To the editor,
It has been recently shown with clinical studies that COVID-19 pathogenesis is associated with coagulopathy, however it differs from sepsis associated disseminated intravascular coagulation (DIC) with relatively normal levels of PT, fibrinogen and platelets, despite markedly elevated d-dimer levels [1–3]. Although the primary pathogenesis was thought as pulmonary type II pneumocyte injury, viral pneumonia, acute respiratory distress syndrome (ARDS) or macrophage activating like syndrome complicating ARDS leading to DIC, the pathological evidence from autopsy series show that the major pathogenic mechanism is ‘Pulmonary Intravascular Coagulopathy-PIC’ as firstly named by McGonagle et al. [4] which is a kind of immune thrombosis that is distinct from classical DIC [4]. Pathological findings indicate that the lungs are oedematous with patchy haemorrhage are as macroscopically with diffuse alveolar damage and extensive fibrin thrombi in distended small vessels and capillaries. The presentation of numerous megakaryocytes stained with CD61 and von Willebrand Factor further supports the hypothesis of local coagulation is the main factor of the whole process [5].
The gross pathological findings of the heart at the same study showed extreme right ventricular dilatation and straining of the interventricular septum as an evidence of right cardiac insufficiency caused by pulmonary hypertension. Another paper that gave us early pathological findings of two patients with lung cancer who were biopsied for their malignancy before they were symptomatic for COVID-19 and revealed early pathological signs of COVID-19 besides adeno carcinoma in biopsies.[6]. Those signs were intra-alveolar fibrin with early organization, proteinaceous exudates in alveoli and mono nuclear inflammatory cells suggesting early start of coagulopathy even when patients were asymptomatic. As PIC is the first step of the disease, the patients fail to respond to classical treatment modalities targeting pulmonary oedema, ARDS and MAS with cytokine storm. The cytokine storm is interpreted as capillary leak syndrome and treatment modalities like IVIG, steroid and anti-IL6, plasma exchange usually fails to manage the clinical picture. Here we provide possible mechanism and treatment strategy for COVID-19 PIC.
Possible pathogenesis and treatment strategy
SARS-CoV2 binds to ACE2 receptors on type II pneumocytes and possibly on vascular endothelial cells and causes lysis of the cells immediately leading to direct activation of the endothelium causing procoagulant activity and activates accumulation of fibrin deposits in pulmonary microcapillary venous vessels. The fibrin deposits cause a compensatory mechanism of increased plasminogen at the beginning but as the disease progresses fail to break down the fibrin deposits reflected in increased d-dimer levels. The treatment strategy at this level should be blockage of hyper coagulation with low molecular weight heparin (LMWH) as mentioned by Thachil [1] for blocking thrombin and dampen the inflammatory response. LMWH at prophylactic doses should be administered to all symptomatic patients with microbiologically or radiologically documented COVID-19 diagnosis and escalated to therapeutic doses in case of respiratory distress.
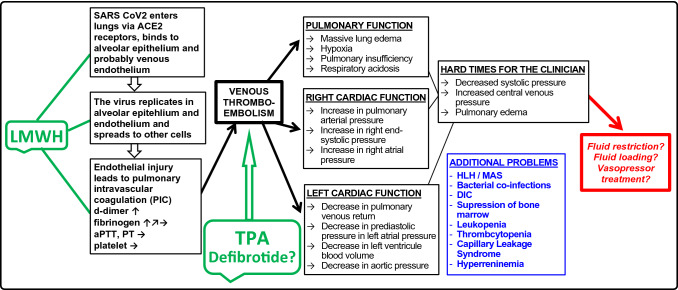
In case LMWH is insufficient of preventing further activation of PIC and the thromboses extend to pulmonary veins, the process will proceed to secondary pulmonary hypertension and cardiac insufficiency. Increased intravascular pressure in lungs will result in extensive alveolar exudation resulting causing marked hypoxia. As a consequence of decreased pulmonary venous flow, the left ventricular stroke volume will decrease leading to systemic hypotension. The treatment option at this step should be Tissue Plasminogen Activator (TPA) or defibrotide. These two fibrinolytic modalities can prevent intubation and progression to DIC (Fig. 1). Plasminogen and TPA has been used in COVID-19 patients in a few studies and have been shown to be beneficial in improving respiratory capacity [7, 8]. As the immune-pathogenesis seems to resemble endothelial dysfunction of sinusoidal obstruction syndrome we think that defibrotide can also be useful or its pro-fibrinolytic, antithrombotic, thrombolytic, anti-ischemic and anti-inflammatory functions that may help to restore the endothelial function [9]. According to the previous literature, we think the major pathogenesis of COVID-19 disease starts with hyper coagulation and PIC. We believe that early anticoagulation and early thrombolytic agents may provide better prognosis in these patients.
Fig. 1.
The possible pathogenesis of COVID-19. TPA tissue plasminogen activator, aPTT activated partial thromboplastin time, PT prothrombin time, HLH hemophagocytic lymphohistiocytosis, MAS macrophage activating syndrome, LMWH low molecular weight heparin
Funding
The authors did not receive any funding for the manuscript.
Compliance with ethical standards
Conflict of interest
The authors FBBA and FS declare no conflict of interest.
Consent to participate
The authors participated together to the hypothesis and writing of the letter.
Consent for publication
The authors FBBA and FS both give permission for publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
F. Burcu Belen-Apak and F. Sarıalioğlu have contributed equally to the manuscript.
References
- 1.Thachil J. The versatile heparin in COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGonagle D, O’Donnell JS, Sharif K, Emery P, Bridgewood C. Why the immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia are distinct from macrophage activation syndrome with disseminated Intravascular coagulation. Autoimmun Rev. 2020 doi: 10.1016/j.autrev.2020.102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fox SE, Akmatbekov A, Harbert JL, Li G, Brown Q, Vander Heide RS. Pulmonary and cardiac pathology in Covid-19: the first autopsy series from New Orleans. MedRxiv. 2020 doi: 10.1101/2020.04.06.20050575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tian S, Hu W, Niu L, Liu H, Xu H, Xiao Y. Pulmonary pathology of early-phase, 2019 novel Coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020 doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore H, Barrett CD, Moore EE, McIntyre RC, Moore PK, Talmar DS, Moore FA, Yaffe MB. Is there a role for plasminogen activator (tPA) as a novel treatment for refractory COVID-19 associated with acute respiratory distress syndrome (ARDS)? J Trauma Acute Care Surg. 2020 doi: 10.1097/TA.0000000000002694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu T, Wang T, Guo C, Zhang D, Ge X, Huang Z, Zhou X, Li Y, Peng Q, Li J. Plasminogen improves lung lesions and hypoxemia in patients with COVID-19. QJM. 2020 doi: 10.1093/qjmed/hcaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pescador R, Capuzzi L, Mantovani M, Fulgenzi A, Ferrero ME. Defibrotide: properties and clinical use of an old/new drug. Vascul Pharmacol. 2013;59:1–10. doi: 10.1016/j.vph.2013.05.001. [DOI] [PubMed] [Google Scholar]