ABSTRACT |
Background:
Occupational diseases involving the immune system are considered to be occupational allergic diseases (OAD); 15% of occupational diseases are allergic. The social consequences of OAD are significant for both workers and employers.
Objectives:
To describe demographic and clinical characteristics of patients with OAD and their social outcomes.
Methods:
Descriptive and retrospective study of the medical records of patients diagnosed with OAD cared at the occupational allergy clinic of a university hospital in São Paulo, Brazil.
Results:
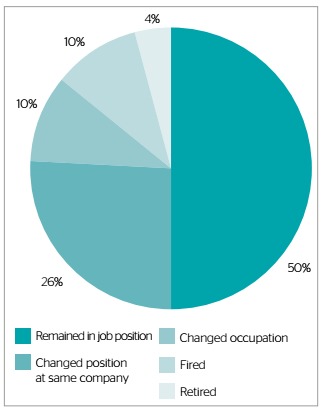
A total of 72 patients exhibited OAD, with age 21 to 89 years old; 52% were male. Atopic antecedents were described for 35% of patients. Most patients worked in the chemical industry (17%), cleaning (15%), construction (11%) and health care (8%). Occupational rhinitis was found in 26% of the patients, work-related asthma in 18%, asthma and rhinitis in 25%, and allergic contact dermatitis in 13%. In regard to the social outcomes, 36 (50%) workers remained in their jobs, 19 (26%) changed function, 7 (10%) changed occupation, 7 (10%) were fired and 3 (4%) retired.
Conclusions:
In the present study, OAD prevailed among males and within the economically active age; cases of occupational rhinitis were the most frequent. Half of the employees remained in the same job position even after diagnosis.
Keywords |: allergy and immunology; asthma, occupational; rhinitis, allergic; dermatitis, occupational
RESUMO |
Introdução:
Doença ocupacional envolvendo o sistema imunológico é considerada doença alérgica ocupacional (DAO). Das doenças ocupacionais, 15% são alérgicas. As consequências sociais do diagnóstico de DAO são importantes para o trabalhador e empregador.
Objetivos:
Descrever características demográficas e clínicas dos pacientes estudados com DAO e seus desfechos sociais.
Métodos:
Estudo descritivo, retrospectivo dos prontuários de pacientes do ambulatório de alergia ocupacional de hospital universitário em São Paulo, com diagnóstico de DAO.
Resultados:
72 pacientes apresentaram DAO, com idades entre 21 e 89 anos; 52% do sexo masculino. Antecedentes atópicos foram descritos em 35% dos pacientes. A maioria dos pacientes trabalhava nas áreas de indústria química (17%), limpeza (15%), construção civil (11%) e saúde (8%). Rinite ocupacional foi vista em 26% dos pacientes; asma relacionada ao trabalho, em 18%; asma e rinite, em 25%; dermatite de contato alérgica, em 13%. Sobre o desfecho social, 36 (50%) mantiveram-se em seus cargos, 19 (26%) mudaram de função, 7 (10%) mudaram de área, 7 (10%) foram afastados e 3 (4%) se aposentaram.
Conclusões:
Na casuística estudada, a DAO prevaleceu no sexo masculino, em faixa etária condizente com faixa trabalhadora; com maior número de casos de rinite ocupacional. Metade dos pacientes continuou exercendo a mesma função mesmo após o diagnóstico.
INTRODUCTION
Our modern society underwent fast changes; the resulting conquests have had effects on human life, both individually and collectively1. As a function of new lifestyles, adults spend more time at the workplace, where they are exposed to a diversity of potentially irritating and immunogenic substances likely to cause disease2. Within this scenario, occupational diseases are increasingly receiving more attention in discussions on workers’ health. Occupational diseases are the ones acquired or developed as a function of particular circumstances related with the work performed3. When the underlying pathogenic mechanism is immunogenic (a hypersensitivity reaction) these conditions are denominated allergic occupational diseases (AOD). From the clinical point of view, exposed workers might develop respiratory or skin occupational allergies2, including: work-related asthma, which might be accompanied by allergic rhinitis and conjunctivitis (originated in the same immune mechanism that causes occupational asthma), contact dermatitis and anaphylaxis, in some cases4.
Among the risks factors predisposing to and promoting occupational allergies, length of exposure to allergens is the most relevant5. Atopy is described as a non-environmental risk factor that contributes to the onset of occupational allergies, as well as to previous development of occupational conjunctivitis and rhinitis alone6.
According to estimates, 15% of occupational diseases have allergic manifestations7. The data on incidence are variable; in the United States the mean incidence is 3/1million cases and in Canada 50/1million cases8. As to Brazil, the incidence of diagnosed cases of occupational asthma in the city of São Paulo was 17/million registered individuals, however, this is possibly an underestimation of the actual rate9. More specifically, occupational asthma represents 5 to 10% of all adult cases of asthma, which denotes its relevance as a public health problem10. The average age at diagnosis is 43 years old; 75% of cases correspond to men4. In regard to occupational skin disorders, they affect about 1% of workers in developed countries. The frequency in Brazil is similar compared to other countries11. The peak age for onset of disease is 30 years old, and is also more frequent among men12.
The social consequences of a confirmed diagnosis of AOD affect both employee and employer. In Brazil, OAD are relevant for their political and social aspects, for which reason four ministries are involved in their control: Labor, Justice, Health and Social Security13. Anydiagnosed case of AOD must be notified through a Work Accident Report (WAR) issued by the Ministry of Social Security and Welfare. WAR are mandatory and must be produced when workers are referred for a medical legal examination at the National Institute of Social Insurance (Instituto Nacional do Seguro Social - INSS). The goal of such examinations is to investigate the causal relationship of disease and presence of disability, which are the criteria that ground the decision on whether to grant or not social security benefits14. We should observe that in the case of occupational diseases, WAR can be only issued for workers with formal employment relationship. Onlyworkers on leave for more than 15 days must perform a medical legal examination at INSS.
Although occupational allergies represent a relevant part of occupational diseases, few Brazilian studies addressed the epidemiology of patients and the social outcomes with which they must cope. Therefore, the aim of the present study was to describe demographic and clinical characteristics of patients with AOD cared at a university hospital in São Paulo and the impact of these conditions on the life of the analyzed population.
METHODS
The present retrospective descriptive study was conducted with 72 patients cared from 2002 to 2015 at the occupational allergy outpatient clinic of the department of allergy and immunology of a university hospital in the city of São Paulo. The analyzed data were extracted from the patients’ electronic medical records (PRONTMED) and included age, sex, occupation, history of atopy, type of AOD, time since onset of symptoms, repercussion of disease, treatments and clinical progression. Data analysis was performed with software Micrsoft® Office Excel (2012). The results were subjected to simple statistical analysis and clustered according to the study goals.
RESULTS
Among 503 patients seen in the period from 2002 to 2015, the ones with AOD (work-related asthma, occupational rhinitis or allergic contact dermatitis) confirmed by clinical or laboratory methods were included in the study. Seventy-two (27%) patients exhibited some occupational allergy and were included in the study. The sample age varied from 21 to 89 years old, mean 51.6 years old. Thirty-eight (52%) patients were male and 34 (48%) female. History of atopy was reported by 26 (35%) patients.
The jobs with the highest prevalence of AOD were the ones related to the chemical industry (17%), cleaning (15%), civil construction (11%), health care (8%) and involving use of paint at some point (7%).
Follow up varied from a maximum of 156months to a minimum of 2months.
Nineteen (26%) patients were diagnosed with occupational rhinitis; the most common symptoms were nasal discharge (49%) and itch (42%) (Figure 1). Within this group, 70% of the patients exhibited clinical improvement following use of the prescribed medications, the main ones being fluticasone nasal spray and budesonide nasal spray. Combined systemic treatment (oral loratadine) was performed by 40% of the sample.
Figure 1. Frequency of respiratory symptoms among patients with occupational asthma and rhinitis (patients might had exhibited more than one symptom), São Paulo, 2002-2015 (N=72).

Occupational asthma was detected in 13 (18%) cases; the most common symptoms were dyspnea on exertion (60%) and dry cough (43%) (Figure 1). The most frequent medication for maintenance treatment was inhaled budesonide + formoterol, and inhaled salbutamol for asthma attacks. Eighteen (25%) patients exhibited asthma and rhinitis concomitantly.
Occupational skin disorders were diagnosed for 9 patients (13%), the main causes being latex for health care workers (33%) and chemicals for civil construction workers and individuals using cleaning products. Also association were found between dermatitis and asthma (8%), dermatitis and rhinitis (8%) and dermatitis, asthma and rhinitis (1%) (Figure 2). Topical treatment was performed by 6 (66%) patients. Use of betamethasone cream was associated with clinical improvement in 50% of the cases; hydrocortisone ointment induced improvement in 75% of the patients.
Figure 2. Distribution of patients per occupational allergy diagnosis, São Paulo, 2002-2015 (N=72).

Relative to the social outcomes, 36 (50%) patients remained in the same job position, 19 (26%) changed position within the same company, 7 (10%) had to change their occupation, 7 (10%) were fired and 3 (4%) retired by disability as a function of the severity of asthma and were granted social security benefits (Figure 3).
Figure 3. Socio-occupational situation of patients diagnosed with occupational allergy, São Paulo, 2002-2015 (N=72).
DISCUSSION
AOD have been scarcely investigated in Brazil although they represent a considerable public health and social security problem. However, advances were made in recent years through identification of new agents, development of diagnostic methods and advancement of the knowledge on the pathophysiology and natural history of disease.
A total of 503 patients with suspected AOD were provided care at the occupational allergy outpatient clinic of the department of allergy and immunology of a university hospital in the city of São Paulo in the period from 2002 to 2015, but diagnosis was confirmed only for 27% of the cases. On data analysis we found that the non-return to work rate was high, which fact often hindered the establishment of a definitive diagnosis. This finding evidences the need for greater awareness among workers and employers about follow up for occupational allergies, and the risks and long-term consequences of disease. The sample age varied from 21 to 89 years, mean 51.6 years old. This variable exhibits wide variation in the literature as a function of the analyzed dependent factors, such as onset of work, predisposition to allergies and occupational activity as such. Nevertheless, the age range found in the present study corresponds to the one of period of more intense professional activity among the overall population15. AOD prevailed among males (52%), which disagrees from the results of some studies, in which women predominated. This discrepancy might be attributed to differences between the samples of the various studies2,15,16.
History of atopy was reported by 35% of the patients, which reinforces the strong relationship between atopy and odds for occupational events, within which context also activity type and length of exposure are relevant5. On analysis of the association between occupation and AOD, disease was found to prevail among chemical industry (17.0%), cleaning (17.0%), civil construction (11%) and health care (8%) workers, as well as among the ones that use paint at some point (7%). These findings agree with the fields with higher prevalence of occupational allergies, such as the chemical industry, carpentry and joinery, health care (assistants and nurses), agriculture, cleaning and caregiving. Thenumber of patients with work-related disorders is higher for these fields due to the composition of the products used daily, such animal antigens in agriculture and livestock, formaldehydes, acrylates, adhesives, lubricants, solvents, dust and fumes17.
As to diagnosis, occupational rhinitis was the most prevalent (26%) and 25% of the cases exhibited association of asthma and rhinitis. These results agree with the findings in Vandenplas etal.’s (2010) study18, in which 90% of the patients exhibited associated diseases. The study by Castano etal. (2009)19 reported similar rates, with 76% of correlation. In the present study, 18% of the patients were diagnosed with occupational asthma, which disagrees from other studies which found prevalence rates of 26 to 52% for occupational asthma relative to all occupational diseases2. A possible explanation is that many workers with suspected work-related asthma seek care at pneumology, rather than at allergy and immunology services.
Relative to occupational skin disorders, only 13% of the patients exhibited allergic contact dermatitis, which also disagrees from the results of other studies, which pointed to prevalence rates of up to 60% relative to all occupational diseases. We should observe that the vast majority of occupational skin disorders corresponds to cases of irritant contact dermatitis, while in the present study we only considered allergic contact dermatitis. We believe that the reason might be that occupations differ according to geographical region (nurses, fishermen, carpenters, agriculturists, etc.), being that different jobs might exhibit more or less relationship with dermatitis20.
Finally, the most interesting finding concerns the social outcomes of patients. About 50% remained in their older job position, which is a cause of concern considering the chronic nature of occupational allergies, which is not taken into account by patients, who often believe the problem will be solved with medication alone, without any need for occupational reeducation. Workers are also afraid of reporting occurrences to employers, case they come to lose their jobs. It is thus a part of the physicians’ duty togive orientation and implement the measures neededto improve both disease and working conditions through proper filling of WAR.
It is worth observing that term work-related asthma comprises work-aggravated and occupational asthma, and the same is the case of rhinitis, which might be work aggravated or occupational. Following diagnosis, the measures for work-aggravated and occupational asthma are the same, to wit, permanent removal from exposure, treatment of disease and reporting by means of WAR. Inother words, from the practical perspective we stress that the cases of previous, work-aggravated asthma should not be underestimated, as the measures for it are the same as for occupational stress. We further emphasize that once an occupational allergic disorder is diagnosed, patients should be referred to occupational physicians, and also to pneumologists for additional orientation and follow up as per need.
CONCLUSION
Based on the data collected in the present study, we might conclude that the prevalence of AOD at the investigated service was higher among males and individuals of economically active age and that most cases were of occupational rhinitis.
AOD is still underdiagnosed in Brazil and deserves attention from health care services to enable prevention and more thorough knowledge of its epidemiology.
Study conducted at Clinical Hospital, School of Medicine, University of São Paulo - São Paulo (SP), Brazil.
Funding: none
REFERENCES
- 1.Araújo TM, Graça CC, Araújo E. Estresse ocupacional e saúde: contribuições do modelo demanda-controle. Ciênc Saúde Coletiva. 2003;8(4):991–1003. [Google Scholar]
- 2.Galvão CES. Asma e rinite ocupacionais: visão imuno-alérgicas. Rev Bras Alerg Imunopatol. 2010;33(1):2–7. [Google Scholar]
- 3.Murofuse NT, Abranches SS, Napoleão AA. Reflexões sobre estresse e Burnout e a relação com a enfermagem. Rev Latino-Am. Enferm. 2005 Apr;13(2):255–261. doi: 10.1590/s0104-11692005000200019. [DOI] [PubMed] [Google Scholar]
- 4.Royal College of Physicians . Allergy: The Unmet Need. A Blueprint for Better Patient Care. A Report of the Royal College of Physicians Working Party on the Provision of Allergy Services in the UK. 2003. [Google Scholar]
- 5.Peden D, Reed CE. Environmental and occupational allergies. JAllergy Clin Immunol. 2010;125(2) 2:S150–S160. doi: 10.1016/j.jaci.2009.10.073. [DOI] [PubMed] [Google Scholar]
- 6.Dykewicz MS. Occupational asthma: current concepts in pathogenesis, diagnosis, and management. J Allergy Clin Immunol. 2009;123:519–528. doi: 10.1016/j.jaci.2009.01.061. [DOI] [PubMed] [Google Scholar]
- 7.Jeebhay MF. Occupational allergy and asthma among food processing workers in South Africa. Afr Newslett Occup Health Safety. 2002;12:59–62. [Google Scholar]
- 8.Carvalho PK, Barbosa D, Vieira PC. Doenças relacionadas ao trabalho: asma ocupacional. Rev. Eletr Acervo Saúde. 2012;4:229–246. [Google Scholar]
- 9.Mendonça EMC, Algranti E, Silva RCC, Buschinelli JTP. Ambulatório de pneumopatias ocupacionais da Fundacentro: resultados após 10 anos. Rev Bras Saúde Ocup. 1994;22:7–13. [Google Scholar]
- 10.Kogevinas M, Anto JM, Sunyer J, Tobias A, Kromhout H, Burney P. Occupational asthma in Europe and other industrialised areas: apopulation-based study. European Community Respiratory Health Survey Study Group. Lancet. 1999;353(9166):1750–1754. doi: 10.1016/s0140-6736(98)07397-8. [DOI] [PubMed] [Google Scholar]
- 11.Ali AS. Dermatoses ocupacionais. São Paulo: Fundacentro/Fundunesp; 2001. [Google Scholar]
- 12.Alchorne AOA, Alchorne MMA, Silva MM. Dermatoses ocupacionais. An Bras. Dermatol. 2010 Apr;85(2):137–147. doi: 10.1590/s0365-05962010000200003. [DOI] [PubMed] [Google Scholar]
- 13.Duarte I, Rotter A, Lazzarini R. Frequência da dermatite de contato ocupacional em ambulatório de alergia dermatológica. An Bras Dermatol. 2010 Aug;85(4):455–459. doi: 10.1590/s0365-05962010000400006. [DOI] [PubMed] [Google Scholar]
- 14.Sociedade Brasileira de Pneumologia e Tisiologia I Consenso Brasileiro sobre Espirometria. J Pneumol. 1996;22(3):105–164. [Google Scholar]
- 15.Meding B. Differences between sexes with regard to work-related skin disease. Contact Dermatitis. 2000;43:65–71. doi: 10.1034/j.1600-0536.2000.043002065.x. [DOI] [PubMed] [Google Scholar]
- 16.Belsito DV. Occupational contact dermatitis: etiology, prevalence, and resultant impairment/disability. J Am Acad Dermatol. 2005;53:303–313. doi: 10.1016/j.jaad.2005.02.045. [DOI] [PubMed] [Google Scholar]
- 17.Lillienberg L, Andersson E, Janson C, Dahlman-höglund A, Forsberg B, Holm M, et al. Occupational exposure and new-onset asthma in a population-based study in Northern Europe (RHINE) Ann Occup Hyg. 2013;57:482–492. doi: 10.1093/annhyg/mes083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vandenplas O, Van Brussel P, D’Alpaos V, Wattiez M, Jamart J, Thimpont J. Rhinitis in subjects with work-exacerbated asthma. Respir Med. 2010;104:497–503. doi: 10.1016/j.rmed.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Castano R, Gautrin D, Thériault G, Trudeau C, Ghezzo H, Malo JL. Occupational rhinitis in workers investigated for occupational asthma. Thorax. 2009;64:50–54. doi: 10.1136/thx.2008.102822. [DOI] [PubMed] [Google Scholar]
- 20.Wold L, Chen JK, Lampel HP. Hand dermatitis: an allergist’s nightmare. Curr Allergy Asthma Rep. 2014;14(11):474–474. doi: 10.1007/s11882-014-0474-0. [DOI] [PubMed] [Google Scholar]


