Abstract
Coronavirus Disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread worldwide. During the ongoing COVID-19 epidemic, most hospitals have postponed elective surgeries. However, some emergency surgeries, especially for trauma patients, are inevitable. For patients with suspected or confirmed COVID-19, a standard protocol addressing preoperative preparation, intraoperative management, and postoperative surveillance should be implemented to avoid nosocomial infection and ensure the safety of patients and the health care workforce. With reference to the guidelines and recommendations issued by the National Health Commission and Chinese Society of Anesthesiology, this article provides recommendations for anesthesia management of trauma and emergency surgery cases during the COVID-19 pandemic.
The outbreak of a novel coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) has led to a public health emergency of international concern. Despite rigorous global containment and quarantine efforts, the incidence of Coronavirus Disease 2019 (COVID-19) is continuously rising, with 2,328,095 laboratory-confirmed cases and 160,515 deaths worldwide as of April 19, 2020. Although the overall casefatality rate (somewhere around 4.1% in early results) of COVID-19 seems to be lower than that of severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), nearly 14% of patients are critically ill and demand massive intensive care resources.1 A large-scale outbreak of COVID-19 will potentially paralyze some fragile health systems.
During the ongoing COVID-19 epidemic, most hospitals have postponed elective surgery to focus medical resources on COVID-19 patients and reduce the risk of nosocomial infections. With the ongoing spread of the COVID-19 epidemic, the ability of epidemiological history to identify patients at risk for COVID-19 has weakened. The number of asymptomatic patients is increasing, given the incubation period of COVID-19 (7–14 days).2 The timeframe for preoperative evaluation of emergency trauma patients is rather limited. Furthermore, trauma, as well as other underlying diseases, can also lead to fever and increased respiration and heart rate. These factors confound the preoperative diagnosis of COVID-19 in trauma and emergency surgery patients. Therefore, it is urgent to establish a workflow for emergency surgery and infection control during the pandemic. This recommendation on anesthesia management is developed based on Novel Coronavirus Diagnosis and Treatment Plan (Seventh Edition) issued by National Health Commission of the People’s Republic of China3 and “Routine Anesthesia Management and Prevention and Control Process Recommendations During COVID-19 Epidemic” issued by the Chinese Society of Anesthesiology.4,5
PREOPERATIVE EVALUATION AND PREPARATION
Preoperative Evaluation
Trauma patients need to be effectively evaluated and treated in a limited timeframe. It is important to accomplish COVID-19 triage and preoperative evaluation as quickly as possible. During the epidemic, for American Society of Anesthesiologists physical status (ASA-PS) classificationI andII patients, it is recommended to conduct preoperative anesthesia evaluation through the electronic medical record. For American Society of Anesthesiologists (ASA) III andIV patients, face-to-face preoperative anesthesia evaluation is still recommended. In well-controlled regions (with intensive infection source control, strict community containment, and intensified active surveillance) with sporadic new cases, patients with epidemiological history or clinical symptoms related to COVID-19 are recommended to receive chest computed tomography (CT) scan, complete blood count, and SARS-CoV-2 nucleic acid test6; in the regions where the epidemic situation is not effectively controlled (with a large number of new cases), it is recommended that all emergency patients should receive chest CT scan, complete blood count, and SARS-CoV-2 nucleic acid test. Critical patients whose condition does not allow chest CT scan should be treated as suspected COVID-19 cases until proven otherwise. Special attention needs to be focused on the differential diagnosis of CT manifestation between pulmonary contusion (when consistent with the mechanism of injury) and COVID-19 infection. In case of difficulties in differentiation, enhanced levels of protection should be used. In the epidemic outburst area (with a large number of confirmed cases and a booming number of new cases), level3 protection should be implemented in all emergency surgeries due to increased risk of encountering asymptomatic patients,infected patients in the incubation period, or patients with false-negative screening results. Becausethe SARS-CoV-2 nucleic acid test of pharyngeal swab specimens has a low sensitivity, a bronchoalveolar lavage specimen (with a positive rate of 93%) might be considered after intubation. The result may better guide postoperative treatment.7 Treatment of critical trauma patients with COVID-19 infection is challenging. Patients with minor symptom may progress into severe cases during hospitalization. Early identification of high-risk patients can reduce the risk of adverse outcome.8 The treatment of patients with severe trauma must not be delayed due to COVID-19. The workflow of COVID-19 triage for emergency surgery during the epidemic is illustrated in Figure 1.
Figure 1.
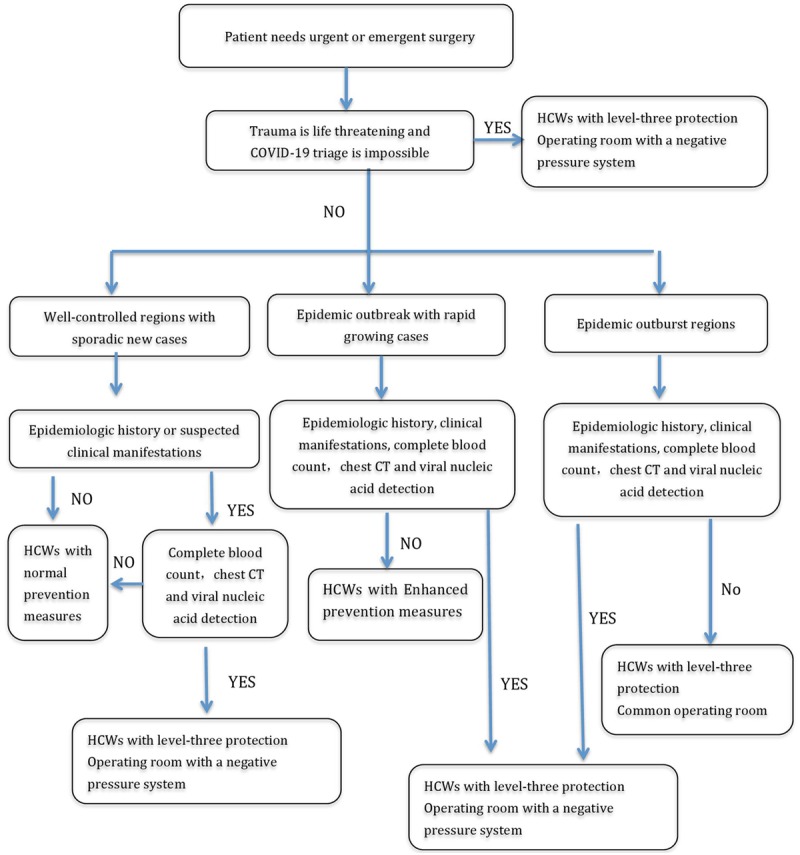
Workflow of COVID-19 triage for emergency surgery and infection precautions for HCWs during the epidemic. (1) In case of multiple suspected or confirmed COVID-19 emergency cases, the more critical patients should be treated first. A 30-minute gap should be taken between 2 operations after thorough disinfection of the OR.(2) If a negative pressure OR is not available, an OR with a separate air conditioning and humidification system should be chosen, or a regular OR can be used with the air conditioning system shut down. (3) Elective surgeries for patients with suspected or confirmed COVID-19 should be postponed. COVID-19 indicates Coronavirus Disease 2019; CT, computed tomography; HCW, health care worker; OR, operating room.
Personnel Allocation and Infection Precautions
During the epidemic, incorrect infection preventions may create a “super spreader,” who can introduce SARS-CoV-2 infections into a high-volume health care facility and cause a serious nosocomial outbreak.3 Therefore, the infection control strategy of medical staff, environment, and devices is a top priority. All COVID-19–related emergency surgeries should be performed under strict infection precautions. Anesthesia should be performed by a senior anesthesia clinician with another one on standby in the anteroom (yellow area) to provide further assistance. For patients with ASA III andIV classification or predicted difficult airway, an experienced expert should be available to assist. Detailed infection precautions for health care workers (HCWs) during anesthesia should be consistent with Perioperative Management of Patients Infected With the Novel Coronavirus issued by the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists.5 Anesthesiologists should implement level3 protection for surgical patients with suspected or confirmed COVID-19 (Figures 2 and 3). Personal protective equipment (PPE) should be donned and doffed in a strict order according to one’s specific institutional guidelines and under careful supervision of an infection control officer. Recommended PPEs for different levels of protection is shown in Table. It should be pointed out that use of PPE will inevitably hinder the visual, hearing ability, and hand dexterity of anesthesiologists, which will impair monitoring accuracy and the success rate of anesthesia procedures.9
Figure 2.

Anesthesiologists with personal protective equipment for COVID-19 in the operating room (Photograph by Dr Wei Mei).
Figure 3.

Endotracheal intubation for a COVID-19 patient in the isolation ward (Photograph by Dr Zhijie Lu). COVID-19 indicates Coronavirus Disease 2019.
Table.
PPE for Different Levels of Professional Protection During COVID-19 Epidemic
| Level of Protection | Applicable Settings | Applicable Procedures | Work Clothes | Disposable Hair Cover | Surgical Masks | Latex Gloves | N95 Respirators or Higher-Level Masks | Fluid-Resistant Gown | Protective Coverall | Goggles/Face Shield | Disposable Shoe Covers | Positive Pressure Breathing Headgears |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level1 protection | General clinics and ward | General diagnosis and treatment | √ | √ | √ | If needed | ||||||
| Level2 protection | Fever clinics | General diagnosis and treatment | √ | √ | √ | √ | √ | If needed | √ | √ | ||
| Level3 protection | Isolation ward, fever clinic, isolation area, operating room, and laboratory | Sputum aspiration, lower respiratory tract sampling, endotracheal intubation and tracheotomy, and other procedures involving airway intervention for COVID-19 related patients.Testrunning for COVID-19 samples | √ | √ | √ Double |
√ | √ | √ | √ | √ | Recommended |
Abbreviations: COVID-19, Coronavirus Disease 2019; PPE, personal protective equipment.
Preoperative Preparation
For both suspected and confirmed COVID-19 patients, proper PPE should be worn by all HCWs involved, and surgery needs to be performed in a negative pressure operating room (OR) with an anteroom beside it (buffer area).5 The negative pressure system should be turned on 30 minutes before the patient is moved in. Operation can be performed when the negative pressure reaches −5Pka or lower.10 Warning signs of COVID-19 should be placed outside the OR. During the operation, it is necessary to keep the OR closed and restrict the number of HCWs who pass through the door. All unnecessary devices should be removed from the OR before surgery. Necessary devices, such as computers, anesthesia machines, and telephones, should be covered with disposable plastic wrap. The central suction system should not be used, and a substitute electric suction device is recommended. Adequate medications and fluids should be prepared before the surgery and placed in the OR away from the operating area.
ANESTHESIA MANAGEMENT FOR EMERGENCY TRAUMA SURGERY DURING THE COVID-19 EPIDEMIC
Choice of Anesthesia Method
For patients with suspected or confirmed COVID-19, choice of anesthesia should be based on the patient’s overall situation, trauma condition, and needed surgical treatment. Regional anesthesia is preferred if it can meet the needs of surgery. Patients receiving regional anesthesia can use oxygen through a nasal cannula, with a surgical mask on top and a suction tube placed next to the mask. But for patients who are already on high-flow nasal oxygenation or mechanical ventilation or who have other indications for endotracheal intubation due to COVID-19,3 general anesthesia with endotracheal intubation should be applied. It is worth noting that SARS-CoV-2 may affect the central nervous system. According to recent studies, SARS-CoV-2 was discovered in patients’ cerebral spinal fluid and corpses’ brain tissues.11,12 Some patients also demonstrated symptoms of intracranial infection, such as headache, epilepsy, and consciousness disorder.12 Therefore, for patients with viremia, neuraxial procedures that breach the dura may carry a theoretical risk of viral translocation, although early experience from the hospitals in Wuhan didnot show meningoencephalitis related to neuraxial anesthesia in COVID-19 patients.9 Becauseno guidelines have been established regarding the safety of neuraxial procedures, the decision should be made after discussion among anesthesia, surgery, and infectious disease colleagues and following a thoughtful discussion with the patient. Furthermore, nearly 20% of patients with COVID-19 have coagulopathy, and almost all the severe and critical patients have coagulation dysfunction.13 These conditions may represent a contraindication to neuraxial anesthesia.
Although there is no specific antiviral treatment recommended for COVID-19, some potential drugs are widely in use, including an antiviral drug remdesivir, the malaria medication chloroquine/hydroxychloroquine, a combination of the HIV drugs lopinavir–ritonavir, and an immune system messenger interferon-β. Chloroquine and hydroxychloroquine have received intense attention because of positive results from small studies.14 But chloroquine and hydroxychloroquine have many side effects, including toxic myopathy, retinal impairment, and even heart injury in rare cases. Some animal studies showed that administration of chloroquine could increase the severity of sevoflurane anesthesia–induced neuronal apoptosis and memory impairment.15 There is also evidence showing that treatment with lopinavir–ritonavir may significantly increase the placental transfer of bupivacaine enantiomers during epidural anesthesia for cesarean delivery.16 Therefore, we suggest that thorough preoperative medication history should be collected, and special attention should be paid to the side effects of the COVID-19 treatment and its potential interactions with anesthetics. Furthermore, there has been speculation that consumption of angiotensin-converting enzyme inhibitor and nonsteroidal anti-inflammatory drugs might worsen the consequences of infection.17 But strict avoidance of these drugs is ill advised, because there is no clinical evidence supporting these hypotheses yet.
Anesthesia Induction and Endotracheal Intubation
During the COVID-19 outbreak, all patients scheduled for emergent surgery should wear masks without an air outlet before being intubated, if possible. Anesthesiologists should pay special attention to the airway evaluation, becausecervical spine injury, airway injury, and difficult airway are common in trauma patients. Patients with COVID-19 may suffer from respiratory distress and/or hypoxemia or even respiratory failure. Therefore, delays during tracheal intubation and multiple attempts at laryngoscopy may increase the risk of complications, including severe hypoxemia, cardiac arrest, and death.18 To shorten intubation time and increase “first-pass success” rate, intubation should be performed by experienced anesthesiologists and facilitated by video laryngoscope.
Detailed procedure for airway management for COVID-19 patients during general anesthesia can be referenced in Expert Recommendations for the Safe Implementation of Endotracheal Intubation Among Critical Patients With Coronavirus Disease 2019 issued by the Airway Management Group of the Chinese Society of Anesthesiology.19 When intubating suspected or confirmed COVID-19 patients, sufficient neuromuscular relaxant should be applied to eliminate cough reflex; aerosol-producing procedures like suctioning should be avoided if possible. Modified rapid sequence induction is recommended for emergency trauma patients. We recommend cricoid force be applied by an experienced assistant to patients with high risk of gastroesophageal reflux. For suspected or confirmed COVID-19 patients, cricoid force should be used with caution because it may cause pharyngeal reflex, while its utility in preventing aspiration remains controversial. Propofol and rocuronium are reasonable drug choices for rapid sequence induction. Etomidate might be used in hemorrhagic shock patients, but its immunosuppressive effects are a relative contraindication to use in COVID-19 patients. Bag mask ventilation should be avoided after induction, while ventilation with low tidal volume and high frequency is recommended in case of severe hypoxemia. For patients with suspected or confirmed COVID-19, proper positioning of the endotracheal tube should be confirmed by chest movement and a waveform of end-tidal carbon dioxide (Etco2), rather than by auscultation. For patients with difficult airway, guidelines for difficult airway management should be followed. For patients with difficult intubation, but without difficult oxygenation, the most familiar airway devices (bronchoscope, video laryngoscope, or light wand) to facilitate endotracheal intubation after anesthesia induction were chosen. For patients with high risk of “cannot intubate and cannot oxygenate,” cricothyroidotomy or tracheotomy directly was proceeded. For patients complicated with hemodynamic instability, proper vasopressors should be prepared before induction.
Anesthesia Monitoring
Mild trauma patients may only require basic noninvasive monitoring, including electrocardiogram, blood pressure, pulse oxygen saturation, Etco2, body temperature, and urine output. COVID-19 may cause pneumonia of varying degrees; thus, lung compliance, airway pressure, oxygen index, and arterial blood gas should be monitored closely. A lung-protective ventilation strategy should be implemented. Acute cardiac injury and renal injury are common in severe or critical COVID-19 patients.20 Therefore, myocardial enzymes, echocardiography, and renal function analysis are highly recommended before emergency surgery in severe COVID-19 patients.
Anesthesia Management
Emergency trauma patients should be treated promptly to avoid hypothermia, acidosis, and coagulative dysfunction. Surgical hemostasis, body temperature monitoring and preservation, volume resuscitation, coagulative monitoring and management, and thromboprophylaxis should be implemented as needed.
Damage Control Surgery.
COVID-19 can cause immune dysfunction, which presents as overall immunosuppression.21 The rate of severe infection secondary to trauma can be predicted to increase in COVID-19 patients. If COVID-19 patients are complicated with secondary infections, sepsis and multiple organ dysfunction syndrome (MODS) may occur; thus, emergency surgery should follow the principles of damage control. Surgical manipulation should be minimized, and surgical duration should be shortened. Emergency trauma surgeries in COVID-19 patients should be limited to damage control surgeries, including (1) blunt injury with prehospital index (PHI) ≥4; (2)hemodynamic instability caused by thoracic or abdominal penetrating injury; (3) uncontrolled external hemorrhage, such as thoracic or abdominal organ injury, tension or open pneumothorax, cardiac tamponade, massive hemothorax, severe craniocerebral injury, cerebral hernia, and other severe injuries; and (4)acute care surgery occurring in patients with confirmed or suspected COVID-19 during hospitalization, such as organ perforation or obstruction.
Fluid Management.
Perioperative systolic blood pressure (SBP) and mean arterial blood pressure (MAP) should be maintained within 80–90 and 50–60 mm Hg, respectively, in emergency trauma patients. For patients with craniocerebral injury, SBP should be maintained at 100–110 mm Hg during resuscitation.22 Goal-directed fluid therapy is recommended to avoid either hypovolemia or hypervolemia. Whether restrictive fluid management is beneficial for pulmonary protection in COVID-19 patients remains unknown. For patients with uncontrolled hemorrhage, fluid therapy and vasopressor can be used to maintain the targeted blood pressure. As allogenic blood transfusion may cause circulatory overload and lung injury, blood products should be transfused with caution.23 Red blood cells should be transfused to maintain adequate oxygen supply, indicated by lactic acid level and mixed venous oxygen saturation. Plasma and other blood products should be transfused according to the results of coagulation testing. Blood samples of COVID-19 patients should be double-bagged and labeled with a warning sign of “COVID-19.” During the COVID-19 epidemic, a severe shortage of blood is foreseeable; thus, intraoperative blood protection strategies are recommended to minimize the requirements of allogenic blood transfusion.
Respiratory Management.
Acute respiratory distress syndrome is one of the main clinical manifestations in severe COVID-19 patients, and pulmonary contusion is common in emergency trauma patients. Perioperative lung-protective ventilation strategy is recommended to reduce the risk of ventilator-associated lung injury. During surgery, lung compliance, airway pressure, oxygen index, and arterial blood gas should be monitored closely, to provide guidance for optimal ventilator settings. According to Guidelines of Diagnosis and Treatment of COVID-19 (Seventh Edition), small tidal volume (6–8 mL/kg ideal body weight) and low plateau pressure (≤30 cmH2O) with permissive hypercapnia are recommended, except for patients with known or suspected brain injury.3 In the setting of plateau pressure ≤35 cmH2O, a proper level of positive end-expiratory pressure can also be used. To reduce viral contamination to the anesthesia machine and maintain heat and moisture within the breathing circuit, high efficiency particulate air filters should be installed between the mask and the breathing circuit and at the expiratory end of the breathing circuit. Considering the amount of airway secretions, endotracheal suction using a closed system should be performed regularly. Recruitment maneuvers 3–5 times/h are recommended to reduce atelectasis. The pressure used for recruitment maneuvers should be tailored to the compliance of the patient’s lung.
Endotracheal Extubation.
Because the asymptomatic rate of the infected COVID-19 patients is high and the incubation period of SARS-CoV-2 is long, we suggest that all the extubation should be performed in the OR, rather than in the postanesthesia care unit. The number of HCWs in the OR should be restricted during extubation. Level3 protection should be provided to HCWs extubating COVID-19–related patients, and level 1 or 2 protection to HCWs extubating non-COVID-19 patients. Before extubation, suction of the lower airway and oropharyngeal sections should be performed with the patient in an adequately deep plane of anesthesia. Administration of propofol, dexmedetomidine, or remifentanil can be used to minimize the cough reflex during extubation.24–26 For COVID-19 patients, laryngeal mask exchange (Bailey maneuver) technique, which involves the replacement of an endotracheal tube with a laryngeal mask, is another way to create a smooth extubation. The Bailey maneuver can maintain a patent and unstimulated airway and allow for stable physiological observations and protection of the airway from soiling secondary to blood and secretions in the mouth.27 This technique is superior to either awake or deep extubation for patients with irritable airways. After extubation, COVID-19 patients should be monitored for at least 20–30 minutes in the OR and then betransferred to the isolation ward directly. Non-COVID-19 patients can be transferred to the postoperative care unit with a surgical mask in place for further recovery before transportation to the general ward.
With cases of COVID-19 climbing steeply, numerous hospitals all over the world are experiencing a shortage of intensive care unit (ICU) beds and ventilators during the current pandemic. Patients who need only short periods of postoperative respiratory support can be monitored and cared for in the OR until extubation. In some hospitals, if needed, the OR may be transformed into a critical care environment for ongoing ventilatory support.
Thromboprophylaxis.
The incidence of thrombosis among patients with multiple traumas is as high as 50%, and pulmonary embolism is the leading cause of death for patients surviving the first 3 days after trauma.28 Acute inflammatory reaction caused by COVID-19 can affect coagulation and fibrinolysis by several means, such as decreasing the level of circulatory protein C and antithrombin-III, and upregulating of plasminogen activator inhibitor-1. These changes can further activate the coagulation cascade and inhibit fibrinolysis, thus promoting thrombosis.13 Therefore, perioperative thromboprophylaxis is of vital importance for trauma patients with COVID-19. Lin et al21 recommended that low-molecular-weight heparin (LMWH) anticoagulant therapy, together with high-dose intravenous immunoglobulin, could be given to COVID-19 patients as early as possible when T cells, B cells, inflammatory cytokines, and d-dimer show the following trends: T lymphocytes and B lymphocytes in peripheral blood are significantly lower than before; inflammatory cytokines such as IL-6 are increased significantly; coagulation parameters such as d-dimer are increased abnormally; and chest CT indicates the expansion of lung lesions.21 They recommended that anticoagulation therapy should be initiated in COVID-19 patients when the d-dimer value was 4 times higher than the normal upper limit, unless obvious anticoagulant contraindications were present. The recommended dose of LMWH is 100U/kg weight per 12 hours by subcutaneous injection for 3–5 days. However, for patients with high risk of postoperative hemorrhage or renal insufficiency, LMWH should be used with caution. Previous evidence has shown that early administration of tranexamic acid safely reduced death from severe bleeding in trauma.29 Therefore, early administration of tranexamic acid may be reasonable in traumatically bleeding patients with COVID-19. But when bleeding is not life-threatening, the thrombotic risk of tranexamic acid is too poorly documented to justify exposing COVID-19 patients to a plausible and inadequately evaluated risk.
Postoperative Pain Management.
Multimodal analgesia is recommended, including regional block analgesia, local infiltration analgesia, opioid drugs, and nonopioid drugs. Becausepatients with COVID-19 may be complicated with hepatic and/or renal insufficiency, as well as coagulation dysfunction, the contradictions and indications of nonsteroidal anti-inflammatory drugs should be prudently evaluated. Considering the diminished pulmonary function in patients with COVID-19, the dosage of opioids should be adjusted to avoid aggravating respiratory depression or carbon dioxide retention.
The Prevention and Treatment of Postoperative Nausea and Vomiting.
Postoperative nausea and vomiting (PONV) can produce virus-containing aerosol. Therefore, PONV should be effectively prevented. A multimodal prevention strategy is recommended, based on the presence of risk factors (female, nonsmoker, history of motion sickness, and postoperative use of opioid).30 For the patients with one or no risk factor, preventive medication is not necessary. For the ones with ≥2 risk factors, combined use of antiemetic medications is recommended, such as dexamethasone and 5-hydroxytryptamine 3 (5-HT3) inhibitors. Use of opioid drugs should be restricted in high-risk patients.
POSTOPERATIVE SURVEILLANCE
Patients who screened negative for COVID-19 diagnosis preoperatively should still be surveilled after surgery, because they may be in the incubation period preoperatively or they might become infected perioperatively. Body temperature, complete blood count, the level of procalcitonin, and C-reactive protein should be monitored regularly. Chest CT and viral nucleic acid test in throat swab specimens should be rechecked, if necessary. Visitation should be restricted, and the wards should be equipped with strict entrance guards. Patients and their accompanying relatives should be educated on personal protective measures, such as wearing masks, hand hygiene, and daily body temperature monitoring.
HCWs, if they have exposure to confirmed or suspected COVID-19 patients without proper self-protection, should be isolated and surveilled postoperatively for 14 days. The HCWs involved in each surgery should be carefully documented, to enable subsequent contact tracing. If a misdiagnosed patient develops symptoms of COVID-19 or is diagnosed as confirmed COVID-19 infection postoperatively, all the related HCWs should be traced and isolated immediately. Follow-up diagnosis and treatment should be arranged, if necessary. Available data suggest that 17%–30% of infected persons are asymptomatic, ergo all HCWs should keep social distancing in cafeterias, break areas, and offices.31,32
In general, a special triage protocol and strict infection precautions should be followed when performing emergency trauma surgeries during the COVID-19 epidemic. Determination of COVID-19 status should be sought in the emergency department and verified again by the anesthesiologist before surgery. For suspected or confirmed COVID-19 patients, surgeries should be performed in negative pressure ORs in designated hospitals, by HCWs applying level3 protection. In the epidemic outburst regions, HCWs should apply level3 protection in every emergency surgery, regardless of the results of COVID-19 testing. During surgery, infection control precautions should be strictly followed, especially during airway intervention. Goal-directed fluid therapy and lung-protective ventilation strategy should be carefully applied. Postoperative anticoagulation therapy is recommended in trauma patients with COVID-19, except for those with obvious contraindications. Postoperative surveillance of the patients who have been excluded from COVID-19 diagnosis preoperatively is very important, especially in epidemic outburst regions.
DISCLOSURES
Name: Yahong Gong, MD.
Contribution: This author helped draft the whole manuscript.
Name: Xuezhao Cao, MD, PhD.
Contribution: This author helped draft the whole manuscript.
Name: Wei Mei, MD, PhD.
Contribution: This author helped draft the section on anesthesia management.
Name: Jun Wang, MD, PhD.
Contribution: This author helped draft the section on anesthesia management.
Name: Le Shen, MD, PhD.
Contribution: This author helped draft the section on infection precaution.
Name: Sheng Wang, MD.
Contribution: This author helped draft the section on infection precautions.
Name: Zhijie Lu, MD.
Contribution: This author helped draft the section on anesthesia management.
Name: Chunhua Yu, MD.
Contribution: This author helped draft the section on triage of workflow.
Name: Lu Che, MD.
Contribution: This author helped draft the section on postoperative surveillance.
Name: Xiaohan Xu, MD.
Contribution: This author helped draft the section on postoperative surveillance.
Name: Juan Tan, MD.
Contribution: This author helped draft the section on anesthesia management.
Name: Hong Ma, MD.
Contribution: This author helped review and revise the manuscript.
Name: Yuguang Huang, MD.
Contribution: This author helped review and fully revise the manuscript.
This manuscript was handled by: Richard P. Dutton, MD.
FOOTNOTES
GLOSSARY
- 5-HT3
- 5-hydroxytryptamine 3
- ASA
- American Society of Anesthesiologists
- ASA-PS
- American Society of Anesthesiologists physical status
- COVID-19
- Coronavirus Disease 2019
- CT
- computed tomography
- Etco2
- end-tidal carbon dioxide
- HCWs
- health care workers
- HIV
- XXX
- ICU
- intensive care unit
- LMWH
- low-molecular-weight heparin
- MAP =
- mean arterial blood pressure
- MERS
- Middle East respiratory syndrome
- MODS =
- multiple organ dysfunction syndrome
- OR
- operating room
- PHI =
- prehospital index
- PONV
- postoperative nausea and vomiting
- PPE
- personal protective equipment
- SARS
- severe acute respiratory syndrome
- SARS-CoV-2
- severe acute respiratory syndrome coronavirus 2
- SBP
- systolic blood pressure
Funding: None.
The authors declare no conflicts of interest.
Reprints will not be available from the authors.
REFERENCES
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health Commission & State Administration of Traditional Chinese Medicine. Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial Version 7). 2020. Available at: http://en.nhc.gov.cn/2020-03/29/c_78469.htm. Accessed April 20, 2020.
- 4.Chinese Society of Anesthesiology and Chinese Association of Anesthesiologists. Anesthesia management and prevention procedures of conventional surgery during COVID-19 epidemic. 2020. Available at: http://www.csahq.cn/guide/detail_1045.html. Accessed April 20, 2020.
- 5.Chen XD, Liu YH, Gong YH, et al. Perioperative management of patients infected with the novel coronavirus: recommendation from the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Workgroup on Novel Coronavirus Pneumonia Diagnosis and Treatment of Peking Union Medical College Hospital. Diagnosis and treatment regimen of novel coronavirus pneumonia of Peking Union Medical College Hospital. (V2.0). Zhonghua Nei Ke Za Zhi. 2020;59:186–188. [DOI] [PubMed] [Google Scholar]
- 7.Wang WL, Xu YL, Gao RQ, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Li ZF, Mao QX. Expert recommendations for severe emergency trauma surgery and infection prevention during COVID-19 epidemic. Chin J Trauma. 2020;36:1–7. [Google Scholar]
- 9.Zhou ZQ, Sun XX, Li SY, Wan L, Luo AL, Han DJ. Anesthesia management for cesarean section during novel coronavirous epidemic. Chin J Anesthesiol. 2020. [Epub ahead of print]. [Google Scholar]
- 10.Li Y, Li ZF, Mao QX, et al. Expert recommendations for infection prevention of severe trauma patients during COVID-19 epidemic. Zhong Hua Chuang Shang Za Zhi. 2020;36:1–7. [Google Scholar]
- 11.Chinese Society of Neurologist. Neurologist expert consensus of COVID-19 clinical prevention. Chin J Neurol. 2020;53:E001–E001. [Google Scholar]
- 12.Xu J, Zhong S, Liu J, et al. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin Infect Dis. 2005;41:1089–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pulmonary Embolism and Pulmonary Vascular Disease Group of Chinese Thoracic Society, Pulmonary Embolism and Pulmonary Vascular Disease Committee of CACP, National Cooperation Group of Pulmonary Embolism and Pulmonary Vascular Disease. Recommendations for novel coronavirus pneumonia associated venous thromboembolism prevention. Natl Med China. 2020;100:E007–E007. [Google Scholar]
- 14.Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020. [Epub head of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang XM, Zhou YF, Xu MM, Chen G. Autophagy is involved in the sevoflurane anesthesia-induced cognitive dysfunction of aged rats. PLoS One. 2016;11:e0153505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ribeiro RMP, Moreira FL, Moisés ECD, et al. Lopinavir/ritonavir treatment increases the placental transfer of bupivacaine enantiomers in human immunodeficiency virus-infected pregnant women. Br J Clin Pharmacol. 2018;84:2415–2421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cook TM, Woodall N, Harper J, Benger J; Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth. 2011;106:632–642. [DOI] [PubMed] [Google Scholar]
- 19.Zuo MZ, Huang YG, Ma WH, et al. Expert recommendations for tracheal intubation in critically ill patients with noval coronavirus disease 2019. Chin Med Sci J. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin L, Lu L, Cao W, Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection-a review of immune changes in patients with viral pneumonia. Emerg Microbes Infect. 2020;9:727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mi WD, Ge HJ, Zhang TZ, et al. Guidelines of anesthesia and circulatory management to war wound and trauma. Perioper Saf Qual Assur. 2020:19–24. [Google Scholar]
- 23.Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload and transfusion-related acute lung injury. Blood. 2019;133:1840–1853. [DOI] [PubMed] [Google Scholar]
- 24.Pak HJ, Lee WH, Ji SM, Choi YH. Effect of a small dose of propofol or ketamine to prevent coughing and laryngospasm in children awakening from general anesthesia. Korean J Anesthesiol. 2011;60:25–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Popat M, Mitchell V, Dravid R, Patel A, Swampillai C, Higgs A; Difficult Airway Society Extubation Guidelines Group. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia. 2012;67:318–340. [DOI] [PubMed] [Google Scholar]
- 26.Nho JS, Lee SY, Kang JM, et al. Effects of maintaining a remifentanil infusion on the recovery profiles during emergence from anaesthesia and tracheal extubation. Br J Anaesth. 2009;103:817–821. [DOI] [PubMed] [Google Scholar]
- 27.Stix MS, Borromeo CJ, Sciortino GJ, Teague PD. Learning to exchange an endotracheal tube for a laryngeal mask prior to emergence. Can J Anaesth. 2001;48:795–799. [DOI] [PubMed] [Google Scholar]
- 28.Ma H. 2015. Available at: http://www.doc88.com/p-9721740047042.html. Accessed April 20, 2020.
- 29.CRASH-3 Trial Collaborators. Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomised, placebo-controlled trial. Lancet. 2019;394:1713–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chao XZ, Paul FW, Ma H. An update on the management of postoperative nausea and vomiting. J Anesth. 2017;31:617–626. [DOI] [PubMed] [Google Scholar]
- 31.Nishiura H, Kobayashi T, Suzuki A, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25:2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]


