Introduction
Cutaneous T-cell lymphoma is a primary non-Hodgkin lymphoma of T lymphocytes and is subclassified by immunophenotype and clinical behavior.1 The majority of cutaneous T-cell lymphoma variants show a T-helper CD4+ phenotype and are characterized on the mycosis fungoides/Sézary syndrome spectrum. Patients with mycosis fungoides manifest skin lesions of patches, plaques, tumors, or all 3, whereas Sézary syndrome has historically been defined as the combination of erythroderma, lymphadenopathy, and leukemic involvement. Several CD8+ cutaneous T-cell lymphoma variants have also been described. Mycosis fungoides palmaris et plantaris was first described in 1995 by Resnik et al2 as mycosis fungoides limited to the palms and soles, and McNiff et al3 reported a case with a CD8+ phenotype. Despite previously reported variants of lymphomatous primary cutaneous involvement with neoplastic CD8+CD4− T lymphocytes, blood involvement with a CD8+CD4− immunophenotype remains a rare entity. Herein, we report a case of CD8+ mycosis fungoides palmaris et plantaris with peripheral blood involvement.
Case report
A 66-year-old man presented with a history of long-standing relapsing-remitting palmar skin lesions. On a background of pink-red discoloration on the bilateral palms were noted numerous deep vesicles, with secondary desquamative scale and fissuring (Fig 1). There was no history of constitutional symptoms. The patient had no chronic medical conditions and was not receiving any medications. Histologic examination of a biopsy showed spongiosis with a superficial lymphohistiocytic inflammatory infiltrate with eosinophils. Epicutaneous patch testing result for potential allergens was negative.
Fig 1.
Mycosis fungoides palmaris et plantaris with peripheral blood involvement. Clinical images of hands, ankle, and soles (A) before diagnosis and treatment, and (B) 5 months after treatment with extracorporeal photophoresis, bexarotene, and spot electron-beam therapy to the palms.
The patient received a preliminary diagnosis of dyshidrotic eczema with severe hand involvement. During the following years, despite trials of various medications the patient developed similar changes on the soles and new violaceous papules on the ankles. He continued to have periodic flares of skin disease without any clear trigger. He documented evolution of his skin disease with serial imaging (Supplemental Video 1). During several years, he was treated with ultrapotent topical steroids, prednisone, cyclosporine, azathioprine, acitretin, excimer laser, home narrow-band ultraviolet B, methotrexate, adalimumab, dupilumab, ustekinumab, and divalproex sodium. He developed prednisone-exacerbated prediabetes and early osteopenia, prompting trials of first tofacitinib and then apremilast and ixekizumab. Flow cytometry result of peripheral blood conducted at years 3 to 5 of presentation was negative.
Seven years after initial presentation, biopsies were performed again of lesions on the hands and ankle. Dermatopathology now revealed features concerning for cutaneous T-cell lymphoma (Fig 2), including aberrant T-cell phenotype (CD8+CD5−CD7−TCR⍺β−TCRɣδ−). Despite CD8+, absence of cytotoxic granules and pattern of CD45RO+CD45RA− militated against an aggressive epidermotropic lymphoma and supported the possibility of mycosis fungoides–type cutaneous T-cell lymphoma. The absence of staining of TCRɣδ (clone H-41, SC-100289) and CD56 also militated against a γ δ lymphoma. Flow cytometry of peripheral blood identified approximately 12% of circulating cells (52.9% of the lymphocyte gate) as an abnormal T-cell population of phenotype CD8+CD3−CD5varCD7dimCD25−CD26varCD2+CD10−CD30−CD57−. Fluorescence in situ hybridization4 results of peripheral blood mononuclear cells indicated normal copy number for ATM, TP53, RB1, CDKN2A, MYC, ARID1A, ZEB1, STAT3, and DNMT3A, suggesting that single-nucleotide mutations were likely driving this patient's clonal expansion. High-throughput sequencing of the TCRβ gene rearrangements of unsorted peripheral blood leukocytes and samples from the palms and soles revealed precise clonal matches in blood to both skin sites, at greater than 10% of all TCRβ sequences identified in each. Positron emission tomography–computed tomography imaging did not reveal changes of lymph node or visceral involvement. Subsequent treatment with extracorporeal photophoresis, oral bexarotene, and spot electron-beam therapy to the palms resulted in marked clinical response (Fig 1). Collectively, these findings define the rare diagnosis of CD8+ mycosis fungoides palmaris et plantaris with peripheral blood involvement.
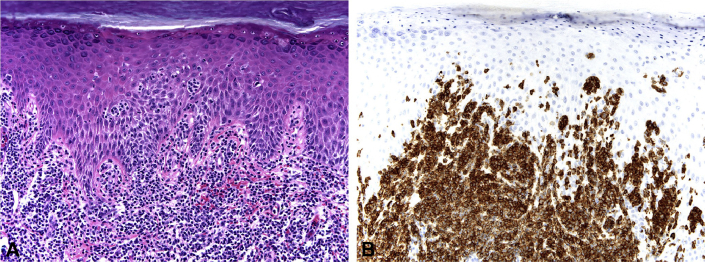
Fig 2.
Mycosis fungoides palmaris et plantaris with peripheral blood involvement. A, Dense lymphocytic infiltrate in the dermis, and single and nested atypical lymphocytes within the epidermis. B, Positive staining result in the majority of lymphocytes. (A, Hematoxylin-eosin stain; original magnification: ×200. B, CD8 immunohistochemical stain; original magnification: ×200.)
Discussion
Cutaneous T-cell lymphoma is group of non-Hodgkin lymphomas characterized by malignant T cells in the skin, with variable involvement of the blood, lymph nodes, and, rarely, viscera. The malignant cells most commonly have a CD3+CD4+CD8−CD45RO+ memory T-cell phenotype.1 For the much rarer cases of CD8+ cutaneous T-cell lymphoma, the World Health Organization defines 4 subclassifications: primary cutaneous CD8+ epidermotropic cytotoxic T-cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma, cutaneous CD8+ lymphomas associated with congenital or acquired immunodeficiency, and CD8+ variants of other well-defined cutaneous T-cell lymphomas, including mycosis fungoides.1 Our patient represents a case of CD8+ mycosis fungoides palmaris et plantaris. The majority of previously reported cases of primary cutaneous CD8+ cytotoxic T-cell lymphomas show metastatic involvement of distal anatomic sites and poor prognosis; however, blood involvement is uncommon.5 Introcaso et al6 described a case of primary cutaneous, aggressive, CD8+CD26−CD7−, epidermotropic, cytotoxic T-cell lymphoma with peripheral blood and central nervous system involvement. Kelemen et al7 identified 2 cases of CD8+ mycosis fungoides with identical clone in the skin and the blood. Herein, we describe a rare case of CD8+ mycosis fungoides palmaris et plantaris with peripheral blood involvement.
Our patient presented with palmoplantar skin disease recalcitrant to numerous therapies, with skin biopsy histology, immunohistochemistry, and molecular analyses eventually indicating the presence of an epidermotropic clonal CD8+CD4− T cell population in the palms and soles. The lack of cytotoxic markers, epidermal necrosis, and negative staining result for TCRɣδ and CD56 did not support a diagnosis of aggressive, primary cutaneous, CD8+, epidermotropic, cytotoxic T-cell lymphoma or γ δ T-cell lymphoma. Consideration was also made for primary cutaneous acral CD8+ T-cell lymphoma. However, this entity is distinguished from our case in that it presents as a slow-growing nodule with CD8+ malignant cells in the dermis and subcutis, with a grenz zone separation from the epidermis.8 We arrived at a diagnosis of mycosis fungoides palmaris et plantaris after trials of multiple therapies, including tumor necrosis factor-α inhibition. Previous reported cases of cutaneous T-cell lymphoma have revealed unmasking or progression after anti–tumor necrosis factor therapy,9 and such may have contributed to pathoetiology in our patient. Foo et al10 reported a variety of cases in which patients receiving treatment for inflammatory dermatoses subsequently received a diagnosis of cutaneous T-cell lymphoma. These cases, as well as the case presented herein, suggest that a chronic inflammatory dermatosis may provide an environment or chronic antigenic stimulus that facilitates T-cell transformation in the skin.10 These data, along with our case, highlight the importance of high clinical suspicion for cutaneous T-cell lymphoma in patients with chronic unremitting inflammatory dermatoses recalcitrant to treatment.
Footnotes
Funding sources: None.
Conflicts of interest: None reported.
Supplementary data
References
- 1.Willemze R., Cerroni L., Kempf W. The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas. Blood. 2019;133:1703–1714. doi: 10.1182/blood-2018-11-881268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Resnik K.S., Kantor G.R., Lessin S.R. Mycosis fungoides palmaris et plantaris. Arch Dermatol. 1995;131(9):1052–1056. [PubMed] [Google Scholar]
- 3.McNiff J.M., Schechner J.S., Crotty P.L., Glusac E.J. Mycosis fungoides palmaris et plantaris or acral pagetoid reticulosis? Am J Dermatopathol. 1998;20(3):271–275. doi: 10.1097/00000372-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Weed J., Gibson J., Lewis J. FISH panel for leukemic CTCL. J Invest Dermatol. 2017;137(3):751–753. doi: 10.1016/j.jid.2016.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guitart J., Martinez-Escala M.E., Subtil A. Primary cutaneous aggressive epidermotropic cytotoxic T-cell lymphomas: reappraisal of a provisional entity in the 2016 WHO classification of cutaneous lymphomas. Mod Pathol. 2017;30(5):761–772. doi: 10.1038/modpathol.2016.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Introcaso C.E., Kim E.J., Gardner J., Junkins-Hopkins J.M., Vittorio C.C., Rook A.H. CD8+ epidermotropic cytotoxic T-cell lymphoma with peripheral blood and central nervous system involvement. Arch Dermatol. 2008;144:1027–1029. doi: 10.1001/archderm.144.8.1027. [DOI] [PubMed] [Google Scholar]
- 7.Kelemen K., White C.R., Gatter K., Braziel R.M., Fan G. Immunophenotypic correlation between skin biopsy and peripheral blood findings in mycosis fungoides. Am J Clin Pathol. 2010;134(5):739–748. doi: 10.1309/AJCP7LRRLK8SLUGE. [DOI] [PubMed] [Google Scholar]
- 8.Hathuc V.M., Hristov A.C., Smith L.B. Primary cutaneous acral CD8+ T-cell lymphoma. Arch Pathol Lab Med. 2017;141(11):1469–1475. doi: 10.5858/arpa.2017-0230-RA. [DOI] [PubMed] [Google Scholar]
- 9.Martinez-Escala M.E., Posligua A.L., Wickless H. Progression of undiagnosed cutaneous lymphoma after anti-tumor necrosis factor-alpha therapy. J Am Acad Dermatol. 2018;78(6):1068–1076. doi: 10.1016/j.jaad.2017.12.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foo S.H., Shah F., Chaganti S., Stevens A., Scarisbrick J.J. Unmasking mycosis fungoides/Sézary syndrome from preceding or co-existing benign inflammatory dermatoses requiring systemic therapies: patients frequently present with advanced disease and have an aggressive clinical course. Br J Dermatol. 2016;174(4):901–904. doi: 10.1111/bjd.14238. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.