Abstract
Background
Thyroid nodules are a common pathology worldwide. Fine needle aspiration biopsy (FNAB) is an important diagnostic method for the investigation of malignancy in thyroid nodules. However, according to the Bethesda System used to classify the results, patients with atypia of undetermined significance/follicular lesion of undetermined significance (AUS / FLUS) may not be classified as benign or malignant. Therefore, it may be necessary to determine some clinical risk factors to apply the best treatment in these patients.
Aim
To determine the factors that increase the risk of malignancy in this patient group.
Methods
A retrospective study including 138 patients with an FNAB categorized as AUS/FLUS and operated between June 2015–September 2018. Demographical, Laboratory (TSH) and Ultrasound variables (number, size and characteristics of nodules) of the patients were compared among postoperative histopathological results.
Results
Hypo-echoic structure, microcalcification and irregular margin of the nodules were detected to be associated with malignancy in patients with FNAB results of AUS/FLUS (p <0.001).
Conclusion
We suggest that surgical treatment should be considered if the patients have nodules with the hypo-echoic structure, microcalcification and irregular margin with an FNAB histopathological result of AUS / FLUS.
Keywords: Atypia of undetermined significance/follicular lesion of undetermined significance, Fine needle aspiration biopsy, Malignancy, Thyroid nodule
INTRODUCTION
Thyroid nodule refers to an abnormal growth of thyroid cells that forms a lump within the thyroid gland. The incidence of thyroid nodules in the general population is high. By age 60, about one-half of all people have a thyroid nodule that can be found either through examination or with imaging. They are detected by palpation at a rate of 2-6% and with high resolution US at 50-70% (1, 2). However, the incidence of malignancy in these nodules is lower and varies between 5 and 15% (3, 4).
Fine needle aspiration biopsy (FNAB) used to investigate malignancy in thyroid nodules is a reliable, technically straightforward and inexpensive method (5). On October 22 and 23, 2007, the National Cancer Institute (NCI) hosted “The NCI Thyroid Fine Needle Aspiration (FNA) State of the Science Conference”, a two-day gathering in Bethesda, Maryland. They determined criteria named as The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) at this meeting to interpret the results after FNAB and to make recommendations about patient management (6). The results of FNAB are evaluated in 6 categories according to Bethesda system. However, the Bethesda Category III (AUS / FLUS) in this reporting system is inadequate in the differential diagnosis of benign-malignant nodule and thus provides a significant limitation (5). The predicted malignancy rate for patients in this group ranges from 5% to 15% (7). However, some studies have reported rates from 6% to 48% (8-10). Due to the different malignancy rates in these patients, the management strategy is still a matter of debate and it is difficult to predict the true malignancy rate except for those who are operated. Although it is recommended to take some clinical factors into account to avoid unnecessary surgeries and also to avoid the being overlooked of malignancy, no specific clinical factor has been shown to date (11).
In this study, we aimed to determine the clinical factors that will help us predict the risk of malignancy in this group of patients and to find the parameters that will help to eliminate the problems related with insufficient and unnecessary surgery.
PATIENTS AND METHODS
We reviewed retrospectively the data on 138 AUS/FLUS patients who underwent surgery and had a histopathological diagnosis at the general surgery clinic of the University of Health Science Hamidiye Etfal Training and Research Hospital between June 2015 and September 2018. The study protocol was approved by the institutional review board and ethics committee of University of Health Science Hamidiye Etfal Training and Research Center (No:1115/2018).
During the examination of the patients; age, family history of thyroid disease, history of head and neck radiation, a mass in the neck, presence of pain at the base of neck, hoarse voice, swallowing and breathing difficulties, presence of symptoms of hypo-hyperthyroidism (irregular heartbeat, unexplained weight loss or weight gain, nervousness or fatigue, dry skin or hair) and use of iodine-containing drug were recorded from patient files. Physical examination, vocal cord examination, neck US, thyroid function tests and FNAB results of all patients were recorded from patient files. Patients who had a personal or familial history of cancer, history of radiation applied to the head and neck region, history of thyroid hormone therapy, history of thyroid surgery and the patients whose file could not be retrieved from the clinic records were excluded from the study. A number of 138 patients who met the criteria of our study were included. Age, gender, Thyroid Stimulating Hormone (TSH) results, ultrasonographic nodule characteristics, operation type and pathology results were recorded.
All patients were examined in supine position with hyperextended neck. Ultrasound examinations were performed with Esaote MyLab 60 system using linear transducer: 4–13 MHz (Esaote SpA, Italy). Patients were questioned about anticoagulant and antiaggregant usage before biopsy procedure. The dimensions and the ultrasonographic characteristics of the each nodule were evaluated and reported before the biopsy procedure. Povidoneiodine solution was used for skin sterilization. Biopsy was performed with a 23-gauge needle affixed to a commercially available 10-mL syringe. The biopsy technique involved a minimum of 2 passes from different parts of the nodule.
Correlation of characteristic features (size, margin, nodule specification, echogenicity, presence of calcification and loss of halo) of the nodules and histopathological results were examined. The term solid was used for nodules with at least 90% solid component, and hypo-echogenic was used for nodules hypo-echogenic compared to normal thyroid parenchyma. Irregular margin was described as microlobulated or spiculated in appearance and demarcation between the tumour and the surrounding normal glandular parenchyma is indistinct. While micro-calcification was the term used for 1mm or less small flecks of calcification that appear bright on an ultrasound image, loss of thin or thick hypo-echoic margin surrounding the nodule is defined as a loss of halo (12).
The ultrasound-guided FNAB indication of thyroid nodules was based on the 2015 ATA guidelines: 1) High suspicious nodule with a diameter of 5-10 mm, 2) Intermediate suspicious nodule with a diameter greater than 10 mm and 3) low suspicious nodule with a diameter greater than 15mm (5). A 23-gauge 10 mL syringe was used for the FNAB and the aspirates were dried in air (aspiration material was fixed with 95% ethanol and stained with either hematoxylin and eosin or Papanicolaou and May Grunwald and Giemsa stain). Cytological evaluation of lesions in Category III (AUS / FLUS) was performed according to the 2007 Bethesda Thyroid Cytopathology Reporting System (6).
Patients with large nodular goiter, suspicious US features and also patients who prefered surgery were operated (5). Repeat FNAB under ultrasound guidance was performed in the remaining 99 patients and those with two consecutive AUS/FLUS results were treated surgically.
The results were analyzed using SPSS version 15.0 (Statistical Package for the Social Sciences Inc, Chicago, USA). Numerical variables were expressed as the mean ± standard deviation (SD) or minimum and maximum while categorical variables were presented as absolute values and percentages. Differences between continuous and categorical variables were assessed by the Mann-Whitney U test for non-normally distributed variables. The relationships between continuous variables (i.e., age, size of nodule) and final pathologic results were analyzed by t-test. Multivariate logistic regression with a backward stepwise variable selection procedure was performed to identify variables associated with an increased risk of malignancy. Variables associated with malignancy with a P<0.10 in the univariate analysis entered the multivariate model, and nonsignificant variables were removed by means of a backward-selection procedure. The chi-square statistics was used to analyze group differences. A p<0.05 was considered statistically significant and 95% confidence intervals (CIs; for adjusted odds ratios [ORs]) were calculated to assess the precision of the obtained estimates.
RESULTS
In this study the ratio of AUS/FLUS results to other FNAB results was found 12% (285/2370). Of these patients, 137 were excluded from the study due to 59 of them not being AUS/FLUS after the repeat FNAB and 78 of them being lack of follow-up data. The results of the second FNA of these 59 patients were categorized as follows: 61% (n=36) in benign, 13.5% (n=8) in non-diagnostic categories and 25.4% (n=15) in follicular neoplasm, suspicious malignant, or malignant. Ten of the remaining patients were taken to the follow-up at the outpatient clinic in line with their preference. Being 98 of them after the first FNAB, and 40 of them after repeat FNAB, a total number of 138 patients were treated by surgery (Fig. 1). Lobectomy was performed in 40.6% (n=56) of the patients and total thyroidectomy in 59.4% (n=82).
Figure 1.
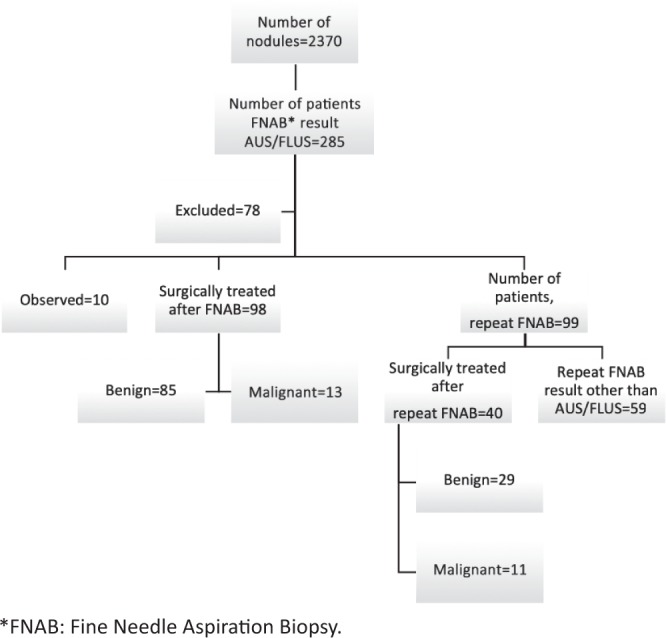
Management of thyroid nodules.
The mean age of the patients was 46.8±14.2 (min-max=20-78) years; 84.1% (n=116) were female and 15.9% (n=22) were male. The rate of malignancy in AUS/FLUS reported lesions was detected in 17.3% (24/138) and the mean tumor diameter in these patients was 13.7±6.9 (min-max=3-30) mm. The mean nodule diameter of the patients was 23.1±10.5 (min-max=8-61) mm and there was no statistically significant difference between the groups (p=0.228). No statistical significance was found between the benign and malignant groups in terms of age and sex (Table 1).
Table 1.
The characteristics of patients
| Total | Benign | Malignant | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p | ||
| Sex | Male | 22 | 15.9 | 15 | 13.2 | 7 | 29.2 | 0.066 |
| Female | 116 | 84.1 | 99 | 86.8 | 17 | 70.8 | ||
| Age (years) | 46.8±14.2 (20-78) |
47.8±14.1 (20-78) |
45.3±14.9 (24-78) |
0.489 | ||||
| Thyroid-stimulating hormone (mIU/L) | ≤1 | 40 | 29.0 | 34 | 29.8 | 6 | 25.0 | 0.321 |
| 1-5 | 90 | 65.2 | 72 | 63.2 | 18 | 75.0 | ||
| >5 | 8 | 5.8 | 8 | 7.0 | 0 | 0.0 | ||
| Localization of nodule | Left | 76 | 55.1 | 65 | 57.0 | 11 | 45.8 | 0.317 |
| Right | 62 | 44.9 | 49 | 43.0 | 13 | 54.2 | ||
| Number of nodules | Single | 32 | 23.7 | 26 | 23.4 | 6 | 25.0 | 0.869 |
| Multiple | 103 | 76.3 | 85 | 76.6 | 18 | 75.0 | ||
| Size of nodule (mm) | 23.1±10.5 (8-61) |
23.7±11.0 (8-61) |
20.2±7.5 (9-35) |
0.228 | ||||
| Operation | Right lobectomy | 21 | 15.2 | 19 | 16.7 | 2 | 8.3 | |
| Left lobectomy | 35 | 25.4 | 31 | 27.2 | 4 | 16.7 | ||
| Total thyroidectomy | 82 | 59.4 | 64 | 56.1 | 18 | 75.0 | ||
| Diameter of tumor (mm) | 13.7±6.9 (3-30) |
|||||||
| Localization of tumor | Multicentric | 6 | 25.0 | |||||
| Right | 12 | 50.0 | ||||||
| Left | 6 | 25.0 | ||||||
Histopathology results of 75% of malignant cases were reported as papillary carcinoma/micro-carcinoma, postoperatively. The most common pathology was adenomatous hyperplasia (33.3%) and adenomatous nodule (31.5%) in patients with benign pathology (Table 2). The postoperative malignity rate of patients whose FNAB result reported as AUS/FLUS, after first FNAB and repeat FNAB were detected as 13.3% and 27.5% (Table 3). While the correlation of US characteristics for hypo-echogenicity (odds ratio [OR], 5.9610; 95% confidence interval [CI], 2.2624-15.7064; p= 0.0003), irregular margin (odds ratio [OR], 10.4000; 95% confidence interval [CI], 3.7120-29.1377; p< 0.0001), and micro-calcification (odds ratio [OR], 5.0000; 95% confidence interval [CI], 1.9539-12.7951; p= 0.0008) with malignant histopathology results were significant on univariate and multivariate analyses, solid structure and loss of halo were not found to have any correlation with malignancy (Table 4).
Table 2.
Histopathological classification of nodules
| Result | n | % | |
|---|---|---|---|
| Benign | Adenomatous Hyperplasia | 38 | 33.33 |
| Adenomatous Nodule | 36 | 31.57 | |
| Nodular Hyperplasia | 21 | 18.42 | |
| Follicular Adenoma | 14 | 12.28 | |
| Hashimoto Nodule | 5 | 4.38 | |
| Malignant | Papillary Carcinoma | 13 | 54.16 |
| Papillary Microcarcinoma | 5 | 20.83 | |
| Papillary Cancer Follicular Variant | 4 | 16.66 | |
| Follicular Carcinoma | 1 | 4.16 | |
| Hurthle Cell Carcinoma | 1 | 4.16 |
Table 3.
Postoperative malignancy rate of patients whose FNAB result reported as atypia of undetermined significance/follicular lesion of undetermined significance
| Total | Benign | Malignant | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| First FNAB* | 98 | 71.1 | 85 | 86.7 | 13 | 13.3 |
| Repeat FNAB | 40 | 28.9 | 29 | 72.5 | 11 | 27.5 |
| Total | 138 | 100 | 114 | 82.6 | 24 | 17.4 |
FNAB: Fine Needle Aspiration Biopsy.
Table 4.
Relation between sonographic features of thyroid nodules and malignancy
| Total | Benign | Malignant | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p | ||
| Solid nature | Yes | 99 | 71.7 | 80 | 70.2 | 19 | 79.2 | 0.374 |
| No | 39 | 28.3 | 34 | 29.8 | 5 | 20.8 | ||
| Hypoechogenicity | Yes | 50 | 36.2 | 33 | 28.9 | 17 | 70.8 | <0.001 |
| No | 88 | 63.8 | 81 | 71.1 | 7 | 29.2 | ||
| Microcalcification | Yes | 31 | 22.5 | 19 | 16.7 | 12 | 50.0 | <0.001 |
| No | 107 | 77.5 | 95 | 83.3 | 12 | 50.0 | ||
| Irregular margin | Yes | 22 | 15.9 | 10 | 8.8 | 12 | 50.0 | <0.001 |
| No | 116 | 84.1 | 104 | 91.2 | 12 | 50.0 | ||
| Loss of halo | Yes | 67 | 48.6 | 58 | 50.9 | 9 | 37.5 | 0.233 |
| No | 71 | 51.4 | 56 | 49.1 | 15 | 62.5 | ||
DISCUSSION
In this study, some criteria for better estimation of malignancy risk in AUS/FLUS group thyroid nodules were intended to be identified and in line with these criteria to achieve better management strategies in these groups of patients was aimed. For this purpose, the clinical and ultrasonographic features of the patients with these criteria were examined. We found that hypoechogenicity, irregular margin and micro-calcification as negative US characters were strongly correlated with malignancy.
Due to the heterogeneity of the diagnosis of AUS/ FLUS, the incidence was reported in this category to be as high as 18% (13, 14). The rate of AUS/FLUS lesions in this study was 12% among all. The cellular architecture and the rate of nuclear atypia of nodules reported as AUS / FLUS are not sufficient for the diagnosis of malignancy or follicular neoplasia (7). AUS/FLUS is a challenging cytological diagnosis and difficult to lead to clinical decision. Results from different institutions have different malignancy rates (13, 14). Therefore, using more experienced cytopathologists is likely to be associated with lower rates of AUS/FLUS and a lower number of unnecessary surgeries. The rate of malignancy predicted by TBSRTC for patients in this group ranges from 5% to 15% (7).
Although the approach to these nodules is controversial, clinical correlation and molecular tests have been recommended, in particular the repeat FNAB (5, 7, 15). However, clinicians may also recommend surgical treatment based on clinical and US findings to the patient rather than the repeat of FNAB (6). 2015 ATA guideline suggested that following the evaluation of clinical and sonographic features for AUS/FLUS reported nodule, repeat FNAB or molecular tests are recommended to support malignancy risk assessment rather than direct surgical treatment (5). However, in the further recommendations, it is stated that if the repeat FNAB, molecular test or both cannot be performed, follow-up or surgery can be performed depending on clinical risk factors, US characteristics and patient preference (5). Some studies have shown that two consecutive AUS/FLUS diagnosed nodules have at least 30% higher malignancy risk than the single FNAB (9, 16, 17). In this study, the overall malignancy rate of nodules with AUS/FLUS was 17.4%. Among these patients, the malignancy rate of the nodules with AUS / FLUS after repeated FNAB was found to be 27.5% (Table 3) and these findings are in line with the literature. In some studies, there was no statistical difference in terms of malignancy rate for AUS/FLUS either first FNAB or repeat FNAB and they suggested that to repeat FNAB or to perform surgery should be under clinicians decision (9, 14, 18, 19). We recommend that repeating the FNAB should always be kept in mind, due to the higher rate of malignancy in the group that had repeated FNAB for AUS/FLUS.
In some previous studies on this subject, it was stated that irregular margin, hypoechogenicity, micro-calcification, height to width ratio, the increase in vascularization, nodule size and also the age can be used for the prediction of malignancy in these patients (20- 22). In this study, age, gender, thyroid hormone level, number and size of nodules were not found to be related with malignancy risk. Hong SH et al. found that malignant nodules were significantly larger in AUS/FLUS than in benign nodules, and therefore they suggested that clinicians should prefer thyroidectomy rather than repeat FNAB on larger nodules (19). In this study, rates of hypoechogenicity, micro-calcification and irregular margin of the nodules were significantly higher in the malignant group than in the benign group (p<0.001). A similar study conducted by Kuru et al. suggested that microcalcification, solid structure, hypoechogenicity, irregular margins and increased vascularity of nodules were found to be related with malignancy and surgical treatment should be considered in these patients (23). Hong MJ et al. recommends surgical treatment for nodules with intermediate or high ultrasonographic characters (Korean Thyroid Imaging Reporting and Data System 4 or 5) instead of repeat FNAB and reported the malignancy rate in these patients in the range of 30% to 90% (24). The recommended surgical method should be lobectomy in these patients (5). However, this approach can be changed according to clinical or ultrasonographic characteristics, patient preference and molecular test results (5).
Our study has certain limitations. All work was performed at a single center. The work was retrospective in nature, and anterior-posterior nodule size records were lacking. Also, molecular tests were not performed to assess the risk of malignancy in patients with AUS / FLUS group. Thus, additional multicenter prospective studies with more patients are warranted.
In conclusion, this study clearly stated that hypoechogenicity, irregular margin and microcalcification of nodules in AUS/FLUS group were strongly associated with malignancy. We suggest that surgical treatment should be considered in the nodules to which FNAB result, reported as AUS/FLUS, includes these US characteristics. We believe that further studies on the molecular basis of this patient group will provide more help in the decision-making process.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Hegedus L. Clinical practice. The thyroid nodule. N Engl J Med. 2004;351(17):1764–1771. doi: 10.1056/NEJMcp031436. [DOI] [PubMed] [Google Scholar]
- 2.Guth S, Theune U, Aberle J, Galach A, Bamberger CM. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest. 2009;39:699–706. doi: 10.1111/j.1365-2362.2009.02162.x. [DOI] [PubMed] [Google Scholar]
- 3.Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, Panunci C, Rinaldi R, Toscano V, Pacella CM. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002;87:1941–1946. doi: 10.1210/jcem.87.5.8504. [DOI] [PubMed] [Google Scholar]
- 4.Nam-Goong IS, Kim HY, Gong G, Lee HK, Hong SJ, Kim WB, Shong YK. Ultrasonography-guided fine-needle aspiration of thyroid incidentaloma: correlation with pathological findings. Clin Endocrinol (Oxf) 2004;60:21–28. doi: 10.1046/j.1365-2265.2003.01912.x. [DOI] [PubMed] [Google Scholar]
- 5.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Stewart DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–33. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cibas ES, Ali SZ, NCI Thyroid FNA State of the Science Conference The Bethesda System for Reporting Thyroid Cytopathology. Am J Clin Pathol. 2009;132(5):658–665. doi: 10.1309/AJCPPHLWMI3JV4LA. [DOI] [PubMed] [Google Scholar]
- 7.Cibas ES, Ali SZ. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid. 2017;27(11):1341–1346. doi: 10.1089/thy.2017.0500. [DOI] [PubMed] [Google Scholar]
- 8.Bongiovanni M, Crippa S, Baloch Z, Piana S, Spitale A, Pagni F, Mazzucchelli L, Di Bella C, Faquin W. Comparison of 5-tiered and 6-tiered diagnostic systems for the reporting of thyroid cytopathology: a multi-institutional study. Cancer Cytopathology. 2012;120(2):117–125. doi: 10.1002/cncy.20195. [DOI] [PubMed] [Google Scholar]
- 9.Park VY, Kim EK, Kwak JY, Yoon JH, Moon HJ. Malignancy risk and characteristics of thyroid nodules with two consecutive results of atypia of undetermined significance or follicular lesion of undetermined significance on cytology. European Radiology. 2015;25(9):2601–2607. doi: 10.1007/s00330-015-3668-5. [DOI] [PubMed] [Google Scholar]
- 10.Ho AS, Sarti EE, Jain KS, Wang H, Nixon IJ, Shaha AR, Shah JP, Kraus DH, Ghossein R, Fish SA, Wong RJ, Lin O, Morris LGT. Malignancy rate in thyroid nodules classified as Bethesda category III (AUS/FLUS) Thyroid. 2014;24(5):832–839. doi: 10.1089/thy.2013.0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiseman SM, Baliski C, Irvine R, Anderson D, Wilkins G, Filipenko D, Zhang H, Bugis S. Hemithyroidectomy: the optimal initial surgical approach for individuals undergoing surgery for a cytological diagnosis of follicular neoplasm. Ann Surg Oncol. 2006;13:425–432. doi: 10.1245/ASO.2006.03.089. [DOI] [PubMed] [Google Scholar]
- 12.Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, Lim HK, Moon WJ, Na DG, Park JS, Choi YJ, Hahn SY, Jeon SJ, Jung SL, Kim DW, Kim EK, Kwak JY, Lee CY, Lee HJ, Lee JH, Lee KH, Park SW, Sung JY, Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology Ultrasonography Diagnosis and Imaging-Based Management of Thyroid Nodules: Revised Korean Society of Thyroid Radiology Consensus Statement and Recommendations. Korean J Radiol. 2016;17(3):370–395. doi: 10.3348/kjr.2016.17.3.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nayar R, Ivanovic M. The indeterminate thyroid fine needle aspiration: experience from an academic center using terminology similar to that proposed in the 2007 National Cancer Institute Thyroid Fine Needle Aspiration State of the Science Conference. Cancer. 2009;117:195–202. doi: 10.1002/cncy.20029. [DOI] [PubMed] [Google Scholar]
- 14.VanderLaan PA, Marqusee E, Krane JF. Clinical outcome for atypia of undetermined significance in thyroid fine-needle aspirations: should repeated FNA be the preferred initial approach? Am J Clin Pathol. 2011;135:770–775. doi: 10.1309/AJCP4P2GCCDNHFMY. [DOI] [PubMed] [Google Scholar]
- 15.Layfield LJ, Abrams J, Cochand-Priollet B, Evans D, Gharib H, Greenspan F, Henry M, LiVolsi V, Merino M, Michael CW, Wang H, Wells SA. Post-thyroid FNA testing and treatment options: a synopsis of the National Cancer Institute Thyroid Fine-Needle Aspiration State of the Science Conference. Diagn Cytopathol. 2008;36:442–448. doi: 10.1002/dc.20832. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan PS, Hirschowitz SL, Fung PC, Apple SK. The impact of atypia/follicular lesion of undetermined significance and repeat fine-needle aspiration: 5 years before and after implementation of the Bethesda system. Cancer Cytopathol. 2014;122:866–872. doi: 10.1002/cncy.21468. [DOI] [PubMed] [Google Scholar]
- 17.Kuru B, Atmaca A, Kefeli M. Malignancy rate associated with Bethesda category III (AUS/FLUS) with and without repeat fine needle aspiration biopsy. Diagn Cytopathol. 2016;44:394–398. doi: 10.1002/dc.23456. [DOI] [PubMed] [Google Scholar]
- 18.Jan IS, Lee YT, Wang CM, Cheng TY, Wang CY, Chang TC, Shih SR. The surgery and repeat aspiration outcomes of the atypia of undetermined significance/ follicular lesion of undetermined significance category in The Bethesda System for Reporting Thyroid Cytopathology. Asian Journal of Surgery. 2018 doi: 10.1016/j.asjsur.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Hong SH, Lee H, Cho MS, Lee JE, Sung YA, Hong YS. Malignancy Risk and Related Factors of Atypia of Undetermined Significance/Follicular Lesion of Undetermined Significance in Thyroid Fine Needle Aspiration. International Journal of Endocrinology vol. 2018. 2018 doi: 10.1155/2018/4521984. Article ID 4521984, 7 pages, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gweon HM, Son EJ, Youk JH, Kim JA. Thyroid nodules with Bethesda system III cytology: can ultrasonography guide the next step? Ann Surg Oncol. 2013;20:3083–3088. doi: 10.1245/s10434-013-2990-x. [DOI] [PubMed] [Google Scholar]
- 21.Sippel RS, Elaraj DM, Khanafshar E, Kebebew E, Duh QY, Clark OH. Does the presence of additional thyroid nodules on ultrasound alter the risk of malignancy in patients with a follicular neoplasm of the thyroid? Surgery. 2007;142:851–857. doi: 10.1016/j.surg.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Ryu YJ, Jung YS, Yoon HC, Hwang MJ, Shin SH, Cho JS, Lee JS, Kim HK, Kang HC, Lim HS, Yoon JH, Park MH. Atypia of undetermined significance on thyroid fine needle aspiration: surgical outcome and risk factors for malignancy. Ann Surg Treat Res. 2014;86:109–114. doi: 10.4174/astr.2014.86.3.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuru B, Atmaca A, Tarim IA, Kefeli M, Topgul K, Yoruker S, Elmali M, Danaci M. Risk factors associated with malignancy and with triage to surgery in thyroid nodules classified as Bethesda category III (AUS/FLUS) Eur J Surg Onc. 2016;42(1):87–93. doi: 10.1016/j.ejso.2015.09.026. [DOI] [PubMed] [Google Scholar]
- 24.Hong MJ, Na DG, Baek JH, Sung JY, Kim JH. Cytology-ultrasonography risk-stratification scoring system based on fine needle aspiration cytology and the Korean-Thyroid Imaging Reporting and Data System. Thyroid. 2017;27(7):953–959. doi: 10.1089/thy.2016.0603. [DOI] [PubMed] [Google Scholar]


