Abstract
Purpose
To demonstrate that rifabutin-related corneal deposits are localized to the deep stroma using anterior segment optical coherence tomography (OCT) and confocal microscopy.
Observations
A 55-year-old male with a history of human immunodeficiency virus (HIV) and disseminated mycobacterium avium complex on rifabutin treatment for 3 years presented with bilateral corneal deposits. Confocal microscopy and anterior segment OCT confirm that rifabutin-related corneal deposits are located in the deep stroma, rather than in the endothelium.
Conclusions
And Importance: Rifabutin deposits localize to the deep corneal stroma, and can be seen with both confocal microscopy and anterior segment OCT. Anterior segment OCT is a widely available and easily used diagnostic tool, and can provide utility in the diagnosis of corneal deposits.
Keywords: Rifabutin, Corneal deposits, Mycobacterium avium complex, Confocal microscopy, Anterior segment OCT
1. Introduction
Patients with human immunodeficiency virus (HIV) primarily develop either disseminated disease or focal lymphadenitis from mycobacterium avium complex (MAC).1 The risk of MAC infection in HIV patients increases when the CD4 count is below 50 cells/uL.1 Rifabutin is part of a multidrug therapy to prevent and treat MAC.1 Its mechanism of action is to inhibit DNA-dependent RNA polymerase in mycobacterial species, and prevent initiation of transcription.2 Rifabutin can cause several adverse effects in the eyes, including uveitis, stellate corneal deposits, anterior lens surface deposits, retinal vasculitis, and abnormal electroretinogram (ERG) with reduction of rod amplitude.3, 4, 5, 6, 7
The location of rifabutin-related corneal deposits has been controversial. Previous studies have reported that these deposits are located in the endothelium,5,8,9 but one recent case report demonstrated that these deposits are in the deep stroma anterior to Descemet's membrane using confocal microscopy.10 We report here findings from anterior segment optical coherence tomography (AS-OCT) using the Spectralis SD-OCT (Heidelberg Engineering, Heidelberg, Germany) and confocal microscopy using the Heidelberg Retinal Tomograph 3 (Heidelberg Engineering, Germany) from a patient previously treated with rifabutin who developed bilateral corneal deposits.
2. Report of the case
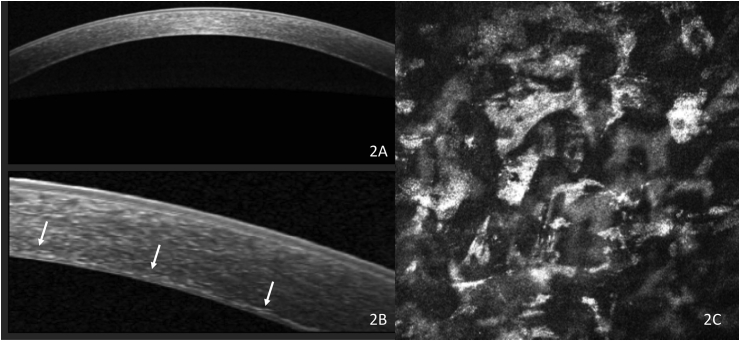
A 55-year-old man with HIV and disseminated MAC on rifabutin therapy for 3 years presented with bilateral diffuse corneal deposits. At the time of presentation, his rifabutin therapy had been discontinued 3 months prior. His best corrected visual acuity was 20/150 in the right eye and 20/200 in the left eye. On examination, he was found to have bilateral, diffuse, fine, pigmented corneal deposits centrally and peripherally presumably in the endothelial layer, bilateral non-visually significant nasal pterygia, and bilateral visually significant cataracts (Fig. 1). There was no evidence of uveitis, anterior lens capsule deposits or retinopathy. Pachymetry was 586um in the right eye and 576um in the left eye. AS-OCT revealed diffuse hyperreflective deposits in the posterior stroma rather than on the endothelium (Fig. 2A and B). Confocal microscopy demonstrated hyperreflective polymorphous deposits in the deep stroma, but none in the endothelium. (Fig. 2C).
Fig. 1.
Diffuse, fine, pigmented deposits distributed diffusely throughout posterior cornea.
Fig. 2.
Anterior segment optical coherence tomography scan showing widefield (A) and magnified (B) scan demonstrating hyperreflective deposits in deep stroma (arrows). Confocal microscopy (C) demonstrates hyperreflective deposits admixed with keratinocytes in deep stroma.
The patient's decreased vision was attributed to his cataracts and he underwent bilateral cataract extraction by phacoemulsification and intraocular lens placement without complication. At his most recent exam 3 months after bilateral cataract surgery, his best corrected visual acuity was 20/20 in both eyes and his corneal deposits were unchanged.
3. Discussion
The first report of rifabutin-associated corneal deposits occurred in 1999 during a phase I-II study of systemic rifabutin to prevent disseminated MAC in 25 children with HIV with CD4 counts of less than 50 cell/uL.5 Six of the 25 children (24%) developed bilateral, stellate corneal endothelial deposits.5 The only significant difference identified in these six children compared to the other 19 was longer duration of rifabutin treatment (mean of 27 months), suggesting that duration is a risk factor for the development of these deposits.5 Holland et al. found that corneal deposits appeared at a mean of 17.8 months for patients on rifabutin.11 The deposits were found to affect the peripheral cornea first, with more concentration inferiorly, followed by spread to the central cornea with longer duration of use.5 These deposits did not affect vision.5 There was no resolution of the deposits despite discontinuation of the rifabutin.5 Interestingly, none of the children developed any evidence of uveitis, which has been shown to be dose-dependent and reversible after discontinuation of the medication or treatment with topical steroids.4 Others have described similar corneal findings in adults with HIV.8,11
Early papers reported the location of these rifabutin-induced corneal deposits to be in the corneal endothelium based on clinical exam.5,8,11 However, Mazzotta et al. used confocal microscopy to demonstrate that these deposits are localized to the deep corneal stroma with no involvement of the endothelium.10 Here, we confirm their findings on confocal microscopy and corroborate it using AS-OCT. AS-OCT is a high-resolution cross-sectional imaging modality. Compared to confocal microscopy, AS-OCT is relatively more comfortable for patients since it does not involve direct eye contact and can obtain images with a larger scan width.
The pathophysiology of rifabutin-induced corneal deposits remains unknown but it has been hypothesized that they could be direct drug toxicity, drug interaction, or drug-HIV interaction. The deposits may originate from the aqueous humor with transendothelial transport and concentrate in the deep stroma due to rifabutin's high lipid solubility.12 Toxicology studies in rats have shown a lipofuscin-like substance deposited in several organs.13 These deposits have not been reported to be visually significant likely due to their predominantly peripheral location on the cornea and good light transmission through these deposits.10 As such, no treatment is recommended.
Given the numerous side effects of rifabutin, it is important for patients on treatment, especially long-term, to undergo a thorough ophthalmological exam. In patients with corneal deposits, which are usually not visually significant, they can be monitored yearly. If available, patients should get AS-OCT, confocal microscopy, pachymetry and endothelial cell count for monitoring.
Consent
Consent to publish this case report has been obtained from the patient in writing.
Funding
The Department of Ophthalmology is supported by an unrestricted educational grant from Research to Prevent Blindness, as well as a departmental Core Grant for Vision Research, NIH-NEI EY002162.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
Dr. Schallhorn is a consultant for Zeiss and Avedro, unrelated to this manuscript.
The following authors have no financial disclosures: Tianyi Zhang, Catherine Sun, Yijie B. Lin.
Acknowledgements
none.
References
- 1.Currier J.S., UpToDate . Mycobacterium avium complex (MAC) infections in HIV-infected patients. In: Bartlett J.G., editor. 2017. Waltham, MA. [Google Scholar]
- 2.Kunin C.M. Antimicrobial activity of rifabutin. Clin Infect Dis : Off. Publ. Infect. Dis. Soc. Am. 1996;22(suppl 1) doi: 10.1093/clinids/22.supplement_1.s3. S3-13;, discussion S13-14. [DOI] [PubMed] [Google Scholar]
- 3.Ponjavic V., Granse L., Bengtsson Stigmar E., Andreasson S. Retinal dysfunction and anterior segment deposits in a patient treated with rifabutin. Acta Ophthalmol Scand. 2002;80:553–556. doi: 10.1034/j.1600-0420.2002.800519.x. [DOI] [PubMed] [Google Scholar]
- 4.Shafran S.D. Determinants of rifabutin-associated uveitis in patients treated with rifabutin, clarithromycin, and ethambutol for Mycobacterium avium complex bacteremia: a multivariate analysis. Canadian HIV Trials Network Protocol 010 Study Group. J Infect Dis. 1998;177:252–255. doi: 10.1086/517366. [DOI] [PubMed] [Google Scholar]
- 5.Smith J.A., Mueller B.U., Nussenblatt R.B., Whitcup S.M. Corneal endothelial deposits in children positive for human immunodeficiency virus receiving rifabutin prophylaxis for Mycobacterium avium complex bacteremia. Am. J. Ophthalmol. 1999;127:164–169. doi: 10.1016/s0002-9394(98)00310-9. [DOI] [PubMed] [Google Scholar]
- 6.Arevalo J.F., Russack V., Freeman W.R. New ophthalmic manifestations of presumed rifabutin-related uveitis. Ophthalmic Surg Laser. 1997;28:321–324. [PubMed] [Google Scholar]
- 7.Jacobs D.S. Acute uveitis associated with rifabutin use in patients with human immunodeficiency virus infection. Am. J. Ophthalmol. 1994;118:716–722. doi: 10.1016/s0002-9394(14)72550-4. [DOI] [PubMed] [Google Scholar]
- 8.Golchin B., McClellan K. Corneal endothelial deposits secondary to rifabutin prophylaxis for Mycobacterium avium complex bacteraemia. Br J Ophthalmol. 2003;87:798–799. doi: 10.1136/bjo.87.6.798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coutinho A.B., Cheema D., Pereira P.R., Souza Filho J.P., Burnier M.N., Jr. Corneal endothelial deposits associated with rifabutin use. J Ocul Pharmacol Therapeut : Off J Assoc Ocular Pharmacol Therapeut. 2005;21:166–169. doi: 10.1089/jop.2005.21.166. [DOI] [PubMed] [Google Scholar]
- 10.Mazzotta C., Traversi C., Nuti E., Sparano M.C., Caporossi A. Rifabutin corneal deposits in a patient with acquired immunodeficiency syndrome: in vivo confocal microscopy investigation. Eur J Ophthalmol. 2009;19:481–483. doi: 10.1177/112067210901900327. [DOI] [PubMed] [Google Scholar]
- 11.Holland S.P., Chang C.W., Vagh M., Courtright P. Corneal endothelial deposits in patients with HIV infection or AIDS: epidemiologic evidence of the contribution of rifabutin. Can J Ophthalmol. 1999;34:204–209. [PubMed] [Google Scholar]
- 12.Blaschke T.F., Skinner M.H. The clinical pharmacokinetics of rifabutin. Clin Infect Dis : Off. Publ. Infect. Dis. Soc. Am. 1996;22(Suppl 1):S15–S21. discussion S21-12. [PubMed] [Google Scholar]
- 13.Brughera M. Overview of toxicological data on rifabutin. Exp Toxicol Pathol : Off J Ges Toxikol Pathol. 1995;47:1–9. doi: 10.1016/s0940-2993(11)80273-3. [DOI] [PubMed] [Google Scholar]