Abstract
We have previously identified neutralizing human monoclonal antibodies against Nipah virus (NiV) and Hendra virus (HeV) by panning a large nonimmune antibody library against a soluble form of the HeV attachment-envelope glycoprotein G (sGHeV). One of these antibodies, m102, which exhibited the highest level of cross-reactive neutralization of both NiV and HeV G, was affinity maturated by light-chain shuffling combined with random mutagenesis of its heavy-chain variable domain and panning against sGHeV. One of the selected antibody Fab clones, m102.4, had affinity of binding to sGHeV that was equal to or higher than that of the other Fabs; it was converted to IgG1 and tested against infectious NiV and HeV. It exhibited exceptionally potent and cross-reactive inhibitory activity with 50% inhibitory concentrations below 0.04 and 0.6 μg/mL, respectively. The virus-neutralizing activity correlated with the binding affinity of the antibody to sGHeV and sGNiV. m102.4 bound a soluble form of NiV G (sGNiV) better than it bound sGHeV, and it neutralized NiV better than HeV, despite being originally selected against sGHeV. These results suggest that m102.4 has potential as a therapeutic agent for the treatment of diseases caused by henipaviruses. It could be also used for prophylaxis and diagnosis, and as a research reagent
Hendra virus (HeV) and Nipah virus (NiV) are highly pathogenic paramyxoviruses that have recently emerged from flying fox populations to cause serious disease outbreaks in humans and livestock in Australia, Malaysia, Singapore, Bangladesh, and India [1]. HeV emerged in Queensland, Australia, in 1994, killing 1 human and 14 horses [2] and the virus was responsible for at least 4 other sporadic outbreaks involving horses and humans between 1994 and 2006 [1]. The closely related NiV emerged in 1998–1999 in peninsular Malaysia, resulting in the death of more than 100 people and the culling of more than one million pigs [3]. Since then, several outbreaks of NiV infection have been recorded in Bangladesh and India [1, 4, 5]. Several important observations have been made during these most recent outbreaks, such as a higher incidence of acute respiratory distress syndrome, higher rates of person-to-person transmission, and higher case fatality rates (60%–75%), compared with the Malaysian outbreak (with case fatality rates of 40%) in which the virus was initially discovered [6–10]
There are currently no therapeutic modalities for treating NiV or HeV infections, and a vaccine for prevention of disease in human or livestock populations does not exist. The first antiviral antibody-based drug approved by the U.S. Food and Drug Administration is a humanized antibody against respiratory syncytial virus (manufactured by Medimmune), which has proven to be highly successful in reducing respiratory syncytial virus infection in infants and immunocompromised patients; this antibody has been recently improved [11]. In this context, the development of neutralizing human MAbs (HMAbs) against henipaviruses could have important implications for prophylaxis and passive immunotherapy
One of the challenges in the development of human antibodies for antiviral applications is the heterogeneity and mutability of RNA viruses. It is, therefore, important to select antibodies that recognize epitopes that are highly conserved among different virus variants. Previously, we reported the isolation and characterization of potent neutralizing recombinant HMAbs that targeted the viral envelope glycoprotein G by use of a highly purified, oligomeric, soluble HeV G glycoprotein (sGHeV) [12] as the antigen for the screening of a large, naive human phage-displayed antibody library [13]. One of these antibodies, m102, exhibited cross-neutralizing activity against both HeV and NiV. In this article, we report the identification and characterization of a novel antibody, m102.4, derived from m102 by light-chain shuffling and heavy-chain variable domain random mutagenesis. This antibody exhibits exceptional potency against both, NiV and HeV, and being fully human antibody, it could be directly used for prophylaxis or treatment of humans exposed to or infected by HeV or NiV. Such an antibody could also be used for improved diagnosis and as a research tool for better understanding of virus-host interaction. Fine mapping of the HMAb-defined epitope may also provide information useful for the rational development of candidate vaccines and small molecule drugs
Methods
Cells and culture conditionsHeLa-USU cells have been described elsewhere [12, 14]. Vero cells were provided by the Australian Animal Health laboratory. The human glioblastoma cell line U373-MG was provided by Adam P. Geballe, Fred Hutchinson Cancer Research Center, Seattle. HeLa-USU and U373 cells were maintained in Dulbecco’s modified Eagle medium (DMEM [Quality Biologicals]) supplemented with 10% cosmic calf serum (HyClone), and 2 mmol/L L-glutamine (DMEM-10). Vero cells were maintained in Eagle minimal essential medium (EMEM) (Invitrogen) supplemented with 10% fetal calf serum (Invitrogen Australia Pty. Ltd), 1 mmol/L HEPES (Invitrogen), and 2 mmol/L L-glutamine (Invitrogen) (EMEM-10). All cell cultures were maintained at 37°C in a humidified 5% CO2 atmosphere
Generation of phage-displayed Fab libraries and selection of affinity-matured FabsThe original human Fab phage display library, from which the antibodies m101–m107 were identified [13], was used as the source for the light-chain variable domain (VL) repertoire in the shuffled library. The phagemid preparation from the original library was first digested with NcoI and SpeI, followed by electrophoresis on an agarose gel to delete the entire heavy-chain variable domain (VH) repertoire. The gene encoding the VH of m102 was amplified by error-prone polymerase chain reaction (PCR) (Stratagene) to introduce random mutations and then fused with the CH1 gene fragment by use of splicing by overlapping extension PCR. The fused fragment was digested with NcoI and SpeI and purified from gel; it was then ligated into the purified backbone vector to create the VLs-shuffled Fab repertoire. Escherichia coli TG1 cells were transformed with the ligation mixtures via electroporation. The transformed TG1 cells were plated on 2× yeast extract–tryptone (2YT) agar plates containing 100 μg/mL ampicillin and 2% glucose (2YTAG). After incubation overnight at 37°C, all of the colonies grown on the plates were scraped into 5 mL of 2YTAG medium, mixed with 1.2 mL of 50% glycerol (final concentration, 10%), aliquoted, and stored at −70°C as the library stock. Two rounds of biopanning were performed on sGHeV conjugated magnetic beads as described for the original library panning [13]. Eight clones were identified as affinity-maturated antibodies, and m102.4 was selected for further characterization. Selected Fabs and m102.4 IgG1 expression and purification was performed as described elsewhere [14]
ELISA binding assayThe sGHeV glycoprotein (50 ng per well) was coated in a 96-well plate in 50 μL PBS. Serially diluted antibodies were added into the well after washing with 1×PBS with 0.05% Tween 20. After incubation for 1 hour at room temperature and washing, horseradish-peroxidase conjugated secondary antibody was added and incubated for another hour. After washing, plates were developed and read at 450 nm in an ELISA reader
Stable cell line construction and fermentationLinearlized m102.4 PDR12 construct was transfected into CHO K1 cells with polyfectin in accordance with the protocol from Qiagen. A stable antibody-producing cell line was selected by screening in glutamine acid–free culture medium with 50 μmol/L methionine sulphoximine. It was adapted to grow in suspension in serum-free medium. The antibody was produced by fermentation in a 15-L fermentor and purification was performed with protein A
Expression and immunoprecipitation of alanine HeV G mutantsAlanine mutations were introduced at specific residues in myc-tagged HeV G using site-directed mutagenesis (Stratagene). Expression and immunoprecipitation of all HeV G mutants were as performed as described elsewhere [15]
Binding and competition analysis using multiplex microsphere assaysMultiplexed microsphere assays were performed as described elsewhere [16]
Cell fusion assaysThe inhibition assay of cell fusion by Fabs and IgGs was performed as described elsewhere [12]
Virus neutralization assaysAll live virus experiments were conducted under strict biocontainment procedures in a biosafety level 4 laboratory. A total of 2×104 Vero cells were added per well with 150 μL EMEM-10 in 96-well plates and incubated overnight at 37°C in a humidified 5% CO2 atmosphere. The foci assay was performed as described elsewhere [12]
Antibody pharmacokinetics in plasma and biological activityFour juvenile (<12 months), male ferrets were anesthetized by mask induction with isofluorane and maintained on 2% isofluorane and 100% oxygen. A baseline blood sample was collected from an axillary vein, and a 20-g intravenous catheter was placed in the left jugular vein. The antibody m102.4 was administered via the catheter by slow infusion over 2 minutes; 2 ferrets received 25 mg of m102.4 and 2 ferrets received 5 mg of m102.4. The catheter was withdrawn, and animals were allowed to recover from the anesthetic. Subsequently, the ferrets were anesthetized on days 1, 4, 8, 12,18, 21, 28, 35, and 42 by intramuscular injection with ketamine (Ketamil; Ilium) and medetomidine (Domitor; Novartis) (reversed with atipamazole [Antisedan; Novartis]). Blood was collected from an axillary or jugular vein while animals were under anesthesia. After collection of the final blood sample, the animals were euthanized by means of an intravenous barbiturate overdose. For all samples, serum was aliquoted and stored at −80°C. Ferret serum was diluted 1:1000 and assayed by use of the binding multiplex microsphere assay described above. An m102.4 standard curve ranging from 500 ng/mL to 0.5 ng/mL and all ferret serum samples were assayed simultaneously. Ferret serum m102.4 concentrations were extrapolated from the standard curve using nonlinear regression analysis (GraphPad software; GraphPad). Half-lives were estimated from the slopes of the natural logarithms of the antibody concentration as function of time by using the formulas ta=0.69/a[[ln(2)=0.69] and tb=0.69/b[[ln(2)=0.69], where ta and tb are the distribution and elimination half-lives, respectively, a and b are measured as the slopes of ln (m102.4 concentration, μg/mL) dependent on time
Serum collected on days 1, 4, and 8 was evaluated in virus neutralization assays. All sera were diluted 1:5, 1:10, 1:20 and 1:40 and assayed in duplicate using the foci assay. Complete neutralization was defined as no viral foci in either well at a particular dilution
Results
In vitro maturation of m102Previously, we reported the isolation of henipavirus-neutralizing recombinant HMAbs by screening of a large nonimmune phage-displayed Fab library against a soluble form of the HeV G glycoprotein (sGHeV). One of these antibodies, m102, exhibited the highest level of cross-reactivity and relatively better binding to NiV G than to HeV G. We reasoned that improving m102’s binding to HeV G could further increase its cross-reactive neutralizing activity by increasing its affinity to HeV G. To mature in vitro m102, we constructed an antibody library—which contained approximately 2×108 clones—by light-chain shuffling combined with heavy-chain VH random mutations introduced by error-prone PCR. Two rounds of panning against sGHeV conjugated to magnetic beads demonstrated sufficient enrichment (data not shown), and 190 random colonies were screened by phage ELISA. The 24 best binders were selected for sequencing analysis. They represented 8 different clones, which were designated m102.1–m102.8. Although there were no amino acid sequence changes, silent mutations occurred in the VH regions in 3 of the 8 clones (data not shown), indicating that the error-prone PCR had worked. Seven of the 8 different light chains were from V κ subfamily III, which is the same as that of m102; 1 clone (m102.8) was from the V κ subfamily I. A sequence analysis of these light chains showed that all clones contained mutations in all 3 complementarity-determining regions; of the 7 clones from subfamily III, m102.4 had the largest number of mutations (data not shown)
All 8 clones were expressed as Fabs, purified, and analyzed by ELISA for binding to the selecting antigen sGHeV. The ELISA data confirmed that all 8 Fab clones displayed a higher level of binding to sGHeV than did the parental m102 Fab (figure 1). Clone m102.4, which had binding affinity equal to or higher than that of the other clones, was selected for further characterization and converted to an IgG1 format
Fig. 1.
Binding of Fab m102 and Fab m102 mutants with different light chains to sGHeV, as measured by ELISA
Binding of IgG1 m102.4 to cognate antigensTo investigate the binding of IgG1 m102.4 to HeV G and NiV G and its ability to block receptor-G interactions, we used 2 multiplex microsphere assays that we recently developed [16]. As shown in figure 2A, m102.4 binds to both sGHeV and sGNiV in a dose-dependent fashion. At relatively low concentrations (in the range of 50 ng/mL or less), the binding reached 50% of its maximum, indicating strong binding to both soluble G proteins. Furthermore, the multiplex assays also demonstrated that m102.4 is highly efficacious in blocking the binding of ephrin-B2 ligand (EFNB2) to both sGHeV and sGNiV (figure 2B). It is important to note that the increase in affinity did not alter the specificity of the Fab; it could still bind to both G proteins very well. It is also interesting to note that m102.4 binds sGNiV better than sGHeV, a result that was also reflected in its slightly better efficiency at blocking EFNB2-sGNiV binding. These results suggest that m102.4 is a cross-reactive, high-affinity binder to the soluble forms of both HeV G and NiV G glycoproteins
Fig. 2.
Characterization of m102.4 IgG1 by multiplex microsphere assays. A Direct binding assay; B Receptor-inhibition assay; see Materials and Methods for calculation of inhibition percentages. MFI, mean fluorescence intensity
Potent cross-reactive inhibition of Env-mediated cell fusion by m102.4The matured antibody m102.4 inhibited NiV and HeV Env-mediated cell fusion in both formats, as Fab and as IgG1. As expected, Fab m102.4 was significantly more potent than Fab m102, and IgG1 m102.4 was more potent than Fab m102.4 (figure 3). A comparison with a previously identified antibody, m101, which is specific for HeV and the most potent inhibitor of infectious HeV [13], suggested that m102.4 and m101 had comparable activity in both Fab and IgG1 formats (figure 3B). Interestingly, and similar to the multiplexed results, the inhibitory activity against NiV G–mediated cell fusion was higher than that against HeV G–mediated fusion although m102.4 was selected by using sGHeV. These results suggest m102.4 possesses exceptional cross-reactivity and potency against HeV and NiV Env-mediated cell fusion and syncytia formation
Fig. 3.

Comparative analysis of inhibition on henipavirus Env-mediated fusion by different antibodies. A Inhibition of Nipah virus (NiV) Env-mediated fusion; B inhibition of Hendra virus (HeV) Env-mediated fusion. HeLa-USU cells were infected with vaccinia recombinants encoding HeV (or NiV) F and G glycoproteins, and with a vaccinia recombinant encoding T7 RNA polymerase (effecter cells). Target cell U373 was infected with the Escherichia coli LacZ-encoding reporter vaccinia virus vCB21R. Serial diluted antibodies were preincubated with effecter cells for 0.5 h and then mixed with target cells. The cell fusion assay was performed for 2.5 h at 37°C. Antibody concentrations were plotted against beta-gal assay reading at 595 nm
Potent cross-reactive neutralization of live virusesIgG1 m102.4 exhibited exceptionally potent and cross-reactive inhibitory activity against infectious NiV and HeV with IC50 values below 0.04 and 0.6 μg/mL, respectively (table 1). These data suggest a strong correlation between binding to the antigens, inhibition of fusion, and neutralization of infectious virus and confirm the exceptional potency and cross-reactivity of m102.4. IgG1 m102.4 was also evaluated in the sensitive Vero cell-foci-immunostaining assay overnight side by side with IgG1 m101 (figure 4). In this case, not only was the amount of virus per well high (4000 TCID50 for HeV and 2000 TCID50 for NiV), but the antibody-virus mixtures were incubated on Vero cell monolayers overnight. If no antibody was present (panels A and F), there was massive coalesced syncytia for both viruses. In the presence of m101, HeV was neutralized to localized foci at 10 μg/mL, which was further reduced to individual infected cells at 50 μg/mL. Importantly, if this assay was carried out as a standard cytopathic effect–based neutralization assay, these wells would essentially look uninfected. By comparison, m102.4 neutralized 100% of HeV and NiV at either 10 μg/mL or 50 μg/mL. This extended neutralization window demonstrates the exceptional potency of m102.4 and may have important implications for postexposure therapeutic efficacy
Table 1.
Neutralization of live henipaviruses by IgG1 m102.4
Fig. 4.
Immunofluorescence-based syncytia assay of Hendra virus (HeV) and Nipah virus (NiV) infection. Vero cells were plated into 96-well plates and grown to 90% confluence. Virus and antibodies were premixed for 30 min at 37°C prior to addition to the cell monolayers. Cells were incubated in the presence of antibody-virus mixtures for 24 h, fixed in methanol, and immunofluorescently stained for P protein prior to digital microscopy. All images were obtained at an original magnification of 20×. A HeV without antibody; B HeV with m101 at 50 μg/mL; C HeV with m101 at 10 μg/m; D HeV with 102.4 at 50 μg/mL; E HeV with 102.4 at 10 μg/mL; F NiV without antibody; G NiV with m101 at 50 μg/mL; H NiV with m101 at 10 μg/mL; I NiV with 102.4 at 50 μg/mL; J NiV with 102.4 at 10 μg/mL
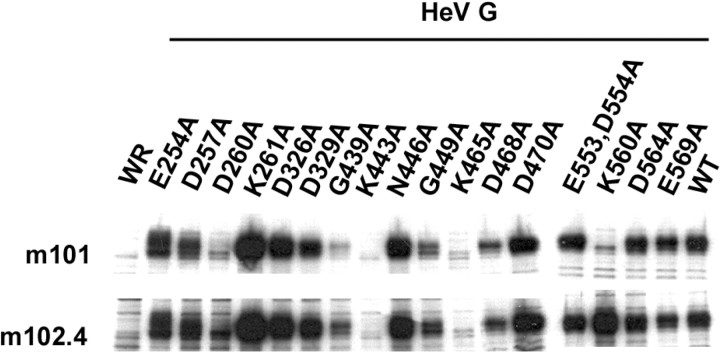
Characterization of the m102.4 epitopeTo characterize the epitope of the affinity-maturated m102.4—compared with m101—on the HeV G glycoprotein, a panel of 17 HeV G alanine-scanning mutants constructed in a previous study [15] were expressed and tested for binding to m101 and m102.4 by immunoprecipitation. The binding of HeV G mutants D260A, G439A, K443A, and K465A to both m101 and m102.4 was almost absent, whereas the mutations G449A and D468A significantly decreased the binding of both antibodies, although they did so to varying degrees (figure 5). Interestingly, one mutation, K560A, almost completely eliminated the binding of the HeV-specific antibody m101 but did not have any effect on the binding of the cross-reactive antibody m102.4. Bishop et al. [15] showed that all 4 mutations—D260A, G439A, K443A and K465A—that eliminated the binding of both MAbs in this study are detrimental for the binding of HeV G to the receptor ephrin-B2. These results suggest that the m102.4 epitope overlaps the receptor-binding domain of HeV G and the epitope of m101
Fig. 5.
Binding of m101 and m102.4 to alanine-scanning mutants of soluble Hendra virus (HeV) G glycoprotein (sGHeV). HeLa cells transfected with wild type GHeV, various alanine mutants of GHeV, or pMCO2 (empty vector) were infected with WR strain vaccinia virus to drive expression, radiolabeled with [35S] methionine-cysteine overnight, lysed in buffer containing Triton X-100, and then subjected to immunoprecipitation by m101 and m102.4. Lysates were then precipitated with Protein G Sepharose and analyzed by 10% SDS-PAGE followed by autoradiography
In vivo plasma half-life and biological activityAs HMAb m102.4 has the potential to be a potent henipavirus therapeutic agent, we next assessed its in vivo half-life and toxicity. We chose to use ferrets for these studies because they have been shown to be susceptible to NiV-mediated disease (K. Bossart, J. Bingham, and D. Middleton; unpublished data) and have become important animal models for several other human respiratory viruses, including SARS coronavirus and highly pathogenic avian influenza virus. Ferrets received 1 of 2 different doses of m102.4 (25 or 5 mg), as detailed above. Animals were closely observed for at least 2 hours after recovery, and no adverse effects were noted. Blood samples were collected over a 42-day period, and antibody concentrations were measured. A typical antibody concentration over time is shown in figure 6, which shows 2 slopes in a logarithmic scale. Half-lives calculated from these slopes did not vary with antibody dose. Average distribution and elimination half-lives of 1.48 days and 3.53 days, respectively, were calculated, with relatively small individual differences. To determine whether the relatively short elimination half-life was the result of immune responses, we tested the ferret serum for anti-m102.4 ferret antibodies. We were not able to detect such antibodies in ferret serum samples after administration of m102.4 (data not shown)
Fig. 6.
Pharmacokinetics of m102.4 in ferret plasma. Solid circles experimental data for 1 ferret. The continuous lines are the best fits to straight lines in the logarithmic scale of the first 4 and last 4 experimental points
To demonstrate that m102.4 measured in plasma was biologically active, serum collected on days 1, 4, and 8 was evaluated using virus neutralization assays, as described above (data not shown). Importantly, for all ferrets, NiV was completely neutralized by 1:5 diluted serum collected on day 1 after antibody administration. When serum samples collected on day 8 were assayed, 2 samples demonstrated complete virus neutralization, and a third serum sample demonstrated 50% neutralization. Although negative on day 8, the fourth serum sample showed 50% neutralization on day 4. Taken together, these data demonstrate that m102.4 can remain biologically active in vivo for at least 8 days
Discussion
The major finding of this study is the identification of a novel, exceptionally potent, cross-reactive neutralizing HMAb, m102.4. This antibody has significantly improved potency, compared with the parent antibody m102 and with other HMAbs identified and characterized in our previous study [13]. Importantly, the substantial gain in potency was achieved without decreasing cross-reactivity. To our knowledge, this is the first fully human antibody that is capable of potently neutralizing both infectious HeV and NiV. An interesting observation made during the present study was that m102.4 had better binding to sGNiV than to sGHeV, despite the fact that sGHeV was used as the selector antigen during the original library screening [13] and in the maturation panning procedures. The better binding to sGNiV correlated with better neutralizing activity against NiV, compared with HeV. Further studies are required to understand the mechanism underlying this unexpected observation
Although the epitope mapping by alanine-scanning mutagenesis indicated that m102.4 and m101 share most of the residues on the HeV G glycoprotein that affect their binding, a dramatic difference was observed for the K560A mutation, which completely abolished the binding of m101 to HeV G, but did not affect m102.4’s binding. It was previously shown by Bishop et al. [15] that K560A had no effect on the binding of HeV G to the henipavirus receptors ephrin-B2 and ephrin-B3. Thus, the m101 epitope may contain contact site(s) located outside the receptor binding site. Because the m102.4 epitope does not include this site, one could hypothesize that it overlaps the receptor binding site to larger extent than the m101 epitope does. Such a hypothesis is in agreement with m102.4’s much higher observed degree of cross-reactivity, compared with that of m101. Thus, one could further hypothesize that the m102.4 epitope closely mimics the receptor binding site and, therefore, that the generation of escape mutants in the presence of this antibody would be less likely, compared with m101 and indeed any other known HMAb. We have previously made similar observation for our potent cross-reactive neutralizing HMAb m396, which is predicted to be effective against all SARS coronavirus isolates with known sequences [17]. The m396 binding site overlaps extensively with the receptor binding site on the SARS coronavirus spike (S) glycoprotein, as shown by the crystal structure of the m396-S complex [18]. Thus, targeting the conserved and functionally important receptor binding site that is critical for virus entry into cells is a promising strategy for the development of cross-neutralizing antibodies
The IgG1 m102.4 was well tolerated in ferrets, and no any adverse effects were noted for the relatively short time (42 days) of the experiment. The antibody pharmacokinetics consisted of 2 phases. The estimated distribution half-life of 1.5 days is typical for IgGs. The elimination half-life was significantly shorter than that for human IgGs in humans (typically 2–3 weeks). We hypothesized that this could be the results of immune responses, specifically the elicitation of anti-human IgG antibodies, which typically develop after 1–2 weeks. However, our attempts to detect such ferret antibodies against m102.4 did not result in any measurable quantities above the background (data not shown). This could be because of the low levels of such antibodies during the relatively short period of observation. Further studies are required to clarify the answer to this question
We also found that m102.4 demonstrates reasonable stability and retains its biological activity in vivo. It has been previously shown that serum from hamsters immunized with vaccinia viruses that expressed NiV envelope glycoproteins can protect the animals from challenge with NiV [19]. This important study by Guillaume et al. [19] further supports the notion that biologically active m102.4 would be able to protect animals and humans from henipavirus infections
In summary, m102.4 appears to be close to an ideal candidate for further development into an immunotherapeutic agent for henipavirus infection because it possesses many of the properties desired in such a therapeutic modality. It is a fully human MAb; it retains its biological activity in vivo; it does not cause toxicity in ferrets; it has a distribution half-life typical for IgGs, and its elimination half-life is likely to be significantly longer in humans; it cross-neutralizes both HeV and NiV; it has a much-improved potency, compared with m102, its parental antibody; and it targets the G glycoprotein region, which largely overlaps with the receptor binding site. This MAb may also prove useful in the development of diagnostics, small molecule drugs, and vaccines, and as a research reagent
Acknowledgments
We wish to thank Tim Hancock from the Australian Animal Health Laboratory for his help with the in vivo ferret work
Footnotes
Potential conflicts of interest: none reported
Financial support: National Institutes of Health (NIH) intramural biodefense program (to D.S.D.) and Middle Atlantic Regional Center of Excellence for Biodefense and Emerging Infectious Disease Research (NIH grants AI057168 and AI054715 to C.C.B.). This project has been funded in whole or in part with federal funds from the National Cancer Institute, NIH (contract N01-CO-12400). This research was supported in part by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government
Present affiliation: Profectus BioSciences, Inc., Techcenter at University of Maryland, Baltimore County, Baltimore, Maryland
References
- 1.Eaton BT, Broder CC, Middleton D, Wang LF. Hendra and Nipah viruses: different and dangerou. Nat Rev Microbiol. 2006;4:23–35. doi: 10.1038/nrmicro1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray K, Selleck P, Hooper P, et al. A morbillivirus that caused fatal disease in horses and human. Science. 1995;268:94–7. doi: 10.1126/science.7701348. [DOI] [PubMed] [Google Scholar]
- 3.Chua KB, Bellini WJ, Rota PA, et al. Nipah virus: a recently emergent deadly paramyxoviru. Science. 2000;288:1432–5. doi: 10.1126/science.288.5470.1432. [DOI] [PubMed] [Google Scholar]
- 4.Hsu VP, Hossain MJ, Parashar UD, et al. Nipah virus encephalitis reemergence, Banglades. Emerg Infect Dis. 2004;10:2082–7. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halpin K, Hyatt AD, Plowright RK, et al. Emerging viruses: coming in on a wrinkled wing and a praye. Clin Infect Dis. 2007;44:711–7. doi: 10.1086/511078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Enserink M. Emerging infectious diseases. Nipah virus (or a cousin) strikes agai. Science. 2004;303:1121. doi: 10.1126/science.303.5661.1121b. [DOI] [PubMed] [Google Scholar]
- 7.Butler D. Fatal fruit bat virus sparks epidemics in southern Asi. Nature. 2004;429:7. doi: 10.1038/429007b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu VP, Hossain MJ, Parashar UD, et al. Nipah virus encephalitis reemergence, Banglades. Emerg Infect Dis. 2004;10:2082–7. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nipah virus outbreak(s) in Bangladesh, January-April 2004. Wkly Epidemiol Rec. 2004. pp. 168–71. [PubMed]
- 10.Gurley ES, Montgomery JM, Hossain MJ, et al. Person-to-person transmission of Nipah virus in a Bangladeshi communit. Emerg Infect Dis. 2007;13:1031–7. doi: 10.3201/eid1307.061128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu H, Pfarr DS, Tang Y, et al. Ultra-potent antibodies against respiratory syncytial virus: effects of binding kinetics and binding valence on viral neutralizatio. J Mol Biol. 2005;350:126–44. doi: 10.1016/j.jmb.2005.04.049. [DOI] [PubMed] [Google Scholar]
- 12.Bossart KN, Crameri G, Dimitrov AS, et al. Receptor binding, fusion inhibition, and induction of cross-reactive neutralizing antibodies by a soluble G glycoprotein of Hendra viru. J Virol. 2005;79:6690–702. doi: 10.1128/JVI.79.11.6690-6702.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu Z, Dimitrov AS, Bossart KN, et al. Potent neutralization of Hendra and Nipah viruses by human monoclonal antibodie. J Virol. 2006;80:891–9. doi: 10.1128/JVI.80.2.891-899.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bonaparte MI, Dimitrov AS, Bossart KN, et al. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah viru. Proc Natl Acad Sci U S A. 2005;102:10652–7. doi: 10.1073/pnas.0504887102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bishop KA, Stantchev TS, Hickey AC, et al. Identification of Hendra virus G glycoprotein residues that are critical for receptor bindin. J Virol. 2007;81:5893–901. doi: 10.1128/JVI.02022-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bossart KN, McEachern JA, Hickey AC, et al. Neutralization assays for differential henipavirus serology using Bio-Plex protein array system. J Virol Methods. 2007;142:29–40. doi: 10.1016/j.jviromet.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Zhu Z, Chakraborti S, He Y, et al. Potent cross-reactive neutralization of SARS coronavirus isolates by human monoclonal antibodie. Proc Natl Acad Sci U S A. 2007;104:12123–8. doi: 10.1073/pnas.0701000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prabakaran P, Gan J, Feng Y, et al. Structure of severe acute respiratory syndrome coronavirus receptor-binding domain complexed with neutralizing antibod. J Biol Chem. 2006;281:15829–36. doi: 10.1074/jbc.M600697200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guillaume V, Contamin H, Loth P, et al. Nipah virus: vaccination and passive protection studies in a hamster mode. J Virol. 2004;78:834–40. doi: 10.1128/JVI.78.2.834-840.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]