Dear Editor,
In December 2019, a novel coronavirus was identified in Wuhan, China, causing an illness that resembled viral pneumonia. This virus, named severe acute respiratory syndrome coronavirus, caused the novel Coronavirus Disease 2019 (COVID-19). Patients with COVID-19 mainly present with symptoms such as fever, dyspnea and cough (1). Neurologic manifestations, although relatively uncommon, also have been reported. According to published studies, the neurologic involvement of COVID-19 mainly falls into three categories: (1) central nervous system (CNS) involvement, such as dizziness, headache, impaired consciousness, acute cerebrovascular disease, and epilepsy, (2) peripheral nervous system involvement including anosmia, hypogeusia, visual impairment, and neuralgia, and (3) skeletal muscle damage (2). Acute Necrotizing Encephalopathy, a rare complication of viral infections that is associated with intracranial cytokine storm, was recently reported in a woman with COVID-19 in the United States. The patient had presented with altered mental status and had subsequently undergone CT and MRI brain scans (3)
Neurological symptoms are often insignificant and nonspecific at the early stages of COVID-19 infection, increasing the risk of misdiagnosis and delayed management of patients (4). Also, it has been shown that major neurologic events such as ischemic stroke and cerebral hemorrhage occur more frequently in patients with severe infection (2). With disease progression, factors such as increased inflammatory cytokine production and impaired coagulation function increase the risk of cerebrovascular disease and subsequently, result in clinical deterioration and a higher mortality rate. Thus, early identification of patients with neurologic involvement is of high importance.
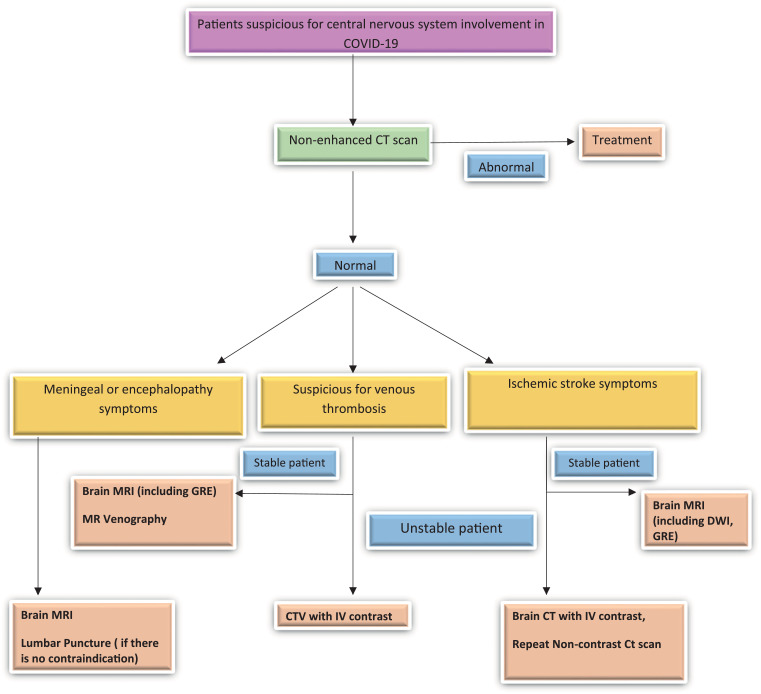
Obtaining a detailed medical history and physical examination, as well as performing imaging could help to detect neurologic manifestations in a timely manner. If a patient with suspected or proven COVID-19 presents with neurological signs or symptoms, emergency action should be taken by neurologists, radiologists, and infectious disease specialists in order to properly manage the condition. However, one of the major challenges in such conditions is to choose the most appropriate imaging modality for the diagnosis of possible COVID-19-associated neurologic complications. It is clear that neuroimaging could not be performed for all patients who present with neurologic manifestations in the current setting as performing CT/MRI examinations may pose an additional risk of infection to both patients and health care providers. Another challenging issue is the use of contrast-based radiologic imaging in COVID-19 patients. As mentioned previously, critically ill patients with severe infection are at a higher risk of developing major neurologic events. In those who are equipped with non-MR compatible supportive devices, the use of MR is very limited. Such patients are also more likely to have comorbidities such as renal failure, diabetes, and hypertension, which further limit the use of contrast media for diagnosing neurologic complications. Therefore, the need for a standard guideline on neuroimaging in COVID-19 is evident. Herein, we have proposed a flowchart for the management of patients with COVID-19 who are suspicious for CNS involvement (Fig 1 ).
Figure 1.
Flowchart of the management of patients with COVID-10 who are suspicious for CNS involvement. CVT, Cerebral Venous Thrombosis; MRV, Magnetic Resonance Venography.
The American College of Radiology (ACR) recommends the use of MR only when the results obtained from the examination potentially impact the physician's decision making in terms of patient management. Moreover, both the ACR and Centers for Disease Control and Prevention agree on the postponement of nonurgent or nonemergent imaging studies during the COVID-19 pandemic (5). In addition, unnecessary neuroimaging might cause delay in performing chest CT scans for patients with COVID-19, which currently has a higher priority in referral hospitals.
MR imaging is associated with other confrontations. For instance, the ACR advises the removal of the metal strip from surgical face masks in patients undergoing MR examinations and also the placement of a MR safe face mask over the tracheostomy in those patients with a tracheostomy (6). However, a study by Murray et al. found that the removal of the metal nosepiece from a surgical mask is not necessary prior to MR examination in patients with suspected or confirmed COVID-19 (7).
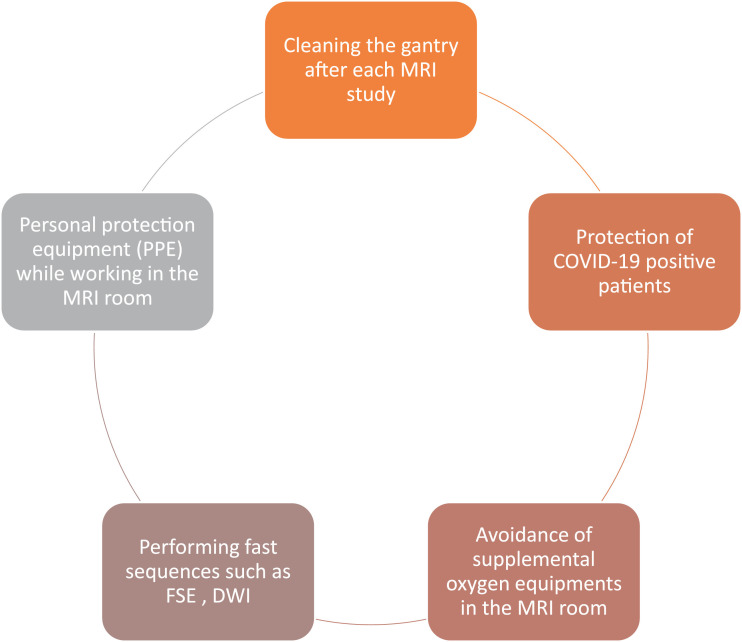
From another aspect, decontamination of imaging devices and suites should be considered. Recently, the ACR published guidance on this issue (6), recommending that while cleaning and disinfection protocols are greatly dependent on the clinical circumstances of each individual setting, 60-minute downtime is generally required accompanied with cleaning of all at-reach surfaces in a particular pattern with approved disinfectant agents (8,9,12). It is important to note that the CT gantry is larger than the MRI gantry and thus, this may increase the possible contamination of the MR machine with COVID-19 patients’ droplets. Whether CT scans or MR machines should be cleaned with different disinfectants has not been investigated yet in the COVID-19 pandemic, but studies have shown that applying 0.1% sodium hypochlorite or 62%–71% ethanol on surfaces is sufficient (10,11). Hence, more information about cleaning MRI/CT scans in the current outbreak should be gathered (Fig 2 ).
Figure 2.
Recommended protective measures in the MRI suite.
Conclusively, neuroimaging should be preserved only for patients at a high risk of developing serious neurologic events. Strict adherence to cleaning protocols is also recommended in radiologic centers to prevent the spread of infection.
Author Contribution
M.S.T, E.K, H.B.M, A.K, and N.K have designed the article and N.K, M.S.T, T.F and S.H. have written the article.
Footnotes
Prior Presentations: No.
Disclosures: M.S.T, E.K, H.B.K, N.K, N.K and S.H report no conflict of interest or funding sources.
References
- 1.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mao L., Jin H., Wang M. Neurologic manifestations of hospitalized patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. Published online April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poyiadji N., Shahin G., Noujaim D. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin H., Hong C., Chen S. Consensus for prevention and management of coronavirus disease 2019 (COVID-19) for neurologists. Stroke and Vascular Neurology. 2020 doi: 10.1136/svn-2020-000382. svn-2020-000382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings [2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Access date: [2020/06/05].
- 6.ACR guidance on COVID-19 and MR use [2020]. Available from: https://www.acr.org/Clinical-Resources/Radiology-Safety/MR-Safety/COVID-19-and-MR-Use. Access date: [2020/06/05].
- 7.Murray O.M., Bisset J.M., Gilligan P.J. Respirators and surgical facemasks for COVID-19: implications for MRI. Clin Radiol. 2020 doi: 10.1016/j.crad.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection [2020]. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Access date: [2020/06/05].
- 9.Mossa-Basha M., Medverd J., Linnau K. Policies and guidelines for COVID-19 preparedness: experiences from the University of Washington. Radiology. 2020 doi: 10.1148/radiol.2020201326. [DOI] [PubMed] [Google Scholar]
- 10.Ding J., Fu H., Liu Y. Prevention and control measures in radiology department for COVID-19. Eur Radiol. 2020 doi: 10.1007/s00330-020-06850-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kampf G., Todt D., Pfaender S. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sedaghat A., Gity M., Radpour A. COVID-19 protection guidelines in outpatient medical imaging centers. Acad Radiol. 2020 doi: 10.1016/j.acra.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]