Introduction
Cutaneous vasculitis may occur as a primary idiopathic process, a secondary phenomenon associated with systemic disease, or an eruption triggered by drug intake, vaccination or infection.1, 2, 3, 4, 5 The spectrum of implicated infectious agents includes viruses, bacteria, fungi, protozoa, and helminths. Septic vasculitis is a mixed vessel (small and medium vessel) variant of cutaneous vasculitis associated with severe bacterial infections or sepsis. Here, we report an unusual case of septic vasculitis caused by Providencia stuartii that occurred in Providence, Rhode Island.
Case report
A 56-year-old woman with a history of pulmonary embolism and stage IV breast cancer presented to the emergency department at Rhode Island Hospital with ecchymoses on her upper and lower extremities. Relevant home medications included warfarin and oral dexamethasone for brain metastases. Although she was not receiving chemotherapy, a port-o-cath was in place. Laboratory evaluation found pancytopenia (hemoglobin of 7.6 g/dL, white blood cell count of 0.9 × 109/L, and platelets of 34 × 109/L) and an elevated international normalized ratio of 2.3. After urine and blood cultures were drawn, she was started on empirical piperacillin/tazobactam. Warfarin was discontinued, and her coagulopathy was corrected with fresh frozen plasma, packed red blood cells, platelets, and vitamin K.
Despite these interventions, her ecchymoses progressed to bullae on her second hospital day, and dermatology input was requested. Skin examination revealed 10- to 30-cm purpuric plaques with a livedo pattern and hemorrhagic bullae with central necrosis on her arms and legs (Fig 1). The bullae were mildly painful to touch. Extensive purpura were asymmetrically distributed on her arms, and few petechiae were scattered along her chest and back. At the time of examination, she was hemodynamically stable and afebrile. Two punch biopsies of the right thigh were performed and specimens were sent for culture and routine hematoxylin-eosin staining.
Fig 1.

A, Hemorrhagic bullae with surrounding purpura. B, Hemorrhagic bullae with surrounding purpura on the medial left leg.
Histopathologic examination demonstrated the presence of ischemic epidermal necrosis and fibrin thrombi occluding capillaries in the dermis and subcutis. Focal vasculitis with perivascular neutrophils and dermal hemorrhage was also observed (Fig 2, A). Gram stain found rare intra- and extravascular gram-negative rods (Fig 2, B). Tissue culture grew 1+ gram-negative rods. Urine culture was negative. The blood culture was speciated to P stuartii, and the diagnosis of P stuartii septic vasculitis was rendered. The infectious disease department was consulted, and cefepime was recommended as treatment. Repeat cultures continued to grow P stuartii, so the patient was switched to ciprofloxacin and caspofungin for broad fungal coverage. She continued to improve throughout her hospital stay and was discharged to a skilled nursing facility after 11 days to complete 2 weeks of intravenous antibiotic therapy.
Fig 2.
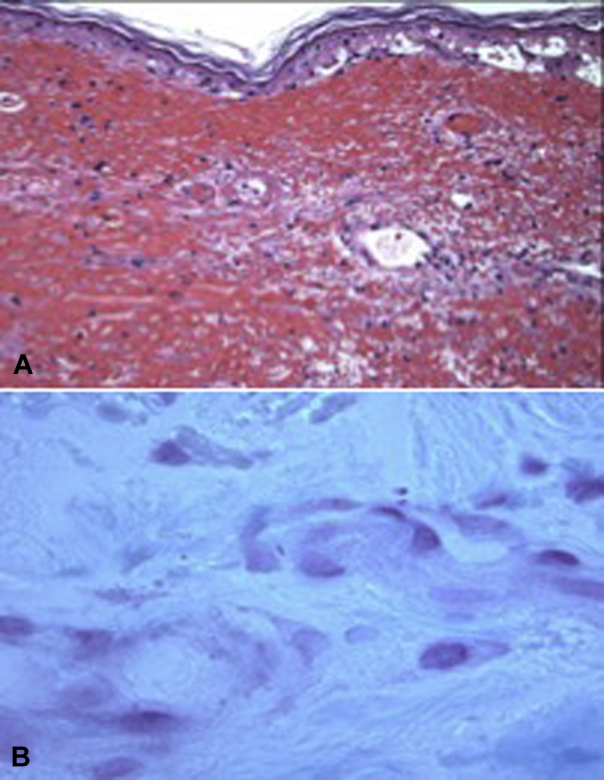
A, Ischemic epidermal necrosis and fibrin thrombi occluding capillaries in the superficial dermis and focal perivascular fibrin deposition with scant neutrophils, pericytoplastic debris, and dermal hemorrhage. B, Extravascular gram-negative rods. (A, Hematoxylin-eosin stain, B, Gram stain; original magnifications: A, ×100; B, ×1000.)
Discussion
Clinically, septic vasculitis presents as hemorrhagic lesions, palpable or pustular purpura, vesicles, and bullae on acral skin and pressure sites.6 Histologically, septic vasculitis is a subtype of neutrophilic vasculitis that is characterized by occlusive intraluminal fibrin thrombi composed of neutrophils, red blood cells, platelets, and fibrin. Bacteria may or may not be present in thrombi, as damage to blood vessels may occur through direct invasion of microorganisms into vessel walls or by immune-mediated mechanisms.1,7
Organisms of the genus Providencia were first described by Stuart et al8 in 1943 at Brown University in Providence, Rhode Island where this patient presented. Providencia stuartii is a gram-negative rod, often associated with bacteriuria and urinary tract infections in nursing home residents with indwelling catheters.9 Rarely, the organism has been reported to cause bacteremia and septicemia. The propensity of Providencia stuartii to infect the urine of catheterized patients may be explained by a hemagglutinin molecule, mannose-resistant/Klebsiella-like (MR/K), found in certain strains.10 Isolates expressing MR/K are more likely to bind to catheter material once introduced and cause longer episodes of bacteriuria than strains that do not express this hemagglutinin.
Long-term urinary catherization, urologic stent placement, age, and paraplegia are well-documented risk factors for Providencia infections. Thus, the emergence of P stuartii septicemia in an immunosuppressed patient without any risk factors is uncommon. Her port-o-cath may have served as a route for infection and supported growth of the MR/K-expressing strain. Although malignancies and autoimmune diseases may manifest as cutaneous vasculitis, the associated lesions tend to be symmetrically distributed. The asymmetric nature of this patient's lesions raised the possibility of an infectious etiology. Although this patient was bacteremic, she did not present with clinical signs of sepsis such as fever, tachycardia, or hypotension. Daily steroid use may have blunted her immune response to infection leaving cutaneous lesions as the presenting symptom of septicemia.
To our knowledge, there are no previously reported cases of P stuartii septic vasculitis. This case shows that, in rare cases, cutaneous manifestations of vasculitis such as purpura, pustular dermatoses, and hemorrhagic lesions may be the first signs of sepsis. Therefore, if infection is suspected, lesions should be biopsied for histologic examination and tissue culture as soon as possible.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
Appendix
PubMed, MEDLINE, EMBASE Academic Search Premier, CINAHL databases were individually searched from inception to October 2019 with the following search terms: “providencia vasculitis,” “providencia septic vasculitis,” and “providencia stuartii septic vasculitis.” Full texts were searches of retrieved articles. In addition, the Brown University search engine was used, which simultaneously searches more than 100 databases and more than 15,000,000 books. We did not find any evidence of previous reports of P stuartii septic vasculitis; thus, we have included the claim that this is the first case reported in the literature.
References
- 1.Carlson J.A., Ng B.T., Chen K.R. Cutaneous vasculitis update: diagnostic criteria, classification, epidemiology, etiology, pathogenesis, evaluation and prognosis. Am J Dermatopathol. 2005;27(6):504–528. doi: 10.1097/01.dad.0000181109.54532.c5. [DOI] [PubMed] [Google Scholar]
- 2.Caproni M., Verdelli A. An update on the nomenclature for cutaneous vasculitis. Curr Opin Rheumatol. 2019;31(1):46–52. doi: 10.1097/BOR.0000000000000563. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Porrua C., Gonzalez-Gay M.A. Bacterial infection presenting as cutaneous vasculitis in adults. Clin Exp Rheumatol. 1999;17(4):471–473. [PubMed] [Google Scholar]
- 4.Blanco R., Martinez-Taboada V.M., Rodriguez-Valverde V., Garcia-Fuentes M. Cutaneous vasculitis in children and adults. Associated diseases and etiologic factors in 303 patients. Medicine. 1998;77(6):403–418. doi: 10.1097/00005792-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Sunderkotter C.H., Zelger B., Chen K.R. Nomenclature of cutaneous vasculitis: dermatologic addendum to the 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheumatol. 2018;70(2):171–184. doi: 10.1002/art.40375. [DOI] [PubMed] [Google Scholar]
- 6.Carlson J.A., Chen K.R. Cutaneous vasculitis update: small vessel neutrophilic vasculitis syndromes. Am J Dermatopathol. 2006;28(6):486–506. doi: 10.1097/01.dad.0000246646.45651.a2. [DOI] [PubMed] [Google Scholar]
- 7.Barnhill R.L., Crowson A.N., Magro C.M., Piepkorn M.W. 3rd ed. McGraw-Hill Education; 2010. Dermatopathology. [Google Scholar]
- 8.Stuart C.A., Wheeler K.M., Rustigian R., Zimmerman A. Biochemical and antigenic relationships of the paracolon bacteria. J Bacteriol. 1943;45(2):101–119. doi: 10.1128/jb.45.2.101-119.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Warren J.W. Providencia stuartii: a common cause of antibiotic-resistant bacteriuria in patients with long-term indwelling catheters. Rev Infect Dis. 1986;8(1):61–67. doi: 10.1093/clinids/8.1.61. [DOI] [PubMed] [Google Scholar]
- 10.Mobley H.L., Chippendale G.R., Tenney J.H. MR/K hemagglutination of Providencia stuartii correlates with adherence to catheters and with persistence in catheter-associated bacteriuria. J Infect Dis. 1988;157(2):264–271. doi: 10.1093/infdis/157.2.264. [DOI] [PubMed] [Google Scholar]


