients, 3.4%), and chickenpox-like vesicles (1 patient, 1.1%).4 Unfortunately, no pictures were taken because of the high risk of infection to other patients with the use of a photographic device.
We report a new case of acute urticaria (AU) in the setting of COVID-19, including both wheals and angioedema and provide, for the first time, clinical images of skin manifestations of COVID-19.
Although the percentage of AU cases recorded so far appears to be low, it is not surprising that these clinical manifestations can occur. The relationship between AU and a viral infection has been well established.5 To safely set this diagnosis, it is important to rule out other underlying causes such as medication or unusual food intake. Herpesviridae (specially cytomegalovirus and EBV), rhinovirus, and hepatitis A, B, and C viruses are the most frequent virus families involved in causing AU.5 Nevertheless, no cases of AU with angioedema had been related to Coronaviridae family before. Multiple mechanisms have been hypothesized to be the trigger of this AU and angioedema type 1 hypersensitivity reaction, most of them leading to an increase in vascular permeability; some authors have proposed a cross-reaction between viral IgM and IgG, with mast cell IgE favoring mast cell degranulation,6 whereas other groups defend that circulating immune complexes stimulate the production of vasoactive amines by basophils and activate complement.7 Coronavirus infection (regardless of the various types of coronavirus) is primarily attacked by immune cells, including mast cells, which are located in the submucosa of the respiratory tract and in the nasal cavity, and represent a barrier of protection against microorganisms. Viral-activated mast cells release inflammatory chemical compounds including protease, ILs such as IL-1, IL-6, or IL-33, and histamine.8 This histamine release may lead to urticaria and angioedema, as occurred in this case. However, the exact role of this infection in the development of urticaria is not clear and will need further studies.
Footnotes
Conflicts of interest: The authors declare that they have no relevant conflicts of interest.
Informed consent: The patient gave written informed consent for publication (both clinical information and images).
References
- 1.Zhao S., Lin Q., Ran J., Musa S.S., Yang G., Wang W. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214–217. doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometer Coronavirus update (live): 2,766,180 cases and 193,777 deaths from COVID-19 virus pandemic. https://www.worldometers.info/coronavirus/ Available from:
- 3.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls Publishing; Treasure Island, FL: 2020. Features, evaluation and treatment coronavirus (COVID-19) [PubMed] [Google Scholar]
- 4.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 5.Imbalzano E., Casciaro M., Quartuccio S., Minciullo P.L., Cascio A., Calapai G. Association between urticaria and virus infections: a systematic review. Allergy Asthma Proc. 2016;37:18–22. doi: 10.2500/aap.2016.37.3915. [DOI] [PubMed] [Google Scholar]
- 6.Arias-Santiago S.A., Almazán-Fernández F.M., Burkhardt-Pérez P., Naranjo-Sintes R. [Cold urticaria associated with Epstein barr virus mononucleosis] Actas Dermosifiliogr. 2009;100:435–436. doi: 10.1016/s0001-7310(09)71265-7. [DOI] [PubMed] [Google Scholar]
- 7.Leiste A., Skaletz-Rorowski A., Venten I., Altmeyer P., Brockmeyer N.H. Urticaria associated with norovirus infection: report of two cases. J Dtsch Dermatol Ges. 2008;6:563–565. doi: 10.1111/j.1610-0387.2007.06501.x. [DOI] [PubMed] [Google Scholar]
- 8.Kritas S.K., Ronconi G., Caraffa A., Gallenga C.E., Ross R., Conti P. Mast cells contribute to coronavirus-induced inflammation: new anti-inflammatory strategy. [published online ahead of print February 4, 2020] J Biol Regul Homeost Agents. [DOI] [PubMed]