Abstract
Although bladder injury is a rare complication during cesarean delivery (CD), its incidence is increasing due to the growing trend in elective CD. Herein, we report a case of a 28-year-old woman, who presented during labor. An emergency CD and hysterectomy were done to control bleeding. The case was complicated by and inadvertent cystectomy. Urine was diverted immediately by ureterostomy. After five months, augmentation ileocytoplasty, bilateral ureteral re-implantation, and abdominal catheterizable stoma formation were carried out. This case highlights the surgical management of inadvertent cystectomy during CD.
Keywords: Iatrogenic, Bladder injury, Cesarean delivery, CD, cystectomy
Introduction
Iatrogenic bladder injury is a reported complication during pelvic and/or abdominal retroperitoneal surgical manipulation. Although infrequent, cesarean delivery (CD) carries a considerable risk for bladder injury, with and incidence ranging from 0.0016% to 0.94%.1 Therefore, careful consideration should be given to such complications during CD in order to appropriately counsel patients and to properly manage any unprecedented intraoperative complications.
Case presentation
A 28-year-old pregnant lady with 2 children whom were delivered by CD. Her gestational age was 36 during presentation with labor. An emergency CD was carried out, which was complicated with bleeding and hysterectomy was done to control it. The obstetrician called a urologist after noticing a Foley's catheter balloon in the surgical field.
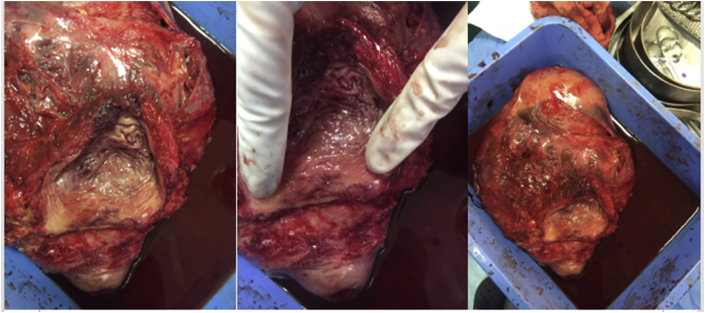
Intraoperatively, the entire bladder body and lower ureters were removed with the uterus, only bladder neck and part of trigon remained [Fig. 1]. As immediate management, both ureteric edges were refreshed and bilateral cutaneous ureterostomy was connected to the anterior abdominal wall. The course went smoothly and urine was collected in a urostomy bag.
Fig. 1.
Ureteric orifices (red arrow). Bladder body (blue star). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
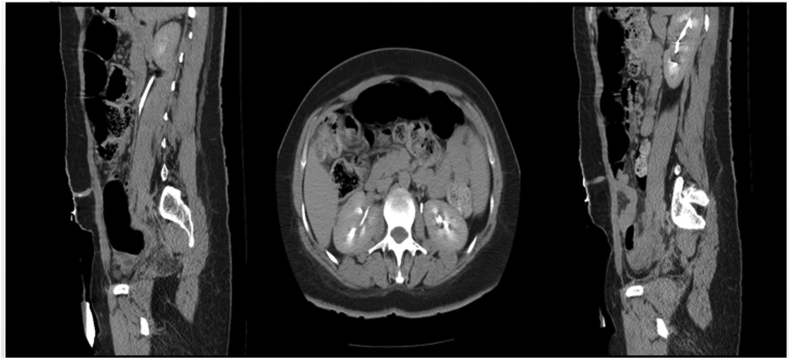
After management, the patient was referred to our institute and counseled for neobladder versus Ileocystoplastic augmentation with abdominal continent catheterizable stoma and ureteral re-implantation. Her serum creatinine was 61.5 μmol/L, and CT urogram revealed normal excretion in both kidneys with no hydronephrosis [Fig. 2].
Fig. 2.
CT urogram 5 months after CD and cystectomy.
Five months later, a midline lower abdominal laparotomy was done, and the bladder was small with volume of 40 cc. It was opened from the upper part and multiple incision were done to widen the bladder opening. Bilateral ureteral re-implantation was done to native bladder. The appendix was used to create catherizable continent stoma to right iliac fossa with anastomosis to native bladder. About 45cm of terminal ilium, proximal to iliocecal junction, was used for ileocystoplasty.
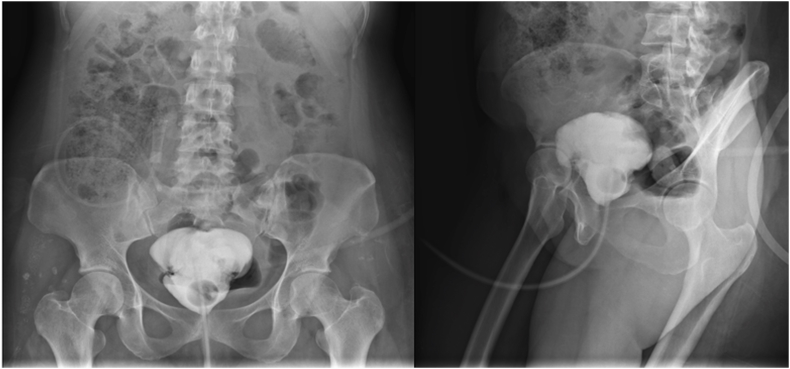
Postoperatively, ureteric catheters and drains were removed by the end of first week. Daily manual gentle wash was done to remove mucus. Cystogram done three weeks after surgery, showing no leak [Fig. 3]. Urethral and suprapubic catheters were removed and she started using 10 Fr. catheter through stoma.
Fig. 3.
Cystogram 3 weeks after augmentation cystoplasty.
During follow-up, she urinated with minimal residual urine for 3 months, however it increased gradually. Currently, she could not urinate, using catheter (through the urethra) to empty her bladder every 6–8 hours and drainung 400-600 ml. Her abdominal stoma obliterated. She was followed for 16 months, with no UTI or hematuria. Now, she is catheterized through her urethra every 6–8 hours without difficulty and no leak in between. Serum creatinine is now 61 μmol/L, with no hydronephronsis in Ultrasound.
Discussion
To the best of our knowledge, this is the first case report of iatrogenic cystectomy during cesarean delivery. Iatrogenic bladder injury can happen during open, laparoscopic, endoscopic, urological, or abdominal surgeries. Iatrogenic bladder injury is a rare complication during cesarean section, with an event rate ranging from 0.0016% to 0.94%.1
Bladder injury during CD was reported to be of higher frequency in multipara women, previous cesarean deliveries, and emergency CD.2 It was noted that the frequency of bladder injury is higher in women with repeated cesarean deliveries (58.5%) compared to women with primary CD (41.2%).3 Similar observations were noted in the literature, where Phipps et al.2 and Rahman et al.3 demonstrated that the incidence of incidental cystotomy was three times higher in women who had a previous cesarean delivery (0.81% vs. 0.27%, P = .0014).
Bladder injury is more likely to occur during emergency CD compared to elective CD, with an event rate of 31% and 11%, respectively. Meanwhile, the incidence of bladder injury was observed to be higher if a trial of normal delivery progressed to second stage (83%) than in those who failed to progress to second stage (61%). It was also noted that the complication of uterine rupture is associated with 14% of bladder injuries.2 Furthermore, there were no significant implications based patient's age or body mass index.2
In our case, only 10–15% of the bladder was left. The primary goal of management was to restore micturition function by having an adequate bladder capacity with low intravesical pressure and no urinary incontinence. The patient was offered neobladder and bilateral ureteral re-implant with continent catheterizable stoma.
Augmentation cystoplasty (AC) is frequently used in the adult population for the treatment of many medical conditions, where the bladder function is compromised or severely affected. These conditions include neurogenic bladder dysfunction, inflammatory diseases (i.e. tuberculous cystitis) with to severely contracted bladder, interstitial cystitis, and eventually the reconstruction of inadvertent bladder injury.4
AC can be carried out with the use of different bowel segments. Enterocystoplasty is general term used to indicate that a part of a bowel segment has been used to improve bladder capacity; however, based on the selected part of the bowel, a different terminology may be applied. The most commonly used bowel part in AC is the detubularized segment of the ileum, and thus, the term ileocystoplasty is applied. In general, augmentation enterocystoplasy has shown favorable outcomes in terms of long-term durability and more frequent patient satisfaction; however, it does not come without complications, as it carries an increased risk of malignancy.5
Spontaneous voiding after augmentation cystoplasty is achieved by abdominal straining to increase abdominal pressure. Hence, Patients should be informed about the possibility of intermittent catheterization. Continent abdominal stomas can be done if the urethra is not suitable for catheterization, as in conditions like urethral stricture, urethral loss, sensitive urethra, and bladder neck reconstruction. The main indication for revision is stenosis and inability to catheterize, followed by leakage.
Conclusion
Pregnant women with secondary or emergent cesarean deliveries should be advised about the significant risk of inadvertent surgical complications and care providers should recognize such complications early enough to manage them properly and reduce associated morbidity.
Informed consent
A signed informed consent was taken from the patient prior to carrying out any of the aforementioned surgeries and manipulations and she agreed to share her case.
Declaration of competing interest
None.
Contributor Information
Muhammad Alahmadi, Email: mu7ammad87@icloud.com.
Abdullah Ahmed Ghazi, Email: aaq997@yahoo.com.
References
- 1.Aghaways I., Bapir R., Hawrami T.A., Thahir N.M., Al Kadum Hassan M.A., Salih Hassan K.M. Conservative management of delayed presentation of intraperitoneal bladder rupture following caesarean delivery: a case report. Int J Surg Case Rep. 2019;59:31–34. doi: 10.1016/j.ijscr.2019.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phipps M.G., Watabe B., Clemons J.L., Weitzen S., Myers D.L. Risk factors for bladder injury during cesarean delivery. Obstet Gynecol. 2005;105:156–160. doi: 10.1097/01.AOG.0000149150.93552.78. [DOI] [PubMed] [Google Scholar]
- 3.Rahman M., Gasem T., Al Suleiman S., Al Jama F.E., Burshaid S., Rahman J. Bladder injuries during cesarean section in a University Hospital: a 25-year review. Arch Gynecol Obstet. 2009;279:349–352. doi: 10.1007/s00404-008-0733-1. [DOI] [PubMed] [Google Scholar]
- 4.Reyblat P., Ginsberg D.A. Augmentation cystoplasty: what are the indications? Curr Urol Rep. 2008;9:452–458. doi: 10.1007/s11934-008-0078-0. [DOI] [PubMed] [Google Scholar]
- 5.Welk B., Herschorn S., Law C., Nam R. Population based assessment of enterocystoplasty complications in adults. J Urol. 2012;188:464–469. doi: 10.1016/j.juro.2012.04.013. [DOI] [PubMed] [Google Scholar]