ABSTRACT |
Background:
Health care professionals are at high risk for work accidents; within this context, personal protective equipment (PPE) acts as a barrier and affords protection in any situation of potential exposure to biological materials.
Objective:
To analyze associated factors and determine the frequency of adherence to use of PPE by health care professionals from the state of Maranhão who suffered sharps injuries at work.
Methods:
A cross-sectional epidemiological and analytical study based on secondary data from the System of Information on Notifiable Diseases (Sistema de Informação de Agravos de Notificação - SINAN) was performed with health care professionals who suffered sharps injuries from 2010 to 2015. Unadjusted analysis was performed first and then hierarchical adjusted analysis with adherence to use of PPE as response variable. Only variables with p<0.05 were considered as having association with the response variable.
Results:
The frequency of use of PPE was 41%. At the end of hierarchical analysis, non-adherence to use of PPE remained associated with having 12 or less years of formal schooling, working at the capital/metropolitan area, percutaneous exposure, exposure to blood, needlestick injuries and improper disposal of sharps.
Conclusion:
The frequency of adherence to PPE was relatively low among health care professionals from the state of Maranhão who were victims of accidents. Twelve years or less of formal schooling, not using PPE and improper disposal of sharps might contribute to the occurrence of work accidents at health care services.
Keywords |: accidents, occupational; personal protective equipment; exposure to biological agents
RESUMO |
Contexto:
Os profissionais da área de saúde estão expostos ao risco de acidentes de trabalho; por isso, equipamentos de proteção individual (EPIs) atuam como barreira e promovem proteção sempre que haja possibilidade de exposição ao material biológico.
Objetivo:
Analisar os fatores associados e determinar a frequência de adesão ao uso de EPI por profissionais de saúde que sofreram acidentes ocupacionais com material biológico no Estado do Maranhão.
Métodos:
Realizou-se um estudo epidemiológico, transversal, tipo analítico baseado em dados secundários do Sistema de Informação de Agravos de Notificação (SINAN) entre os profissionais de saúde acidentados com material biológico no período de 2010 a 2015. Primeiramente, foi realizada a análise não ajustada; na segunda fase, foi adotada a análise ajustada do tipo hierarquizada, tendo como variável resposta a adesão ao uso de EPI. Foram consideradas associadas à variável resposta aquelas que apresentaram p<0,05.
Resultados:
A frequência de utilização de EPI foi de 41% e, ao final da análise hierarquizada, mantiveram-se associados a não utilização de EPI: ter 12 anos ou menos de estudo; trabalhar na capital/região metropolitana; sofrer exposição percutânea, por sangue, por agulha e por descarte inadequado de perfurocortantes.
Conclusão:
A frequência de adesão ao uso de EPI foi relativamente baixa entre os profissionais de saúde que sofreram acidentes no Estado do Maranhão. Os profissionais com 12 anos ou menos de estudo, não utilizando EPI e que realizaram descarte inadequado de materiais perfurocortantes podem estar contribuindo para a ocorrência de acidentes ocupacionais nas instituições de saúde.
INTRODUCTION
Work is a social activity and plays a key role in the living conditions of human beings. However, depending on how it is performed, work might expose workers to hazards in the workplace, and thus interfere with their state of health and cause multiple illnesses1.
Biosafety in health care work environments must begin by implementation of standard precautions (SP), among which we might mention hand washing, use of personal protective equipment (PPE), adequate handling of residuals and immunization to protect professionals and patients against exposure to biological fluids2,3,4.
Biosafety at Brazilian health care facilities is the subject of Regulatory Norm no. 32 (RN 32)5. NR 32 recommends implementing preventive measures for each particular hazard to promote the safety of workers in health care services. Among such measures, use of PPE stands out.
RN 6 defines PPE as any device or product individually used by workers to prevent risks that might threaten their safety and health at work6.
While use of PPE does not protect against all thehazards to which workers are exposed, it reducesthe odds of occurrence of accidents. Health care professionals are exposed by handling sharps, and there is also skin and mucosal exposure to contaminated blood and bodily secretions during the performance of work. Such exposures and sharps injuries are considered to be extremely dangerous, because they are potentially able to transmit more than 20 different kinds of pathogens, being the human immunodeficiency virus (HIV) and the hepatitis B (HBV) and C (HCV) viruses the most frequent ones7.
The most important factor within this scenario is adherence to use of PPE, attended by a proactive attitude to comply with measures for prevention of accidents to protect patients, other professionals and oneself. Although several studies evidenced the high severity of accidents involving biological materials and point to use of PPE as the best preventive means, in practice many workers underestimate the risk, which accounts for the low adherence to and improper use or handling of PPE4,8,9.
Some of the factors that contribute to non-adherence to preventive measures include: workers’ resistance to changes in the routine of procedures, lack of protective resources and lack of managers’ support4. Factors that influence the adoption of preventive measures must be identified to make feasible and orient continuing education and training of health care professionals for adherence to SP, and consequently to use of PPE, to occur in all situations, thus ensuring the safety of workers at work4.
Accurate knowledge of the circumstances that determine and influence the occurrence of accidents by exposure to biological materials at health care facilities, non-adherence to preventive measures such as use of PPE, in particular, might provide grounds for the planning of preventive actions.
Therefore, the aims of the present study were to analyze associated factors and investigate the rate of adherence to use of PPE among health care professionals from the state of Maranhão who were victims of work accidents involving biological materials in the period from 2010 to 2015.
METHODS
The present cross-sectional, analytical time-series study investigated accidents involving biological materials suffered by health care professionals from the state of Maranhão in the period from 2010 to 2015. Maranhão is a part of the Brazilian Northeastern macro-region. With a current population of 6.9 million inhabitants, Maranhão occupies an area of 331,936.955 km2; the population density is 20.80 inhabitants/km2. There are 5,118 registered health care facilities, including hospitals and health basic units, among others, and about 50,000 health care providers10,11.
The study population corresponded to all the health care professionals who were victims of work accidents involving biological materials reported in Maranhão from 1 January 2010 to 31 December 2015. As the survey was performed in July 2016, the database was up-to-date, since enough time had elapsed to allow for the inclusion of reports filed in 2015.
The inclusion criterion was: health care professionals who were victims of work accidents involving biological materials at health care services. Work accidents with exposure to biological materials were defined as incidents involving blood or other biological fluids occurring to health care professionals at work12.
Information was collected from the System of Information on Notifiable Diseases (Sistema de Informações sobre Agravosde Notificação - SINAN), State Secretariat of Health of Maranhão, database and exported to software Microsoft® Excel 2010. Next we excluded all the variables identifying the included individuals to protect their anonymity, as well as inconsistencies (imprecise information), incomplete data (missing data) and duplicates (two or more records of one and the same case). We selected variables related to the sociodemographic and occupational profile of the health care professionals who were victims of accidents and to the characteristics of accidents by sharps.
In the fitting of the regression model, use of PPE on the occasion of the accident with exposure to biological materials was considered the dependent variable and was categorized as yes or no.
Adherence to PPE was defined as use of three or more of the pieces of equipment (gloves, mask, glasses, face protection and boots) listed in the SINAN accident investigation form and used as a function of the procedure to be performed and the body part requiring protection13.
The independent variables were clustered in three levels (Figure 1).
Figure 1. Theoretical model of hierarchical analysis for use of personal protective equipment by health care professionals.
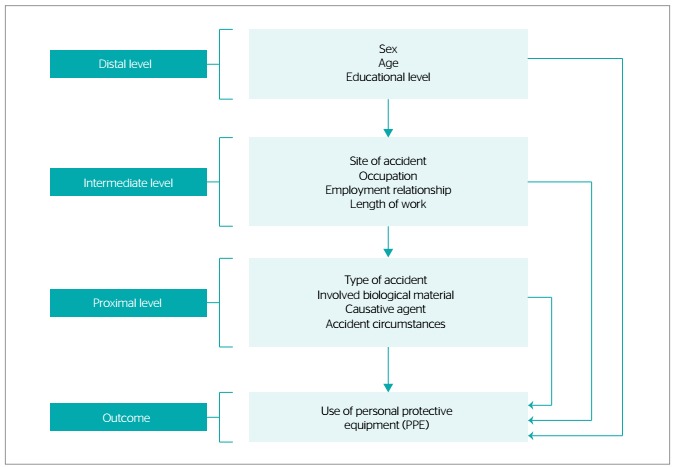
Distal level
Sociodemographic variables:
Age range (in years): 18-30, 31-40, 41-50, 51-60, >60
Sex: male, female
Educational level (years of formal schooling): ≤12, >12
Intermediate level
Occupation: physician, nurse, pharmacist, dentist, physical therapist, nursing technician and laboratory technician, among others
Employment relationship: formal - work on the books, civil servant; informal: cooperative job, work off the books, temporary job, among others
Length of work (in years): <1, 1-5, 6-10, 11-20, >20
Site of accident: capital/metropolitan area; other counties
Proximal level
Accident characteristics: circumstances, type of accident, involved biological material and causative agent
First we performed descriptive analysis of the data through calculation of absolute and relative frequencies to represent the characteristics of the investigated population and adherence to use of PPE.
The response (dependent) variable was adherence to use of PPE; demographic, occupational and accident-related characteristics were considered as explanatory (independent) variables. We began by univariate analysis, in which we tested the association of all the variables with the outcome. To identify the associated factors we fitted a Poisson regression model with robust variance to reduce possible overestimation of the standard error, because the dependent variable was binary and its frequency (or prevalence) was over 10%14. Nextwe calculated prevalence ratios (PR) considering PR=1 as reference category, 95% confidence intervals (95%CI) and p-value. The variables that exhibited p<0.20 were kept for adjusted analysis.
In a second step we performed Poisson regression analysis with robust variance and hierarchical data modeling to calculate the PR between independent variables and outcome15. On hierarchical analysis, variables are clustered in levels as a function of their influence on the outcome. The distal level included the demographic variables, the intermediate level the occupational variables and the proximal level the accident-related variables, as depicted in the flowchart (Figure 1). Association estimates were adjusted for the variables belonging to the same and previous hierarchical levels, which allowed keeping the variables more strongly associated with the outcome of interest16.
Variables were included in the model along three hierarchical steps according to their influence on the outcome. First we included the distal level variables that exhibited p<0.20 on non-adjusted analysis together. Only the variables with significance level 0.05 remained in the adjusted model for this level. Next we included the intermediate level variables that exhibited p<0.20 on non-adjusted analysis. These variables were simultaneously included in the model independently from the statistical significance of the distal level variables already included in the model; the intermediate level variables with significance level 0.05 remained in the model. Finally we included the proximal level variables with p<0.20 together with the variables from the two previous levels that proved to be significant within their respective hierarchical levels. Only the proximate level variables with significance level 0.05 remained in the adjusted model, without removing any of the distal and intermediate level variables independently from their significance level. This resulted in an adjusted analysis model with three hierarchical levels.
In compliance with the National Council of Health (Conselho Nacional de Saúde - CNS) Resolution, no. 466/2012, the study was submitted for appraisal to and was approved by the research ethics committee of University Hospital, Federal University of Maranhão (Hospital Universitário da Universidade Federal do Maranhão - HUUFMA) ruling no. 327,795/2013.
RESULTS
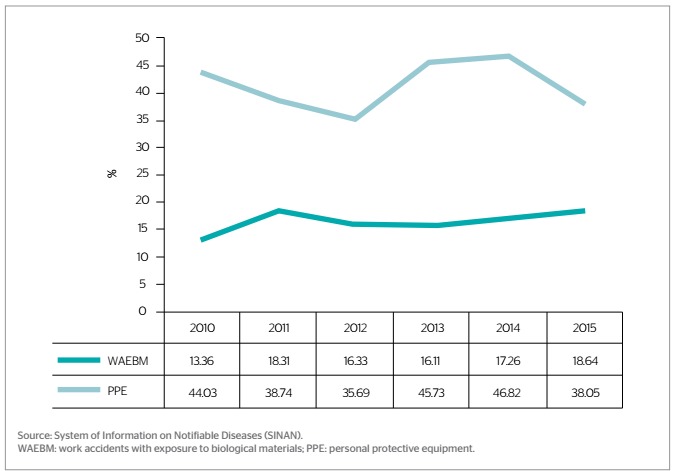
The total number of health care professionals from Maranhão who were victims of work accidents with exposure to biological materials (WAEBM) in the period from January 2010 to December 2015 was 1,819. Thehighest rates corresponded to 2011 (18.31%) and 2015 (18.64%). The estimated frequency of use of PPE by health care professionals was 41.34%; the highest rates corresponded to 2010 (44.03%), 2013 (45.82%) and 2014 (46.82%) (Figure 2).
Figure 2. Percentage of work accidents with exposure to biological materials and prevalence of use of personal protective equipment among health care professionals per year, state of Maranhão, 2010-2015 (n=1,819).
Relative to the sociodemographic and occupational profile of the health care professionals who were victims of accidents we found predominance of:
age range 31 to 40 years old (37%) followed by 18 to 30years old (35.73%);
females (85.05%);
12 years or less of formal schooling (89.72%);
formal employment relationship (82.35%) and 1 to 5years of work (41.51%);
nursing technicians (73.83%).
Accidents were more frequent among the health professionals who worked at the capital/metropolitan area (73.56%). The accidents were most frequently due to improper disposal of sharps (42.44%), occurred via percutaneous exposure (83.40%), involved blood (79.77%) and were caused by needles (66.19%).
The variables associated with non-adherence to use of PPE with statistical significance on non-adjusted analysis (p<0.05) were (Tables 1 and 2):
Table 1. Non-adjusted analysis of distal and intermediate variables relative to non-adherence to use of personal protective equipment among health care professionals who were victims of work accidents with exposure to biological materials in the state of Maranhão, 2010-2015 (n=1,819).
| Variables | Use of PPE | PR | 95%CI | p-value* | |
|---|---|---|---|---|---|
| Yes | No | ||||
| 752 (41.34% | 1.067 (58.66%) | ||||
| Distal variables | |||||
| Sex | |||||
| Female | 633 (84.18) | 914 (85.66) | 0.98 | 0.94-1.02 | 0.388 |
| Male | 119 (15.82) | 153 (14.34) | 1 | - | - |
| Age (years) | |||||
| 18-30 | 289 (38.43) | 361 (33.83) | 0.96 | 0.94-0.99 | 0.046 |
| 31-40 | 263 (34.97) | 410 (38.43) | 1.02 | 0.99-1.05 | 0.131 |
| 41-50 | 143 (19.02) | 215 (20.15) | 1.00 | - | - |
| 51-60 | 48 (6.38) | 71(6.65) | 1.00 | 0.95-1.06 | 0.817 |
| >60 | 9 (1.20) | 10 (0.94) | 0.96 | 0.82-1.11 | 0.604 |
| Formal schooling (years) | |||||
| ≤12 | 438 (58.24) | 716 (67.10) | 1.04 | 1.00-1.09 | 0.043 |
| >12 | 314 (41.76) | 351 (32.90) | 1.00 | - | - |
| Intermediate variables | |||||
| Site of accident | |||||
| Capital/metropolitan area | 581 (77.26) | 757 (70.95) | 1.05 | 1.01-1.08 | 0.002 |
| Other counties | 171 (22.74) | 310 (29.09) | 1.00 | - | - |
| Professional category | |||||
| Physicians | 56 (7.45) | 71 (6.65) | 1.00 | - | - |
| Dentists | 15 (1.19) | 19 (1.78) | 0.98 | 0.88-1.09 | 0.744 |
| Pharmacists | 3(0.40) | 7(0.66) | 0.98 | 0.92-1.03 | 0.520 |
| Nurses | 102 (13.56) | 117 (10.97) | 0.96 | 0.91-1.00 | 0.102 |
| Physical therapists | 18 (2.39) | 15 (1.41) | 0.91 | 0.81-1.02 | 0.141 |
| Nursing technicians | 542 (72.07) | 801 (75.07) | 1.02 | 0.99-1.05 | 0.157 |
| Laboratory technicians | 16 (2.13) | 37 (3.47) | 1.07 | 0.99-1.15 | 0.064 |
| Employment relationship | |||||
| Formal | 620 (82.45) | 878 (82.29) | 1.00 | - | - |
| Informal | 132 (17.55) | 189 (17.71) | 1.00 | 0.98-1.01 | 0.930 |
| Length of work (years) | |||||
| <1 | 231 (30.72) | 308 (28.87) | 0.98 | 0.95-1.01 | 0.397 |
| 1-5 | 295 (39.23) | 460 (43.11) | 1.02 | 0.99-1.05 | 0.096 |
| 6-10 | 105 (13.96) | 154(14.43) | 1.00 | - | - |
| 11-15 | 44 (5.85) | 56 (5.25) | 0.98 | 0.96-1.04 | 0.585 |
| 16-20 | 30 (3.99) | 38 (3.56) | 0.98 | 0.92-1.04 | 0.641 |
| >20 | 47 (6.25) | 51 (4.78) | 0.95 | 0.89-1.02 | 0.186 |
PPE: personal protective equipment; PR: prevalence ratio; 95%CI: 95% confidence interval; *calculated by means of Poisson regression.
Table 2. Non-adjusted analysis of proximal variables relative to non-adherence to use of personal protective equipment among health care professionals who were victims of work accidents with exposure to biological materials in the state of Maranhão, 2010-2015 (n=1,819).
| Variables | Use of PPE | PR | 95%CI | p-value* | |
|---|---|---|---|---|---|
| Yes | No | ||||
| 752 (41.34%) | 1.067 (58.66%) | ||||
| Proximal | |||||
| Type of accident | |||||
| Percutaneous | 597 (79.39) | 920 (86.22) | 1.08 | 1.03-1.12 | <0.001 |
| Mucosal | 123 (16.36) | 129 (12.09) | 1.00 | - | - |
| Percutaneous-mucosal | 32 (4.26) | 18 (1.69) | 0.85 | 0.77-0.94 | 0.002 |
| Involved biological material | |||||
| Blood | 583 (77.53) | 868 (81.35) | 1.03 | 0.99-1.07 | 0.050 |
| Bloody fluid | 36 (4.79) | 43 (4.03) | 0.97 | 0.90-1.04 | 0.446 |
| Plasma | 8(1.06) | 4(0.37) | 1.00 | - | - |
| Other | 58 (7.71) | 57 (5.34) | 0.93 | 0.88-0.99 | 0.050 |
| Not reported | 67 (8.91) | 95 (8.90) | 0.99 | 0.95-1.05 | 0.996 |
| Causative agent | |||||
| Needles | 466 (61.97) | 738 (69.17) | 1.05 | 1.01-1.08 | 0.002 |
| Intracath | 8 (1.06) | 20 (1.87) | 1.08 | 0.98-1.19 | 0.118 |
| Blade/lancet | 52 (6.91) | 79 (7.40) | 1.00 | - | - |
| Glass | 11 (1.46) | 16 (1.50) | 1.00 | 0.89-1.12 | 0.949 |
| Other | 177 (23.54) | 174 (16.31) | 0.92 | 0.89-0.96 | <0.001 |
| Not reported | 38 (5.05) | 40 (3.75) | 1.01 | 0.95-1.06 | 0.688 |
| Accident circumstance | |||||
| Administration of medication | 158 (21.01) | 281 (26.34) | 1.04 | 1.01-1.07 | 0.007 |
| Venous/arterial puncture | 138 (18.35) | 189 (17.71) | 1.00 | - | - |
| Improper disposal of sharps | 333 (44.28) | 439 (41.14) | 0.98 | 0.95-1.00 | 0.184 |
| Surgical procedures | 123 (16.26) | 158 (14.81) | 0.98 | 0.94-1.02 | 0.378 |
PPE: personal protective equipment; PR: prevalence ratio; 95%CI: 95% confidence interval; *calculated by means of Poisson regression.
age range 18 to 30 years old (PR=0.96; p=0.046);
≤12 years of formal schooling (PR=1.04; p=0.043);
working at the capital/metropolitan area (PR=1.05; p=0.002);
percutaneous exposure (PR=1.08; p<0.001);
blood as biological material (PR=1.03; p<0.050);
caused by needles (PR=1.05; p=0.002);
for administration of medication (PR=1.04; p=0.007).
On adjusted analysis, the distal level variables which maintained statistical significance (p<0.05) following adjustment for the other variables in the same level were:
age range 18 to 30 years old (PR=0.96; p=0.040);
≤ 12 years of formal schooling (PR=1.04; p=0.043).
The intermediate level variables were included in the model; following adjustment, ≤12 years of formal schooling (PR=1.04; p=0.038) and working at the capital/metropolitan area (PR=1.04; p=0.011) remained statistically significant.
In the final hierarchical adjusted model, following inclusion of the proximal level variables, the variables that maintained statistically significant association with non-adherence to use of PPE were:
age range 18 to 30 years old (PR=0.96; p=0.040);
≤12 years of formal schooling (PR=1.04; p=0.043);
working at the capital/metropolitan area (PR=1.04; p=0.11);
percutaneous exposure (PR=1.02; p=0.010);
blood as biological material (PR=1.10; p=0.016);
caused by needles (PR=1.10; p=0.003);
improper disposal of sharps (PR=1.05; p=0.04).
It is worth observing that variables ≤12 years of formal schooling, working at the capital/metropolitan area, accident from percutaneous exposure, exposure to blood, caused by needles and/or due to improper disposal ofsharps were associated with not using PPE at the timeof the accident (Table 3).
Table 3. Final model for hierarchical analysis of distal, intermediate and proximal variables relative to non-adherence to use of personal protective equipment among health care professionals who were victims of work accidents with exposure to biological materials in the state of Maranhão, 2010-2015 (n=1,819).
| Variables | PR | 95%CI | p-value* |
|---|---|---|---|
| Age 18 to 30 years old | 0.96 | 0.92-0.99 | 0.040 |
| ≤12 years of formal schooling | 1.04 | 1.00-1.09 | 0.043 |
| Working at the capital/metropolitan area | 1.04 | 1.01-1.07 | 0.011 |
| Percutaneous exposure | 1.02 | 1.00-1.10 | 0.010 |
| Blood as biological material | 1.01 | 1.00-1.05 | 0.016 |
| Caused by needles | 1.01 | 1.01-1.09 | 0.004 |
| Disposal of sharps | 1.05 | 1.01-1.11 | 0.004 |
PR: prevalence ratio; 95%CI: 95% confidence interval; *calculated based on a Poisson regression model with robust variance.
DISCUSSION
In the present study, the frequency of use of PPE was 41.34%, thus lower than the ones reported in studies conducted in China (55.5%)17, United States (62%)18 and the Brazilian states of São Paulo (78.07%)19 and Mato Grosso (79.7%)20, but higher than the one found in a study performed in Minas Gerais (36.6%). This discrepancy might be explained by differences in the methods employed in the various studies, in which investigation of use of PPE was restricted to professional categories or health care facilities, as well as differences in the methods used for data collection and sample size. Among possible explanations for our findings, we might mention the resistance of many health care providers against use of PPE and lack of availability of PPE at health care facilities. Some studies3,21 found that although health professionals do recognize the presence of hazards in their work environment, they often ignore the possibility of contamination and the relevance of protection at work.
Availability of PPE at health care services is the basic condition for employees to use them in their work. RN 6 recommends that the employers provide PPE in sufficient number to professionals who perform high-risk activities, and ensure its immediate supply or replacement7.
The results of the present study showed that for 2011 and 2015, the rates of WAEBM were the highest and the ones of use of PPE the lowest, which suggests that the higher number of WAEBM might be related to low adherence to use of PPE. It is worth reminding that other studies22,23 observed that PPE behaves as a protective barrier, thus it contributes to reduce risks and avoid more serious accidents.
Relative to the health care professionals’ profile, WAEBM were more frequent among the ones aged 31 to 40 years old. Similar results were reported for Ceará24 and São Luís25, in which the largest proportion of victims of WAEBM were 20 to 39 years old.
Some authors26,27,28 emphasized the need for training courses and time enough for adjustment to the activities and routines of health care services. The reason is that many health care professionals enter the labor market without adequate knowledge of the precautions required to avoid exposure to hazards present in the hospital environment and remain without specific training and orientation relative to occupational hazards and the required precautions.
Women were more often involved in WAEBM, which corroborates the findings in other studies3,17,21,27,28 in which the rates of female victims varied from 71.2 to 86.5%. Thissituation might be related to the fact that the number of female employees is considerable larger at health care services, as well as among the health care professions. Moreover, women frequently also perform additional work (household chores and family care) which prolong the daily working hours and cause physical and mental exhaustion, which contribute to the occurrence of accidents in the workplace29.
Differently, we did not find association between sex and non-adherence to use of PPE. Despite the substantial numerical differences between men and women that might reflect on safety and health at work, as health care professionals both sexes exhibited a similar attitude in regard to the risk of exposure to biological materials and to protective measures.
Accidents were more frequent among the professionals who had attended 12 or less years of formal schooling (secondary or elementary school) among which the nursing technicians stood out, this category behaving as the most susceptible. Similar data were found in other studies25,27.
Occurrence of work accidents among the aforementioned workers is possibly related to flaws in their training in regard to occupational hazards and negligence in the use of PPE. Several studies22,24,25,27,30 found that health care professionals with low educational level (nursing technicians and assistants) suffered more often work accidents and exhibited low rates of adherence to use of PPE. It is worth stressing that in the hierarchical analysis performed in the present study, having attended 12 or less years of formal schooling increased 1.04 times the odds of accidents involving sharps.
The largest proportion of WAEBM corresponded to professionals working at the capital/metropolitan area. This finding might be related to the fact that a large number of health care services are located in this geographical area, which thus concentrates a very large number of workers. A similar situation was evidenced in a study performed in Bahia31, where the number of WAEBM was also larger in urban areas, the state capital and metropolitan area in particular, which is the largest supplier of jobs in the state, especially in the health care sector, and hosts a large number of hospitals and outpatient facilities.
Hierarchical analysis evidenced significant association between working at the capital/metropolitan area and non-adherence to use of PPE, increasing 1.04 times the odds of WAEBM. This finding is perhaps related to unavailabilityof PPE and/or resistance to use it and poor investment in training courses at the local health care services.
The main circumstance for occurrence of accidents was improper disposal of sharps. One frequent reason is that disposal containers are filled beyond their capacity, which favors exposure. A similar finding was reported in a study conducted in 50 counties in Minas Gerais20.
In agreement with the literature17,20,21,22,23,24, accidents from percutaneous exposure were the most frequent. The reason might probably be that the skin surface is larger than the mucosal one, and the body surface is in immediate contact with instruments during the performance of procedures23. Blood was the biological material most often involved in the analyzed accidents, which were mainly caused by needles, which were the instruments that most contributed to the accidents involving percutaneous exposure.
Hierarchical analysis evidenced statistically significant association among improper disposal of sharps, percutaneous exposure, blood as biological material, needles as causative agent and non-adherence to use of PPE. This finding suggests that health care professionals who do not adhere to use of PPE are more vulnerable to accidents involving sharps. These data corroborate the results of a study28 which showed that 78% of the analyzed professionals dismissed the biosafety norms, including use of PPE.
However, we should observe that use of PPE does not fully eliminate the risk of accidents involving sharps32. According to RN appendix III Plan for Prevention against Risk of Accidents Involving Sharps (Plano de Prevenção de Riscos de Acidentes com Materiais Perfurocortantes - PPRAMP) also safety devices during handling of sharps are needed to meet this goal. Indeed, use of PPE and safe practices significantly contribute to reduce the risk of work accidents and infection33.
One of the difficulties we met in the present study concerns SINAN database; many data are missing, boxes are left empty, which hinders the attempts at achieving an accurate characterization of the situation of WAEBM and use of PPE. We believe that this flaw is due to the fact that filing reports is a routine activity still ineffectively performed at health care services, the epidemiological surveillance efforts at counties notwithstanding. Theinformation actually available points to the need ofbetter qualification, which might be achieved via trainingof the involved professionals and periodical investigation of possible errors.
Despite its limitations, the present study has some strengths, such as affording a diagnosis of the situation of work accidents and adherence to use of PPE by health care professionals in Maranhão, a description of the profile of such professionals and of the factors associated with non-adherence to use of PPE during performance of work activities.
CONCLUSION
We found a relatively low frequency of adherence to use of PPE (41.39%) among health care professionals in Maranhão who were victims of accidents. Professionals with low educational level (≤12 years of formal schooling), who do not use PPE and dispose of sharps wrongly might be contributing to the occurrence of work accidents in health care services.
As a function of the results and taking the peculiarities of each service into account, we consider that education and specific training of health care professionals as to the relevance and adequate use of PPE, as well as orientation on all other biosafety norms, has paramount importance
Study performed at Federal University of Maranhão (Universidade Federal do Maranhão - UFMA) - São Luís (MA), Brazil.
Funding: none
REFERENCES
- 1.Tibães HB. Análise dos dados referentes aos acidentes de trabalho por exposição a material biológico com contaminação por hepatites virais "B" e "C", em uma capital brasileira [Dissertação de Mestrado] Belo Horizonte: Universidade Federal de Minas Gerais; 2012. Dissertação de Mestrado. [Google Scholar]
- 2.Marziale MH, Valim MD. Notificação de acidentes do trabalho com exposição a material biológico: estudo transversal. OBJN. 2012;11(1):53–67. [Google Scholar]
- 3.Ribeiro LC, Souza AC, Neves HC, Munari DB, Medeiros M, Tripple AF. Influência da exposição a material biológico na adesão ao uso de equipamentos de proteção individual. Cienc Cuid Saude. 2010;9(2):325–332. doi: 10.4025/cienccuidsaude.v9i2.8282. [DOI] [Google Scholar]
- 4.Suarte HA, Teixeira PL, Ribeiro MS. O uso dos equipamentos de proteção individual e a prática da equipe de enfermagem no centro cirúrgico. Rev Cient do ITPAC. 2013;6(2):1–8. [Google Scholar]
- 5.Brasil. Ministério do Trabalho e Emprego . Portaria nº 485, de 11 de novembro de 2005. Aprova a Norma Regulamentadora nº 32. Brasília: Ministério do Trabalho e Emprego; 2005. [Google Scholar]
- 6.Brasil. Ministério do Trabalho e Emprego . Norma Regulamentadora 6 - NR 6: Equipamento de proteção individual - EPI. Brasília: Ministério do Trabalho e Emprego; 2006. [Google Scholar]
- 7.Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas . Exposição a materiais biológicos. Brasília: 2006. [Google Scholar]
- 8.Neves HC, Ribeiro L, Souza AC, Munari DB, Medeiros M. A influência das relações interpessoais na adesão aos equipamentos de proteção individual. Sau & Transf Soc. 2011;1(2):84–93. [Google Scholar]
- 9.Barbosa AS, Diogo GA, Salotti SR, Silva SM. Subnotificação de acidente ocupacional com materiais biológicos entre profissionais de enfermagem em um hospital público. Rev Bras Med Trab. 2017;15(1):12–17. [Google Scholar]
- 10.Cnes Net . Cadastro Nacional de Estabelecimentos de Saúde. Secretaria de Atenção à Saúde. Ministério da Saúde; 2016. internet. Disponível em: http://cnes2.datasus.gov.br/Mod_Ind_Unidade.asp. [Google Scholar]
- 11.Datasus . Cadernos de informações de saúde Maranhão. Ministério da Saúde; 2010. internet. Disponível em http://tabnet.datasus.gov.br/tabdata/cadernos/ma.htm. [Google Scholar]
- 12.Brasil. Ministério do Trabalho e Emprego . Portaria nº 1.748, de 30 de agosto de 2011. Plano de prevenção de riscos de acidentes com materiais perfurocortantes. Brasília: Ministério do Trabalho e Emprego; 2011. [Google Scholar]
- 13.Sarquis LM, Miranda FM, Amaral PM. Felli VE, Baptista PC. Saúde do Trabalhador de Enfermagem. Baueri: Manole; 2015. Biossegurança e exposição a fluidos biológicos; pp. 86–101. [Google Scholar]
- 14.Papaléo CL. Estimação de risco relativo e razão de prevalência com desfecho binário [Dissertação de Mestrado] Porto Alegre: Universidade Federal do Rio Grande do Sul; 2009. Dissertação de Mestrado. [Google Scholar]
- 15.Hirakata VN. Estudos transversais e longitudinais com desfechos binários: qual a melhor medida de efeito a ser utilizada? Ver HCPA. 2009;29(2):174–176. [Google Scholar]
- 16.Fuchs SC, Victora CG, Fachel J. Modelo hierarquizado uma proposta de modelagem aplicada à investigação de fatores de risco para diarreia grave. Rev Saúde Públ. 1996;30(2):168–178. doi: 10.1590/S0034-89101996000200009. [DOI] [PubMed] [Google Scholar]
- 17.Hu X, Zhang Z, Li N, Liu D, Zhang L, He W. Self-reported use of personal protective equipment among Chinese critical care clinicians during 2009 H1N1 influenza pandemic. PLoS One. 2012;7(9):e44723. doi: 10.1371/journal.pone.0044723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daughert EL, Perl TM, Needham DM, Rubinson L, Bilderback A, Rand CS. The use personal protective equipament for control of influenza among critical care clinicians: a survey study. Crit Care Med. 2009;37(4):1210–1216. doi: 10.1097/CCM.0b013e31819d67b5. [DOI] [PubMed] [Google Scholar]
- 19.Schiesari A, Júnior, Lepre AA, Scucuglia AC, Gomes NL, Fernandes VA. Epidemiologia dos acidentes com material biológico em um centro de referência do noroeste paulista. Cuid Arte Enferm. 2014;8(2):115–121. [Google Scholar]
- 20.Souza AC, Brune MW, Brune MF. A avaliação das notificações de acidentes com exposição a material biológico na região do Médio Araguaia/MT. Infarma. 2014;26(1):67–72. [Google Scholar]
- 21.Ferreira DM. Morbi-mortalidade e agravos relacionados ao trabalho em Pernambuco de 2007 a 2010 [Dissertação de Mestrado] Recife: Fundação Oswaldo Cruz; 2012. Dissertação de Mestrado. [Google Scholar]
- 22.Ferreira RC, Martins AM, Mota DL, Pereira RD, Santos NC, Queiroz IO. Uso de equipamentos de proteção individual entre cirurgiões-dentistas de Montes Claros, Brasil. Arquivos em Odontologia. 2010;46(2):88–97. [Google Scholar]
- 23.Rondon EC, Tavares MS, Santos WL. Fatores dificultadores e facilitadores que os profissionais de enfermagem enfrentam relacionados ao uso dos EPI's. Rev Gestão & Saúde. 2012;3(3):1045–1060. [Google Scholar]
- 24.Pereira EM, Torres AR. Incidência de acidentes de trabalho com exposição a material biológico no Ceará, 2009 a 2012. Rev Formar Interdisciplinar. 2015;1(7):42–55. [Google Scholar]
- 25.Gonçalves PM, Belfort IK, Fernandes MA, Monteiro SC, Sousa WR, Sampaio RM. Análise da estatística de acidentes com exposição de material biológico no Maranhão nos anos 2009-2010. Rev Pesq Saúde. 2014;15(3):360–363. [Google Scholar]
- 26.Magagnini MA, Miotto LB, Serradilha AF. Acidentes de trabalho com material biológico entre os profissionais de saúde. Cuid Arte Enferm. 2008;2(1):53–60. [Google Scholar]
- 27.Análise dos acidentes de trabalho com fluidos biológicos entre trabalhadores brasileiros de 2007 a 2014 [Tese de Doutorado] Curitiba: Universidade Federal do Paraná; 2016. Tese de Doutorado. [Google Scholar]
- 28.Santos SS, Costa NA, Mascarenhas MD. Caracterização das exposições ocupacionais a material biológico entre trabalhadores de hospitais no Município de Teresina, Estado do Piauí, Brasil, 2007 a 2011. Epidemiol Serv Saúde. 2013;22(1):165–170. [Google Scholar]
- 29.Julio RS, Filardi MB, Marziale MH. Acidentes de trabalho com material biológico ocorridos em munícipios de Minas Gerais. Rev Bras Enferm. 2014;67(1):119–126. doi: 10.5935/0034-7167.20140016. [DOI] [PubMed] [Google Scholar]
- 30.Santos EP, Junior, Batista RR, Almeida AT, Abreu RA. Acidente de trabalho com material perfurocortante envolvendo profissionais e estudantes da área da saúde em hospital de referência. Rev Bras Med Trab. 2015;13(2):69–75. [Google Scholar]
- 31.Cordeiro TM, Carneiro JN, Neto, Cardoso MC, Mattos AI, Santos KO, Araújo TM. Acidentes de trabalho com exposição a material biológico: descrição dos casos na Bahia. R Epidemiol Control Infec. 2016;6(2):50–56. [Google Scholar]
- 32.Garcia LP, Blank VL, Blank N. Aderência a medidas de proteção individual contra a hepatite B entre cirurgiões-dentistas e auxiliares de consultório dentário. Rev Bras Epidemiol. 2007;10(4):525–536. [Google Scholar]
- 33.Talhaferro B, Barboza DB, Oliveira AR. Adesão ao uso dos equipamentos de proteção individual pela enfermagem. Rev Ciênc Méd. 2008;17(3-6):157–166. [Google Scholar]


