Abstract
Background:
A walking cadence of ≥100 steps/min corresponds to minimally moderate intensity, absolutely-defined as ≥3 metabolic equivalents (METs). This threshold has primarily been calibrated during treadmill walking. There is a need to determine the classification accuracy of this cadence threshold to predict intensity during overground walking.
Methods:
In this laboratory-based cross-sectional investigation, participants (N=75, 49.3% women, age 21–40 years) performed a single 5-min overground (hallway) walking trial at a self-selected preferred pace. Steps accumulated during each trial were hand tallied and converted to cadence (steps/min). Oxygen uptake was measured using indirect calorimetry and converted to METs. The classification accuracy (sensitivity, specificity, overall accuracy and positive predictive value) of ≥100 steps/min to predict ≥3 METs was calculated.
Results:
A cadence threshold of ≥100 steps/min yielded an overall accuracy (combined sensitivity and specificity) of 73.3% for predicting minimally moderate intensity. Moreover, for individuals walking at a cadence ≥100 steps/min, the probability (positive predictive value) of achieving minimally moderate intensity was 80.3%.
Conclusions:
Although primarily developed using treadmill-based protocols, a cadence threshold of ≥100 steps/min for young adults appears to be a valid heuristic value (evidence-based, rounded, practical) associated with minimally moderate intensity during overground walking performed at a self-selected preferred pace.
Keywords: physical activity, accelerometry, pedometry, guidelines and recommendations
INTRODUCTION
Consistent evidence has demonstrated a relationship between levels of habitual physical activity (PA) and all-cause mortality,1–3 as well as improvements in numerous other health outcomes.4 Importantly, the benefits of PA follow a dose-response relationship with increasing volume and intensity.4 Current U.S. recommendations4,5 state that adults should aim to accrue ≥150 min/week of moderate or ≥75 min/week of vigorous intensity aerobic PA (or some equitable combination thereof). These guidelines are based on an absolute definition of intensity, i.e., metabolic equivalents (METs), whereby 1 MET = 3.5 mL O2/kg/min (standardized resting energy expenditure), and intensity levels are expressed as multiples of this base unit. Specifically, moderate and vigorous intensities are defined as 3.0-5.9 (METs) and ≥6 METs, respectively.4 While exercise scientists and health professionals may be familiar with these and other physiology-based definitions of intensity (e.g., percent of oxygen uptake reserve or heart rate reserve),6 lay audiences may struggle to comprehend their meaning, and in turn, fail to accurately evaluate whether they are achieving the intended intensity to meet PA guidelines.
Walking is a feasible (low cost and low skill) mode of PA and is thus often recommended as a means of achieving public health PA guidelines.5,7 Notably, walking cadence (steps/min) has been established as a valid proxy of ambulatory intensity8,9 and promoted as a simple and practical method for gauging intensity in the free-living setting.8,9 We previously described the calibration of cadence-intensity thresholds (i.e., cadence values associated with increasing levels of intensity in a sample of young adults (21–40 years of age) during treadmill walking.10 We confirmed previous reports11–18 that a heuristic (evidence-based, rounded, practical) cadence of ≥100 steps/min corresponds to minimally moderate intensity (≥3 METs) during treadmill walking in young adults. This direct translation of a commonly accepted MET-defined intensity level into a cadence threshold has the potential to improve public health messaging of PA guidelines, especially given that a step is a commonly understood unit of human movement. Notably, among the previously published studies,11–18 three12,14,17 investigated the cadence-intensity relationship during overground walking. Additionally, these three studies all constrained cadence or speed in some fashion (e.g., using rhythmic auditory cuing or timing). To our knowledge, no studies have examined the classification accuracy of ≥100 steps/min to predict minimally moderate intensity (≥3 METs) during overground walking at a self-selected preferred pace.
The aim of this secondary analysis of the CADENCE-Adults study was to determine the classification accuracy (i.e., sensitivity, specificity, overall accuracy) of a cadence threshold of ≥100 steps/min to predict a minimally moderate intensity (i.e., ≥3.0 METs) during overground walking at a self-selected preferred (normal or usual) pace. This analysis will evaluate whether this consensus threshold originally set with our own10 and others’ previous research11–18 using treadmill or constrained overground walking protocols can be applied with similar accuracy during self-selected overground walking at a preferred pace.
METHODS
Study design and setting
The CADENCE-Adults study was a laboratory-based, cross-sectional design investigating the relationship between cadence and metabolic intensity across the adult lifespan (21-85 years of age). The primary aims, full methods, and results from the first report (focused on adults 21-40 years of age) from the CADENCE-Adults study are published elsewhere.10 The protocol is also registered at ClinicalTrials.gov (NCT02650258). Briefly, the participants completed an incremental, sub-maximal treadmill walking protocol that allowed us to link directly observed cadence (hand tally; criterion standard for step counting) with increasing levels of absolutely-defined intensity (oxygen uptake from indirect calorimetry converted to METs; criterion standard). In addition, the participants also completed several simulated activities of daily living, one of which was a 5-min overground walking trial that is the focus of this secondary analysis. Data collection for this younger cohort was conducted in the Physical Activity and Health Laboratory, Department of Kinesiology, University of Massachusetts Amherst between January and October, 2016. The study protocol was approved by the University of Massachusetts Amherst Institutional Review Board. Informed consent was provided by all participants prior to enrollment in the study. Where possible, we complied with the STROBE checklist19 to improve the transparency of our reporting.
Participants
The participant sample evaluated herein are the same sample of younger adults as the previous report10 which focused on the treadmill walking aspects of the study protocol. A full description of the study recruitment and selection procedures, and sample size justification are available elsewhere.10 Briefly, we recruited a sex and age balanced sample of 10 apparently healthy young men and women per 5-year age-group (i.e., 21-25, 26-30, 31-35, 36-40 years). Eligible participants were able to walk without assistance and free from injury, illness or disability that would affect their metabolic response to exercise or ability to walk overground or on a treadmill.
Procedures and measures
Participants completed an overground walking trial in a hallway (corridor). Participants were instructed to walk for 5 min at their self-selected preferred (normal or usual) walking pace, looping around two cones that were set 13 m apart. We directly observed and counted each individual’s total steps using a hand tally counter, with a video recording as a redundant record of steps for verification purposes. Oxygen uptake (VO2; mL/kg/min) was measured using a validated20 portable indirect calorimeter (Oxycon Mobile; CareFusion BD Germany 234 GmbH, Höchberg, Germany) and exported in 5-second epochs. In addition to the above measures, basic demographic (e.g., age, sex) and anthropometric information (e.g., height, weight, BMI and leg length) were collected. Detailed descriptions of the procedures for these measurements can be found in the previous report.10
Data treatment
Custom MATLAB (The MathWorks, Natick, MA) and R (Version 3.5.1, R Core Team, Vienna, Austria) scripts were used to import and combine sample characteristics, cadence, and VO2 data. Cadence was calculated as the total number of steps accumulated within a bout, divided by the duration of the bout (i.e., hand tallied steps/5-min). Mean VO2 values during minutes 2:45–4:45 of each 5-min trial were averaged. Mass-specific VO2 (mL/kg/min) values were converted to metabolic equivalents (METs) using standard procedures4 (i.e., dividing by 3.5 mL/kg/min). Minimally moderate absolute intensity was defined as ≥3.0 METs. Notably, two individuals reached an intensity level consistent with the definition for vigorous intensity (i.e., ≥ 6 METs)4. Although unexpected, these values were retained in the analysis and coded simply as minimally moderate intensity. Finally, to facilitate the analyses outlined below, two new binary variables were created: 1) cadence <100 or ≥100 steps/min; and 2) intensity <3 or ≥3 METs.
Analytical sample
Data from five of the 80 participants (two men and three women) were removed from the data set due to identified malfunction of the portable indirect calorimeter during testing. The final analytical data set therefore consisted of 75 participants with complete measures (sample characteristics, cadence, and VO2). These finalized data and an accompanying data dictionary are provided in Supplementary files 1 and 2, respectively.
Statistical analyses
All analyses were performed in R (Version 3.5.1) with the α level set at 0.05. Sample characteristics were summarized by sex and reported as mean ± standard deviation (SD). In addition, frequencies and percentages (proportions) were computed for individuals who naturally self-selected to walk at cadence ≥100 steps/min or achieved minimally moderate intensity (≥3 METs). Intensity values were also summarized (mean ± SD) separately for individuals categorized as walking at either <100 steps/min or ≥100 steps/min. Differences in characteristics between these two groups of individuals were evaluated using Welch’s two sample t-tests. Normality of distribution within groups and homogeneity of variances between groups were assessed for each outcome using Shapiro-Wilk tests and F-Tests, respectively. Pearson’s correlation (r) between cadence and MET-intensity was also computed to describe the strength of relationship between these two variables.
To address the primary aim, we calculated the classification accuracy (sensitivity, specificity, accuracy, positive predictive value [PPV], and negative predictive value [NPV]) of a cadence threshold of ≥100 steps/min to predict minimally moderate intensity (≥3 METs). This analysis was performed using the “pROC” package21 in R. To aid with interpretation of the data, true positive, false positive, true negative and false negative rates were also extracted.
RESULTS
Characteristics of the sample
Table 1 reports a summary (n, %; mean ± SD) of the study sample demographics, anthropometrics and outcome measures. As per our strategic recruitment plan, half (n = 37, 49.3%) of the sample were women. The participants predominately identified as being White (64.4%), reflecting the local demographics, with the next highest representations being Asian (21.9%), Hispanic (5.5%), Black/African American (2.7), Other (2.7%), American Indian (1.4%), unknown or not reported (1.4%).
Table 1.
Characteristics of the sample (N= 75)
| Outcome | Mean ± SD |
|---|---|
| Age (years) | 30.5 ± 5.8 |
| Height (cm) | 170.7 ± 9.4 |
| Weight (kg) | 72.8 ± 14.2 |
| BMI (kg/m2) | 24.8 ± 3.4 |
| Leg length (cm) | 79.7 ± 5.9 |
| Cadence (steps/min) | 107.7 ± 8.2 |
| Intensity (METs) | 3.5 ± 0.7 |
Note: BMI – body mass index,
METs – metabolic equivalents
Figure 1 displays the cadence-intensity relationship (Pearson r = 0.48) observed during the overground walking trial. The mean ± SD cadence was 108 ± 8 steps/min, and intensity was 3.5 ± 0.7 METs. In total, 61 of 75 participants (81.3%) naturally selected to walk at a cadence ≥100 steps/min and 57 of 75 participants (76.0%) achieved ≥3 METs. Individuals who walked at ≥100 steps/min achieved an intensity of 3.6 ± 0.7 METs, while those who walked at <100 steps/min averaged 3.1 ± 0.3 METs (Welch’s two sample t-test: t = −4.65, df = 46.42, p < 0.001, Cohen’s d = 1.05). On average, individuals who walked at ≥100 steps/min were shorter (1.7 ± 0.1 m vs 1.8 ± 0.1 m, t = 2.36, df = 23.29, p = 0.03, Cohen’s d = 0.65) and had shorter leg lengths (79.0 ± 6.0 cm vs 82.8 ± 4.3 cm, t = 2.73, df = 24.57, p = 0.01, Cohen’s d = 0.73). No differences were observed for age, weight or BMI (p > 0.05).
Figure 1.
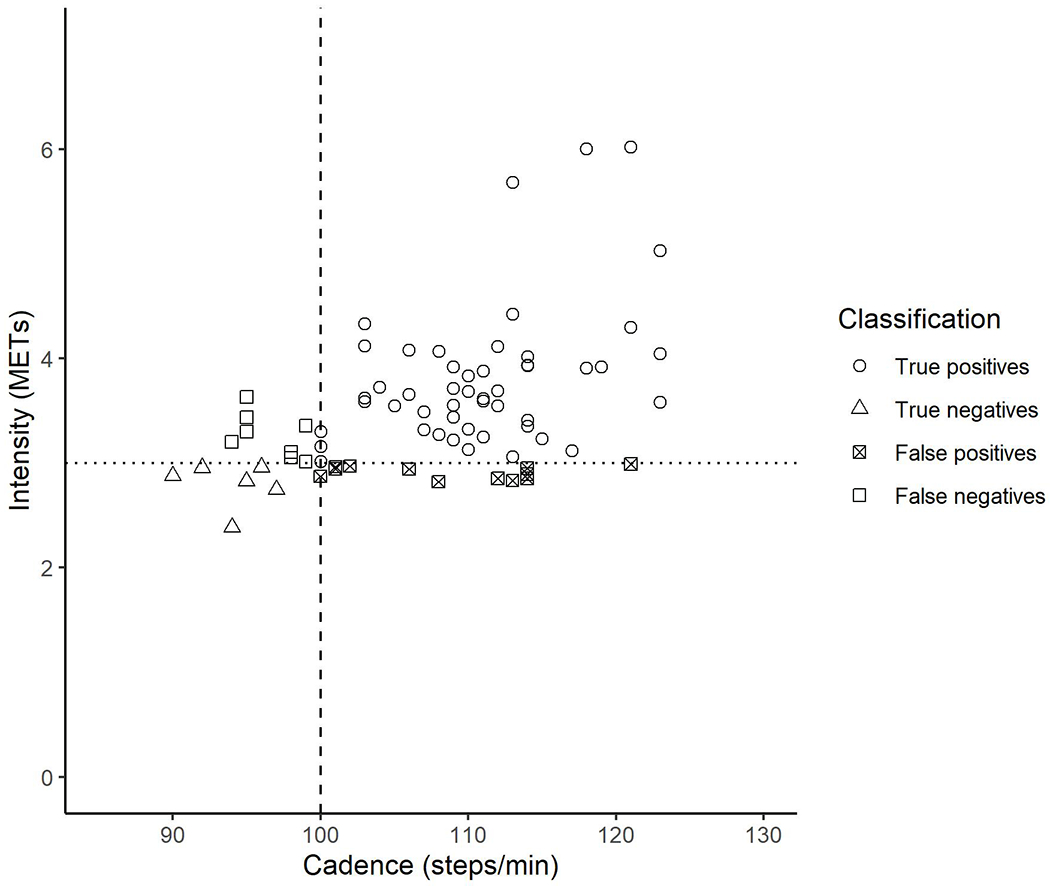
Scatter plot of cadence (steps/min) and intensity (metabolic equivalents [METs]) values observed during overground walking at a self-selected preferred walking pace. The shapes of the data points represent the classification of bouts as true positives (open circles), true negatives (open triangles), false positives (squares with cross), and false negatives (open squares). The dotted line signifies absolutely defined minimally moderate intensity (≥3 METs). The dashed line represents the heuristic moderate-intensity cadence threshold (≥100 steps/min).
Classification accuracy
Table 2 reports the classification accuracy (sensitivity, specificity, accuracy, PPV, NPV) for a cadence threshold of ≥100 steps/min to predict minimally moderate intensity (≥3 METs). The overall accuracy was 73.3% (combined sensitivity and specificity), and the PPV was 80.3%. In other words, the probability of an individual achieving minimally moderate intensity when walking at a cadence ≥100 steps/min was ~80%. Table 3 reports the true positive, true negative, false positive, false negative values for classifying minimally moderate intensity at a cadence ≥100 steps/min. The true positive rate was 65.3% (n = 49), meaning that ~65% of participants in this sample naturally selected to walk at a cadence ≥100 steps/min and also achieved minimally moderate intensity (≥3 METs).
Table 2.
Classification accuracy of ≥100 steps/min to predict minimally moderate intensity in overground walking (≥3 metabolic equivalents)
| Cadence (steps/min) | Sensitivity | Specificity | Accuracy | PPV | NPV | |
|---|---|---|---|---|---|---|
| Value | 100 | 86.0 | 33.3 | 73.3 | 80.3 | 42.9 |
PPV – Positive predictive value, NPV – Negative predictive value
Table 3.
Confusion matrix for classification of minimally moderate intensity (≥3 metabolic equivalents) during overground walking based on a cadence threshold of >100 steps/min
| ≥3 METs | <3 METs | Total | |
|---|---|---|---|
| ≥100 steps/min |
True Positive 49 (65.3%) |
Fales Positive 12 (16.0%) |
61 (81.3%) |
| <100 steps/min |
False Negative 8 (10.7%) |
True Negative 6 (8.00%) |
14 (18.7%) |
| Total | 57 (76.0%) | 18 (24.0%) | 75 (100%) |
Note: Values are n (%). METs – metabolic equivalents
DISCUSSION
In our first report from the CADENCE-Adults study,10 we described the calibration of cadence thresholds corresponding to MET-intensity levels in younger adults (21-40 years of age) during treadmill walking. Specifically, we confirmed findings from previous studies11–18 that a cadence threshold of ≥100 steps/min corresponded to an absolutely-defined minimally moderate intensity (≥3.0 METs). The primary aim of this secondary analysis of the CADENCE-Adults study was to determine the classification accuracy of a cadence threshold of ≥100 steps/min to predict minimally moderate intensity during overground walking at a self-selected preferred pace in the same sample of young adults. Herein we report that ≥100 steps/min had an overall accuracy of 73.3% for predicting minimally moderate intensity. Furthermore, the probability of achieving ≥3 METs when walking at a cadence ≥100 steps/min was 80.3%. The results of this secondary analysis extend the findings from our treadmill-based protocol,10 demonstrating that a cadence threshold of ≥100 steps/min accurately predicts moderate intensity in young adults during overground walking at self-selected preferred pace. In addition, considering the independence of our sample from other studies,11–18 these findings also demonstrate the generalizability of these results for 21-40 year olds.
Herein we report that a cadence threshold of ≥100 steps/min demonstrated good sensitivity (86.0%) and overall accuracy (73.3%) for correct classification of ≥3 METs during overground walking at a self-selected preferred pace. The sensitivity value (86%) was exactly the same during treadmill-based walking.10 However, this threshold also had relatively poor (33.3%) specificity i.e., ability to detect true negatives (intensity <3 METs when cadence <100 steps/min), thus lowering the overall accuracy value (73.3%) when compared to our treadmill-based findings (89.6%).10 The conversion of cadence and intensity into binary classifiers for this specific analysis requires careful consideration. For example, for individuals classified as false positives (i.e., intensity <3 METS when cadence ≥100 steps/min), the mean intensity was 2.9 ± 0.1 METs. This value is only marginally lower (−0.1 METs) and arguably not meaningfully different from the minimal intensity recommendation in PA guidelines (≥3 METs). To be clear, given that the health benefits of physical activity follow a dose-response relationship, it is difficult to argue that individuals walking at this exact intensity would not receive the same/similar benefits compared to those walking at ≥3 METs. In addition, we observed relatively fewer cases <3 METs (n = 18, 24%), compared to ≥3 METS (n = 57, 76%). We acknowledge that the small number of cases walking at <3 METs is a limitation when calculating the proportion of bouts classed as true negatives (n = 6, 8%) and false positives (n = 12, 16%. The addition of overground walking trials at self-selected slow and fast paces in future studies would provide a more evenly balanced data set of both lower (<3 METs) and higher (≥3 METs) intensity values. This would likely result in a more robust assessment of both sensitivity and specificity. Also, the addition of multiple observations per participant (i.e., slow-, preferred-, and fast-paced bouts) would allow for analyses that consider repeated measures designs, including more complex regression-based methods.
Studies investigating the cadence-intensity relationship have typically employed treadmill protocols with incremental changes in speed to calibrate cadence-intensity thresholds, 10,11,13,15,16,18 with the consensus8,9 that ≥100 steps/min corresponds to minimally moderate intensity. Fewer studies12,14,17 have investigated the cadence-intensity relationship during overground walking in healthy adults. In a small sample of 20 young healthy adults, Beets et al.12 found that a cadence of 100.2 steps/min was associated with ≥3 METs. Although their findings agree with our results, there are some methodological differences that should be considered. Specifically, in their study protocol, overground walking speed was constrained (set) by a researcher walking in front of the participant across 5 progressive walking speeds (0.50, 0.75, 1.00, 1.25, and 1.50 m/s).12 Similarly, in a sample of 75 adults, Rowe et al.14 used a metronome to constrain cadence during overground walking trials, reporting that a cadence of 103 steps/min was associated with ≥3 METs. Finally, in a sample of 226 young adults, Wang et al.17 reported that a cadence of 105 steps/min was associated with ≥3 METs. Again, walking speeds (3.8, 4.8, 5.6 and 6.4 km/h) were constrained, in this case by asking participants to “…maintain the preset walking speed by following the instructions and markers on the ground…”.17 Importantly, there is evidence to suggest metabolic differences during constrained versus unconstrained walking trials.22 In other words, there appears to be an increased metabolic cost associated with the effort of matching and/or maintaining an externally set walking speed/cadence. This may limit the generalizability of the findings of Beets,12 Rowe,14 and Wang17 to constrained walking conditions. The inclusion of self-selected preferred walking pace in the present study allows for a more natural exploration of the cadence-intensity relationship during overground walking that may more accurately represent walking behavior in the free-living setting.
The results reported herein continue to support the use of a heuristic (evidence-based, rounded, practical) value of ≥100 steps/min corresponding to an absolutely-defined minimally moderate intensity (≥3 METs) in young adults. Moreover, our findings have potential implications for physical activity/public health messaging. For example, PA guidelines currently suggest accumulating moderate-to-vigorous PA time by walking at a “brisk” pace, which could be further defined as a cadence ≥100 steps/min. Individuals could track their cadence to ensure they are achieving ≥100 steps/min by simply counting the number of steps accumulated over 1 min (or 15 s multiplied by 4). Alternatively, some newer wearable technologies provide real-time (instantaneous) readings of cadence that would enable individuals to modulate and/or maintain a cadence ≥100 steps/min. Both methods would increase the likelihood of reaching an absolutely-defined minimally moderate intensity. In addition, our results might be of interest to researchers using accelerometers to measure PA. Researchers could quantify time spent at or above moderate-intensity PA during free-living observation by applying a cadence threshold of ≥100 steps/min to their data sets.
To our knowledge, this is the first study to evaluate the classification accuracy of a cadence threshold of ≥100 steps/min to predict ≥3 METs during self-selected preferred pace overground walking in young adults. This study had several other strengths, including the use of criterion standards for the assessment of walking cadence and intensity and the inclusion of an age- and sex-balanced sample of young adults. There are also several limitations that should be considered. First, and as indicated previously, our sample was delimited to the same set of young adult participants from our previous report.10 Although this may be considered a limitation to the generalizability of the findings, importantly, these individuals are independent from other similar studies examining the cadence-intensity relationship.11–18 As such, our independent results demonstrate the generalizability of ≥100 steps/min to predict minimally moderate intensity during overground walking in young adults (21–40 years of age). Future reports from the CADENCE-Adults study will present the same analyses in middle-aged (41–60 years of age) and older adults (61–85 years of age) as data are finalized. Second, the study protocol only included a single 5-min bout of walking at a self-selected preferred (usual or normal) pace. A future study that includes self-selected slow, normal and fast overground walking trials in young-, middle- and older-aged adults (and the resulting wider range of observed cadence and intensity values) would provide a more evenly balanced data set. This will allow for a more robust evaluation of sensitivity, specificity and overall accuracy values. Finally, this report focused on the relationship between walking cadence and absolutely-defined intensity (METs). Although the relationship between cadence and expressions of relative (individualized) intensity (e.g., percentage of VO2 reserve, heart rate reserve or heart rate maximum) have been the focus of other studies,16,23,24 we chose to use absolutely-defined intensity in MET-based units given its widespread use in PA guidelines. Future analyses that are outside the scope of this initial focus will further explore relationships with relative-intensity markers.
CONCLUSION
Walking is often recommended as a means of achieving public health PA guidelines, which emphasize both the volume and intensity of PA.4,5 Yet, it remains difficult for the general public to precisely quantify their intensity without the assistance of technology (e.g., heart rate monitors). The results reported herein demonstrate that walking at a cadence of ≥100 steps/min, corresponds with an absolutely-defined minimally moderate intensity (≥3 METs) in young adults. Future studies should investigate the relationship between overground walking cadence and intensity across a wider age-span (i.e., middle- and older-aged participants) and across a wider range of self-selected paces (e.g., slow, normal, fast).
Supplementary Material
Acknowledgments
Funding source/trial registration
The CADENCE-Adults study was supported by an award NIH NIA Grant 5R01AG049024. The funding agency had no role in the design of the study, the collection, analysis, or interpretation of data, or in the writing or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The study protocol is registered at www.clinicaltrials.gov (No. NCT02650258).
Footnotes
SUPPLEMENTARY FILES
Supplementary file 1 - Final data set.csv
Supplementary file 2 - Data dictionary.xls
REFERENCES
- 1.Sadarangani KP, Hamer M, Mindell JS, Coombs NA, Stamatakis E. Physical activity and risk of all-cause and cardiovascular disease mortality in diabetic adults from Great Britain: pooled analysis of 10 population-based cohorts. Diabetes Care. 2014;37(4):1016–1023. [DOI] [PubMed] [Google Scholar]
- 2.Arem H, Moore SC, Patel A, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015;175(6):959–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–1310. [DOI] [PubMed] [Google Scholar]
- 4.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee scientific report. Washington, DC: U.S. Department of Health and Human Services;2018. [Google Scholar]
- 5.US Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. In. Wasington, DC: U.S. Dept of Health and Human Services; 2018. [Google Scholar]
- 6.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. [DOI] [PubMed] [Google Scholar]
- 7.Morris JN, Hardman AE. Walking to health. Sports Med. 1997;23(5):306–332. [DOI] [PubMed] [Google Scholar]
- 8.Tudor-Locke C, Rowe DA. Using cadence to study free-living ambulatory behaviour. Sports Med. 2012;42(5):381–398. [DOI] [PubMed] [Google Scholar]
- 9.Tudor-Locke C, Han H, Aguiar EJ, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med. 2018;52(12):776–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tudor-Locke C, Aguiar EJ, Han H, et al. Walking cadence (steps/min) and intensity in 21–40 year olds: CADENCE-adults. Int J Behav Nutr Phys Act. 2019;16(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abel M, Hannon J, Mullineaux D, Beighle A. Determination of step rate thresholds corresponding to physical activity intensity classifications in adults. J Phys Act Health. 2011;8(1):45–51. [DOI] [PubMed] [Google Scholar]
- 12.Beets MW, Agiovlasitis S, Fahs CA, Ranadive SM, Fernhall B. Adjusting step count recommendations for anthropometric variations in leg length. J Sci Med Sport. 2010;13(5):509–512. [DOI] [PubMed] [Google Scholar]
- 13.Marshall SJ, Levy SS, Tudor-Locke CE, et al. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes. Am J Prev Med. 2009;36(5):410–415. [DOI] [PubMed] [Google Scholar]
- 14.Rowe DA, Welk GJ, Heil DP, et al. Stride rate recommendations for moderate-intensity walking. Med Sci Sport Exer. 2011;43(2):312–318. [DOI] [PubMed] [Google Scholar]
- 15.Tudor-Locke C, Sisson SB, Collova T, Lee SM, Swan PD. Pedometer-determined step count guidelines for classifying walking intensity in a young ostensibly healthy population. Can J Appl Physiol. 2005;30(6):666–676. [DOI] [PubMed] [Google Scholar]
- 16.O’Brien MW, Kivell MJ, Wojcik WR, d’Entremont G, Kimmerly DS, Fowles JR. Step rate thresholds associated with moderate and vigorous physical activity in adults. Int J Environ Res Public Health. 2018;15(11):2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang H, Zhang YF, Xu LL, Jiang CM. Step rate-determined walking intensity and walking recommendation in Chinese young adults: a cross-sectional study. BMJ Open. 2013;3(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peacock L, Hewitt A, Rowe DA, Sutherland R. Stride rate and walking intensity in healthy older adults. J Aging Phys Act. 2014;22(2):276–283. [DOI] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosdahl H, Gullstrand L, Salier-Eriksson J, Johansson P, Schantz P. Evaluation of the Oxycon Mobile metabolic system against the Douglas bag method. Eur J Appl Physiol. 2010;109(2):159–171. [DOI] [PubMed] [Google Scholar]
- 21.Robin X, Turck N, Hainard A, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wezenberg D, de Haan A, van Bennekom CA, Houdijk H. Mind your step: metabolic energy cost while walking an enforced gait pattern. Gait Posture. 2011;33(4):544–549. [DOI] [PubMed] [Google Scholar]
- 23.Serrano F, Slaght J, Senechal M, Duhamel T, Bouchard DR. Identification and Prediction of the Walking Cadence Required to Reach Moderate Intensity Using Individually-Determined Relative Moderate Intensity in Older Adults. J Aging Phys Act. 2017;25(2):205–211. [DOI] [PubMed] [Google Scholar]
- 24.Slaght J, Senechal M, Bouchard DR. Impact of Walking Cadence Prescription to Reach the Global Physical Activity Recommendations in Older Adults. J Aging Phys Act. 2017;25(4):604–611. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


