Abstract
Objective
To compare perioperative outcomes between cortical bone trajectory (CBT) instrumentation with pedicle screws (PS) in patients undergoing laminectomy and posterolateral fusion for single-level lumbar spinal stenosis, and degenerative grade I spondylolisthesis.
Methods
A consecutive series of 91 patients from a single institution between January 2017 and July 2019 were retrospectively reviewed.
Results
Patients in CBT group had significantly shorter operative time, lower blood loss and shorter length of stay.
Conclusion
CBT instrumentation demonstrated favorable perioperative outcomes that may enhance the overall value in patients undergoing laminectomy and posterolateral fusion for single-level lumbar spinal stenosis, and degenerative grade I spondylolisthesis.
Keywords: Spinal stenosis, Spondylolisthesis, Length of stay, Surgical blood loss, Operative time
Abbreviations
- CBT
Cortical bone trajectory
- PS
Pedicle Screws
- BMI
Body mass index
- ASA
American Society of Anesthesiologists
- EBL
Estimated blood loss
- LOS
Length of stay
1. Introduction
Cortical Bone Trajectory (CBT) instrumentation has been reported as a less invasive, biomechanically equivalent alternative to traditional pedicle screw fixation.1, 2, 3 With the utilization of a medial to lateral screw trajectory, the exposure required for screw placement is similar to a traditional midline laminectomy and less disruptive to the paraspinal soft tissues when compared to the exposure for traditional pedicle screw placement. CBT technique maximizes the thread contact within higher density bone while providing greater screw purchase and interface strength.2 As such, CBT has also been described as a rescue option in cases of pedicle screw failure, loosening, or in patients with poor bone density.4(see Fig. 1, Fig. 2)
Fig. 1.
Anatomy and exposure of the lumbar paraspinal muscles on an axial T2-weighted MRI. Exposure for direct visualization of the CBT starting points and laminectomy (thick dotted line) disrupts only the multifidus (M) and rotatores spinae (not labeled) muscles. Exposure for traditional pedicle screws (thin dotted line) includes the transverse processes and disrupts the longissimus (L) and iliocostalis (IC) muscles.
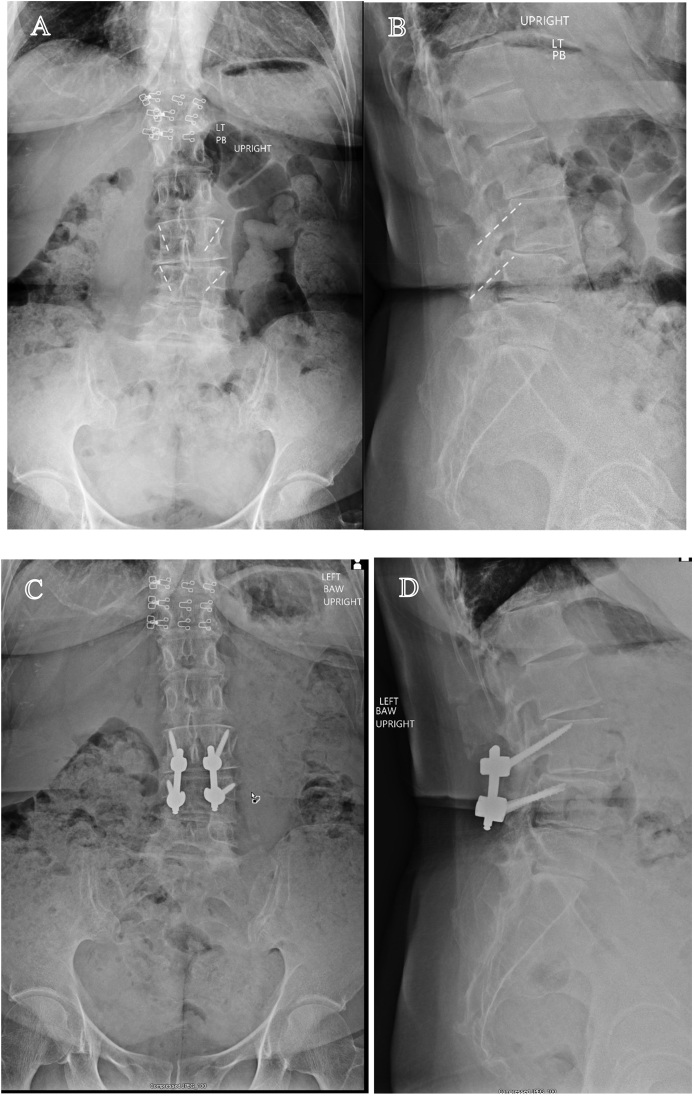
Fig. 2.
Pre-operative and post-operative radiographs demonstrating CBT instrumentation. Standing AP (A) and lateral (B) pre-operative radiographs demonstrating L3/4 grade I spondylolisthesis and approximate trajectory of CBT instrumentation. Standing AP (C) and lateral (D) post-operative radiographs.
Lumbar decompressive laminectomy and instrumented fusion with pedicle screw fixation has become the gold standard surgical treatment for spinal stenosis with associated spondylolisthesis or other causes of relative spinal instability.5,6 Spinal fusion is typically considered to address motion segment stability as well as pervasive symptoms of low back pain when present along with neurogenic claudication or radicular leg pain secondary to spinal stenosis.7 However, the expansion of techniques, including the application of interbody fusion, has led to increased surgical complexity and variability in both clinical and financial outcomes.8,9
CBT instrumentation has been well described in the setting of less invasive midline posterior interbody fusion with favorable outcomes.10 We have observed similar clinical success with CBT instrumentation and interbody fusion. In addition, we have used CBT instrumentation without interbody fusion in obese patients or patients with known osteoporosis undergoing laminectomy and posterolateral fusion for a variety of degenerative conditions. Based on our initial experience, we hypothesize that CBT instrumentation can serve as a less invasive alternative to traditional pedicle screws (PS) with favorable perioperative outcomes in patients with single level spinal stenosis and low-grade spondylolisthesis.
2. Materials and methods
We performed a retrospective review (Level–III evidence) of 91 consecutive patients who underwent decompressive laminectomy and instrumented posterolateral fusion for symptomatic single-level lumbar spinal stenosis with associated grade I degenerative spondylolisthesis from January 2017 through July 2019 in a single institution by one of two fellowship trained spine surgeons. Patients with previous instrumentation, multi-level disease, a mechanism of trauma, or a diagnosis of neoplasm were excluded. Patients were grouped according to the instrumentation used (CBT vs PS). This study was deemed institutional review board exempt by our hospital's Clinical Research Committee.
Patients in the CBT and PS groups were matched according to age, sex, BMI, and ASA class. Perioperative outcome measures included operative time, estimated blood loss (EBL), length of stay (LOS), 30-day readmissions, reoperation for any reason, implant related complications, and total hospital cost. All statistical analysis was performed using SPSS version 24 (IBM, Armonk, NY). Independent samples t-test was used for continuous variables and the Fisher exact test or chi square analysis was conducted to compare nominal variables. A 2-sided P-value < 0.05 was considered statistically significant.
2.1. Surgical technique
All patients underwent an open procedure consisting of a midline decompressive laminectomy and posterolateral fusion. Computer assisted spinal navigation (Medtronic O-Arm and StealthStation) as well as neuromonitoring were used during surgery for both groups. In the PS group, screws were placed with a traditional open exposure of the transverse process and direct visualization of the starting point. In the CBT group, the exposure was limited to the lateral aspect of the facet joints. The CBT starting point was determined using navigation, and a high speed drill and bone tap was used to prepare the screw path. Prior to screw insertion, a midline decompressive laminectomy was performed, with caution to preserve the CBT starting points. Following the decompression, CBT instrumentation was then inserted using computer navigation. In both groups, the corresponding facet joints were then decorticated and a combination of local bone and allograft bone was densely packed into the facet joints and posterolateral soft tissue envelope. Patients were recovered with a standard multimodal pain control regimen (without the use of patient controlled analgesia) and Physical Therapist led mobility protocol (including day of surgery ambulation).
3. Results
A total of 91 patients (41 in the CBT group and 50 in the PS group) were included in the study. All patients had a diagnosis of single-level spinal stenosis and grade I degenerative spondylolisthesis. The average follow up was 220 days (CBT: 190 days vs. PS: 245 days, p = 0.127). Demographic characteristics including age, sex, BMI were similar between the two groups (Table 1). There was a trend towards higher BMI, higher Medicare Hierarchical Condition Categories score (a measure of comorbidity burden), and greater proportion of ASA score 3 in the CBT group but these were not significant.
Table 1.
Patient characteristics. Patient data is provided for laminectomy and posterolateral fusion for single level lumbar stenosis and degenerative spondylolisthesis. PS – Pedicle screw; CBT – Cortical bone trajectory; BMI – Body mass index; HCC - Hierarchical Condition Category; ASA – American Society of Anesthesiologists; SD – Standard deviation.
| Patient Characteristics | CBT Instrumentation | PS Instrumentation | P-value |
|---|---|---|---|
| N | 41 | 50 | – |
| Males (%) | 19 (46.3%) | 14 (28.0%) | 0.070 |
| Age (mean ± SD) | 67.12 ± 10.04 | 66.34 ± 10.11 | 0.714 |
| BMI (mean ± SD) | 32.28 ± 6.21 | 30.34 ± 6.21 | 0.141 |
| HCC (mean ± SD) | 0.74 ± 0.55 | 0.65 ± 0.41 | 0.402 |
| ASA 1 (%) | 0 (0%) | 0 (0%) | – |
| ASA 2 (%) | 19 (46.3%) | 28 (56.0%) | 0.359 |
| ASA 3 (%) | 20 (48.78%) | 21 (42%) | 0.380 |
| ASA 4 (%) | 1 (2.44%) | 1 (2%) | 0.887 |
| Follow up (mean ± SD) | 190.32 ± 114.98 | 244.76 ± 200.77 | 0.127 |
Patients in the CBT group had significantly shorter operative times (160 min vs. 184 min, p = 0.005), lower EBL (201 mL vs. 331 mL, p = 0.002), and shorter LOS (44 h vs. 59 h p = 0.006) (Table 2). There was a trend towards lower total cost in the CBT group ($18,881 vs. $20,060, p = 0.171) although this was not statistically significant. Readmissions were similar between groups, with 1 patient in the CBT group and 1 patient in the PS requiring readmission within 30 days of surgery (2.4% vs. 2.0%, p = 0.897). One patient in the CBT group underwent reoperation for wound dehiscence, and 1 patient in the PS group underwent reoperation for implant loosening. There were no other implant related complications over the study time period.
Table 2.
Perioperative outcomes. Patient data is provided for laminectomy and posterolateral fusion for single level lumbar stenosis and degenerative spondylolisthesis. PS – Pedicle screw; CBT – Cortical bone trajectory; SD – Standard deviation; EBL – Estimated blood loss; LOS – Length of stay; OR – Operating room. † denotes statistical significance with p < 0.05.
| Perioperative Outcome | CBT Instrumentation | PS Instrumentation | P-value |
|---|---|---|---|
| Operative time (mean ± SD) | 160.23 ± 39.41 | 184.02 ± 37.34 | 0.005† |
| EBL (mean ± SD) | 201.79 ± 142.59 | 331.12 ± 219.70 | 0.002† |
| LOS (mean ± SD) | 44.62 ± 17.89 | 59.97 ± 30.93 | 0.006† |
| Total cost (mean ± SD) | $18,881 ± 3640.92 | $20,060.41 ± 4332.13 | 0.171 |
| Readmissions (%) | 1 (2.4%) | 1 (2.0%) | .887 |
| Return to OR (%) | 1 (2.4%) | 1 (2.0%) | .887 |
4. Discussion
In our initial experience, CBT instrumentation appears to be an alternative to pedicle screw fixation in patients with single level lumbar stenosis and spondylolisthesis. Compared to pedicle screw fixation, the CBT cohort had lower blood loss, shorter operative times and shorter LOS. While CBT fixation has been reported in the setting of posterior interbody fusion techniques, our series is among the first to report potential advantages and improved perioperative outcomes compared to traditional pedicle screws for posterolateral fusion alone.10, 11, 12
Crawford et al.13 recently described prognostic factors for achieving optimal outcomes or the minimal symptom state following lumbar fusion for single level spondylolisthesis and concluded that shorter operative times were predictive of greater clinical success. In contrast, negative prognostic factors include comorbidity burden, osteoporosis, high blood loss, and obesity.13, 14, 15, 16, 17 Increased costs of care, particularly when considering prolonged LOS and complication rates, have been reported in these higher risk groups including obese, elderly, and osteoporotic patients.8,14,16,18, 19, 20, 21, 22, 23 With less blood loss, shorter operative time, and ease of placement in obese patients from decreased exposure relative to pedicle screw fixation, CBT instrumentation may be a favorable alternative in achieving best clinical outcomes in select patients.
In our study, there were no implant related complications or need for revision instrumentation over the early postoperative period. Biomechanical studies have demonstrated the efficacy of CBT fixation in osteoporotic bone.24 In a recent prospective study of 22 patients with CBT instrumentation, screw placement was assessed using postoperative CT imaging and the authors demonstrated that increased efficiency and decreased overall complications in the late vs. early cohorts.3 In our series, all screws were placed using computer navigation which may allow for optimal screw placement in regards to position and time of path preparation and insertion. Further, our series included 12 patients with osteoporosis or osteopenia. 25% of these patients received CBT screws, supporting the utility of the approach in these patients in clinical practice.
Interlaminar stabilization (IS) has also been described as a less-invasive alternative to traditional PS fixation in patients with lumbar spinal stenosis and spondylolisthesis.25 Compared to pedicle screw fixation and posterolateral fusion, IS has demonstrated similar benefits as seen in our series including shorter procedure times, lower blood loss, and shorter hospital length of stay — most likely explained by the limited surgical exposure needed for a midline laminectomy and insertion of the interspinous implant. However, in a 3 year follow up study, 16 of 215 (7.4%) patients in the interlaminar stabilization group underwent reoperation including removal of the implant and/or conversion to an instrumented lumbar fusion.26 Similar to interlaminar stabilization, CBT instrumentation appears to offer the benefits of a limited surgical exposure yet provide definitive, rigid fixation and possibly an overall lower likelihood of revision surgery.
CBT instrumentation may also be relevant in transitioning lumbar fusion procedures from the inpatient setting to the outpatient, ambulatory environment. Chin et al.27 compared patients undergoing lumbar fusion in an ambulatory surgery center (ASC) using CBT instrumentation with patients in the hospital using traditional pedicle screws, showing not only favorable outcomes in the CBT group but also demonstrating feasibility of the procedure in an ASC and same-day discharge to home. In our own series, one patient in the CBT group was discharged to home the same day as the procedure. As evidenced by the 15 h reduction in LOS in comparison to pedicle screws, CBT instrumentation may help reduce costs associated with inpatient stays in the high cost hospital setting by expanding the number patients who may undergo posterolateral fusion in the ambulatory setting.
This retrospective case series has several limitations. As a single institution study by two surgeons, the results may not be generalizable to other practicing surgeons, and our several-year experience with computer navigation allowed for easy adoption of this technique. Further, we examined only the early postoperative outcomes of surgery; longer term assessment of radiographic and patient reported outcomes are needed. A prospective study comparing CBT and PS instrumentation, with and without interbody fusion, is needed to determine the relative value of these techniques in the treatment of lumbar stenosis and spondylolisthesis.
5. Conclusion
Few studies have directly compared CBT and PS instrumentation. Our initial series suggests that CBT instrumentation may be a valuable alternative to traditional PS instrumentation for patients undergoing single-level lumbar decompression and posterolateral fusion for lumbar stenosis and spondylolisthesis. CBT instrumentation demonstrates favorable early postoperative outcomes including reduced length of stay, blood loss and operative time which may enhance the overall value of care for select patients. Further prospective study is needed to compare patient-reported and radiographic outcomes.
Funding
No corporate entity or foundation provided any funding for this investigation.
Institutional review board
Study was deemed exempt by the institutional Clinical Research Committee.
Author agreement
All authors have seen and approved the final version of the manuscript being submitted. We warrant that the article is the authors' original work, hasn't received prior publication and isn't under consideration for publication elsewhere.
Declaration of competing interest
None of the authors listed above certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgments
No corporate entity or foundation provided any funding for this investigation. None of the authors have any relevant conflict of interest to disclose.
Contributor Information
Nandakumar Menon, Email: nmenon@aahs.org.
Justin Turcotte, Email: jturcotte@aahs.org.
Alessandro Speciale, Email: aspeciale@aahs.org.
Chad M. Patton, Email: cpatton@aahs.org.
References
- 1.Perez-Orribo L., Kalb S., Reyes P.M., Chang S.W., Crawford N.R. Biomechanics of lumbar cortical screw-rod fixation versus pedicle screw-rod fixation with and without interbody support. Spine. 2013;38(8):635–641. doi: 10.1097/BRS.0b013e318279a95e. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 2.Santoni B.G., Hynes R.A., McGilvray K.C. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9(5):366–373. doi: 10.1016/j.spinee.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Dayani F., Chen Y.R., Johnson E. Minimally invasive lumbar pedicle screw fixation using cortical bone trajectory – screw accuracy, complications, and learning curve in 100 screw placements. J Clin Neurosci. 2019;61:106–111. doi: 10.1016/j.jocn.2018.10.131. [DOI] [PubMed] [Google Scholar]
- 4.Calvert G.C., Lawrence B.D., Abtahi A.M., Bachus K.N., Brodke D.S. Cortical screws used to rescue failed lumbar pedicle screw construct: a biomechanical analysis. J Neurosurg Spine. 2014;22(2):166–172. doi: 10.3171/2014.10.spine14371. [DOI] [PubMed] [Google Scholar]
- 5.Resnick D.K., Watters W.C., Sharan A. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: lumbar fusion for stenosis with spondylolisthesis. J Neurosurg Spine. 2014;21(1):54–61. doi: 10.3171/2014.4.SPINE14274. [DOI] [PubMed] [Google Scholar]
- 6.Talia A.J., Wong M.L., Lau H.C., Kaye A.H. Comparison of the different surgical approaches for lumbar interbody fusion. J Clin Neurosci. 2015;22(2):243–251. doi: 10.1016/j.jocn.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Weinstein J.N., Lurie J.D., Tosteson T.D. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Jt Surg - Ser A. 2009;91(6):1295–1304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raad M., Donaldson C.J., El Dafrawy M.H. Trends in isolated lumbar spinal stenosis surgery among working US adults aged 40–64 years, 2010–2014. J Neurosurg Spine. 2018;29(2):169–175. doi: 10.3171/2018.1.SPINE17964. [DOI] [PubMed] [Google Scholar]
- 9.Makanji H., Schoenfeld A.J., Bhalla A., Bono C.M. Critical analysis of trends in lumbar fusion for degenerative disorders revisited: influence of technique on fusion rate and clinical outcomes. Eur Spine J. 2018;27(8):1868–1876. doi: 10.1007/s00586-018-5544-x. [DOI] [PubMed] [Google Scholar]
- 10.Crawford C.H., Owens R.K., Djurasovic M., Gum J.L., Dimar J.R., Carreon L.Y. Minimally-Invasive midline posterior interbody fusion with cortical bone trajectory screws compares favorably to traditional open transforaminal interbody fusion. Heliyon. 2019;5(9) doi: 10.1016/j.heliyon.2019.e02423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Y.Z., Hai Y., Zhang X.N. Comparison of cortical bone trajectory screw fixation and pedicle screw fixation in posterior lumbar fusion. Zhonghua Yixue Zazhi. 2019;99(19):1473–1478. doi: 10.3760/cma.j.issn.0376-2491.2019.19.008. [DOI] [PubMed] [Google Scholar]
- 12.Delgado-Fernandez J., García-Pallero M.Á., Blasco G., Pulido-Rivas P., Rafael, Sola G. Review of cortical bone trajectory: evidence of a new technique. Asian Spine J. 2017;11(5):817–831. doi: 10.4184/asj.2017.11.5.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crawford C.H., Glassman S.D., Djurasovic M., Owens R.K., Gum J.L., Carreon L.Y. Prognostic factors associated with best outcomes (minimal symptom state) following fusion for lumbar degenerative conditions. Spine J. 2019;19(2):187–190. doi: 10.1016/j.spinee.2018.06.348. [DOI] [PubMed] [Google Scholar]
- 14.Bjerke B.T., Zarrabian M., Aleem I.S. Incidence of osteoporosis-related complications following posterior lumbar fusion. Global Spine J. 2018;8(6):563–569. doi: 10.1177/2192568217743727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lim S., Edelstein A.I., Patel A.A., Kim B.D., Kim J.Y.S. Risk factors for postoperative infections after single-level lumbar fusion surgery. Spine. 2018;43(3):215–222. doi: 10.1097/BRS.0000000000000608. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 16.Marquez-Lara A., Nandyala S.V., Sankaranarayanan S., Noureldin M., Singh K. Body mass index as a predictor of complications and mortality after lumbar spine surgery. Spine. 2014;39(10):798–804. doi: 10.1097/BRS.0000000000000232. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 17.Samuel A.M., Fu M.C., Anandasivam N.S. After posterior fusions for adult spinal deformity, operative time is more predictive of perioperative morbidity, rather than surgical invasiveness. Spine. 2017;42(24):1880–1887. doi: 10.1097/BRS.0000000000002243. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 18.Raad M., Reidler J.S., El Dafrawy M.H. US regional variations in rates, outcomes, and costs of spinal arthrodesis for lumbar spinal stenosis in working adults aged 40–65 years. J Neurosurg Spine. 2018;30(1):83–90. doi: 10.3171/2018.5.spine18184. [DOI] [PubMed] [Google Scholar]
- 19.Deyo R.A., Mirza S.K., Martin B.I., Kreuter W., Goodman D.C., Jarvik J.G. Trends, major Medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA, J Am Med Assoc. 2010;303(13):1259–1265. doi: 10.1001/jama.2011.1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frymoyer J.W. United States trends in lumbar fusion surgery for degenerative conditions: point of view. Spine. 2005;30(12):1446–1447. doi: 10.1097/01.brs.0000166507.28530.13. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 21.Puvanesarajah V., Werner B.C., Cancienne J.M. Morbid obesity and lumbar fusion in patients older than 65 years. Spine. 2017;42(2):122–127. doi: 10.1097/brs.0000000000001692. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 22.Epstein N. Spine surgery in geriatric patients: sometimes unnecessary, too much, or too little. Surg Neurol Int. 2012 doi: 10.4103/2152-7806.91408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yadla S., Malone J., Campbell P.G. Obesity and spine surgery: reassessment based on a prospective evaluation of perioperative complications in elective degenerative thoracolumbar procedures. Spine J. 2010;10(7):581–587. doi: 10.1016/j.spinee.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Sansur C.A., Caffes N.M., Ibrahimi D.M. Biomechanical fixation properties of cortical versus transpedicular screws in the osteoporotic lumbar spine: an in vitro human cadaveric model. J Neurosurg Spine. 2016;25(4):467–476. doi: 10.3171/2016.2.SPINE151046. [DOI] [PubMed] [Google Scholar]
- 25.Davis R.J., Errico T.J., Bae H., Auerbach J.D. Decompression and coflex interlaminar stabilization compared with decompression and instrumented spinal fusion for spinal stenosis and low-grade degenerative spondylolisthesis: two-year results from the prospective, randomized, multicenter, food and drug. Spine. 2013;38(18):1529–1539. doi: 10.1097/BRS.0b013e31829a6d0a. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 26.Bae H.W., Davis R.J., Lauryssen C., Leary S., Maislin G., Musacchio M.J. Three-year follow-up of the prospective, randomized, controlled trial of coflex interlaminar stabilization vs instrumented fusion in patients with lumbar stenosis. Neurosurgery. 2016;79(2):169–180. doi: 10.1227/NEU.0000000000001237. [DOI] [PubMed] [Google Scholar]
- 27.Chin K.R., Pencle F.J.R., Coombs A.V. Clinical outcomes with midline cortical bone trajectory pedicle screws versus traditional pedicle screws in moving lumbar fusions from hospitals to outpatient surgery centers. Clin Spine Surg. 2017;30(6):E791–E797. doi: 10.1097/BSD.0000000000000436. [DOI] [PubMed] [Google Scholar]