1. Case report
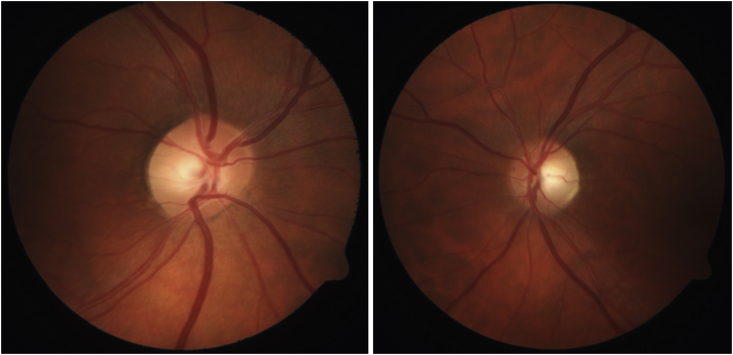
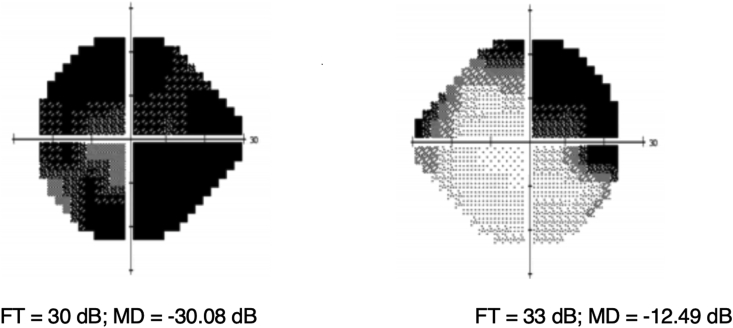
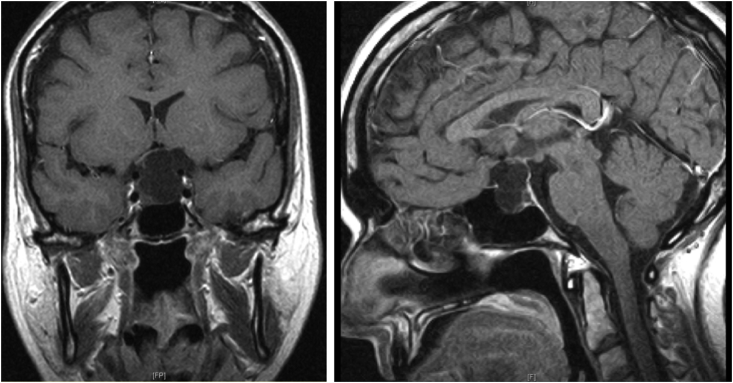
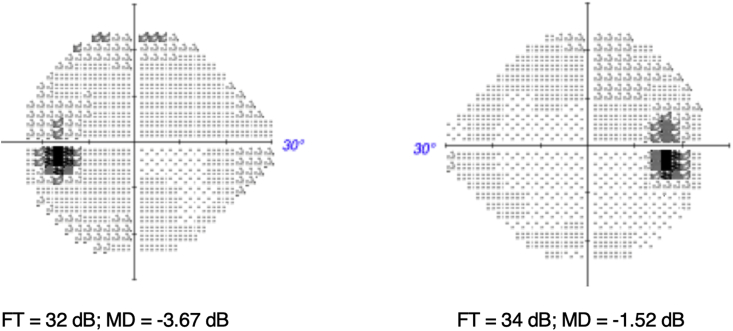
A 44-year-old Caucasian woman presented with sudden awareness of painless vision loss in the left eye while driving. Physical examination revealed visual acuity of 20/20 in the right eye and 20/60 in the left eye, and there was a left relative afferent pupillary defect. The fundus exam was notable for bilateral temporal optic disc pallor, left greater than right (Fig. 1). Automated static perimetry (Humphrey 24-2) revealed a left junctional scotoma (Fig. 2). The patient subsequently underwent magnetic resonance imaging, which showed a 2.7 X 1.7 × 1.7 cm suprasellar arachnoid cyst compressing the left posterior optic nerve and anterior optic chiasm (Fig. 3). The patient underwent uncomplicated endoscopic trans-sphenoidal fenestration of the arachnoid cyst with recovery of her visual acuity to 20/20 in each eye and substantial improvement of her visual fields defect (Fig. 4).
Fig. 1.
Temporal optic disc pallor of the right and left eye, respectively.
Fig. 2.
Humphrey visual fields (24-2) at initial visit demonstrate a left junctional scotoma.
Fig. 3.
Magnetic resonance images show suprasellar arachnoid cyst compressing left posterior optic nerve and left anterior optic chiasm.
Fig. 4.
Humphrey visual fields (24-2) show near-complete resolution of junctional scotoma two months after fenestration of the arachnoid cyst.
2. Discussion
Arachnoid cysts are fluid-filled sacs that occur on the arachnoid membrane; they comprise about 1% of all intracranial space-occupying lesions and are the most common intracranial cysts.1 The exact pathophysiology of arachnoid cysts is unknown, but they are most commonly seen in childhood, or form secondarily to head trauma, intracranial infection, tumor, and surgeries.1 Arachnoid cysts are typically asymptomatic and diagnosed in children who undergo imaging for other reasons. They may, however, cause symptoms such as headache, nausea, vomiting, and dizziness, depending on their size or location. Suprasellar arachnoid cysts may occasionally cause visual symptoms. The differential diagnosis of a suprasellar lesion include cystic pituitary adenoma, meningioma, craniopharyngioma, internal carotid aneurysm, Rathke's cleft cyst, and metastatic disease. There have been reports of suprasellar arachnoid cysts causing oculomotor nerve palsy and endocrine dysfunction,2,3 but to our knowledge no reversible junctional visual fields defect caused by suprasellar arachnoid cyst has been reported. Although the existence of Wilbrand knee is debatable, compression of the ipsilateral posterior optic nerve and anterior optic chiasm can produce the characteristic, localizing junctional scotoma seen in our patient. Management options of suprasellar arachnoid cysts include close observation when patients are asymptomatic. When symptomatic, interventions such as minimally invasive surgical resection, fenestration, shunting, or decompression provide good outcomes.
3. Conclusion
Our patient had severe visual fields defects consistent with the pattern of junctional scotoma in the setting of a suprasellar arachnoid cyst. She underwent a successful fenestration of the arachnoid cyst resulting in complete recovery of her central visual acuity and near-complete resolution of her visual fields defect. We present a case of reversible junctional scotoma caused by suprasellar arachnoid cyst and it serves as an example of how prompt diagnosis and surgical treatment of symptomatic suprasellar arachnoid cyst can afford substantial visual recovery.
Patient consent
Written consent to publish this case has not been obtained. This report does not contain any personal identifying information.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The authors have no financial disclosure.
Acknowledgements
None.
References
- 1.Cincu R., Agrawal A., Eiras J. Intracranial arachnoid cysts: current concepts and treatment alternatives. Clin Neurol Neurosurg. 2007;109(10):837–843. doi: 10.1016/j.clineuro.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Elliott R.E., Tanweer O., Rubin B.A., Koslow M., Mikolaenko I., Wisoff J.H. Suprasellar hamartoma and arachnoid cyst. World Neurosurg. 2013;80(6):e401–e407. doi: 10.1016/j.wneu.2012.01.058. [DOI] [PubMed] [Google Scholar]
- 3.Ashker L., Weinstein J.M., Dias M., Kanev P., Nguyen D., Bonsall D.J. Arachnoid cyst causing third cranial nerve palsy manifesting as isolated internal ophthalmoplegia and iris cholinergic supersensitivity. J Neuro Ophthalmol. 2008;28(3):192–197. doi: 10.1097/WNO.0b013e318183c57c. [DOI] [PubMed] [Google Scholar]