Highlights
-
•
COVID-19 has neuro-invasion potential independently of the critical disease process.
-
•
Cerebrovascular diseases such as ischemia may develop in the course of disease.
-
•
Increased inflammation may be predicted by CRP and D-dimer levels.
-
•
The elder Covid-19 patients with prothrombotic risk factors should also be considered for the signs of stroke.
Keywords: Coronavirus, COVID-19, Stroke, Ischemia
Abstract
Coronaviruses are revealed to target the human respiratory system mainly. However, they also have neuro-invasive abilities and might spread from the respiratory system to the central nervous system. Herein, we report four patients with COVID-19 simultaneously diagnosed with acute ischemic stroke. There were four stroke cases with simultaneously diagnosis of Covid-19 till the April 14, 2020 in the city of Sakarya, Turkey. They were aged between 45 and 77 years. All four cases were likely to have contracted the virus in Sakarya. The patients had all commonly reported symptoms of Covid-19. Three patients have elevated D-dimer levels, and two of them had high C-reactive protein (CRP) levels. They were managed symptomatically for both the infection and the stroke. Our findings suggest that ischemic cerebrovascular diseases may simultaneously develop in the course of Covid-19 independently of the critical disease process. Increased inflammation predicted by CRP and D-dimer levels may play a role in the formation of ischemia. In particular, elder patients with prothrombotic risk factors should also be considered for the signs of cerebrovascular events in addition to infectious symptoms.
1. Introduction
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes coronavirus disease 2019 (COVID-19), was first detected in December 2019 [1]. Approximately 2.4 million cases have been reported up to date, including approximately 83.000 confirmed cases in Turkey [2]. The prominent symptoms of COVID-19 are fever, cough and fatigue, as well as hemoptysis, and dyspnea. In severe cases, patients develop pneumonia, acute respiratory distress syndrome (ARDS), acute cardiac problems, and multiple organ failure [4]. Besides, SARS-CoV-2 also has neuro-invasive abilities and might spread from the respiratory system to the central nervous system [3], [4]. It was recently shown that some patients with COVID-19 have neurological symptoms, such as headache, anosmia, dysgeusia, dizziness, and impaired consciousness [4], [5]. COVID-19 may also predispose to cerebrovascular diseases due to excessive inflammation, immobilization, hypoxia, and diffuse intravascular coagulation [6]. In this case series, 4 patients with COVID-19 were reported to be simultaneously accompanied by neurological involvement of acute ischemic stroke independently of the critical disease course. Although the pathophysiology of the neurological signs caused by COVID-19 have not been investigated in a detailed manner, the spectrum and intensities of these manifestations need to be explored.
2. Case report
All four cases were infected by the SARS-CoV-2 in the city of Sakarya, Turkey. They patients were aged between 45 and 77 years. The demographic and clinical features of the patients were summarized in Table 1 . All of these patients managed in our neurology clinic at Education and Research Hospital of Sakarya University. The chest computed tomography (CT) revealed ground-glass opacities and accompanying consolidated areas which were compatible with Covid-19 pneumonia in all cases. The Covid-19 PCR tests of oropharyngeal and nasopharyngeal swabs were positive in all 4 cases. They were treated with hydroxychloroquine and azithromycin. All patients had increased blood pressure (≥130/80 mmHg) at admission of stroke. Intravenous alteplase or mechanical thrombectomy treatments were not indicated. Therefore, they were managed with antithrombotic therapy, blood pressure control, intravenous fluids and supportive care.
Table 1.
The demographic and clinical features of the presented COVID-19 patients with stroke.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age, Gender | 45 years old, woman | 67 years old, woman | 72 years old, man | 77 years old, man |
| Approximate date after Covid-19 when stroke diagnosed | 4 | 1 | 1 | 2 |
| Stroke risk factors | Diabetes Mellitus | Hypertension | Hypertension | Hypertension |
| Ventilated/Critically ill | None | None | None | None |
| Treatment | Aspirin and low dose LMWH | Aspirin and Klopidogrel | Aspirin and low dose LMWH | Aspirin and Klopidogrel |
| Outcome | Bedridden | Discharged well | Bedridden | Discharged well |
| Thorax CT Findings | Typical findings for coronavirus infection | Typical findings for coronavirus infection | Typical findings for coronavirus + Sub-centric metric pleural effusion in both pleural leaves | Typical findings for coronavirus infection + Several non-specific solid nodules, 4 mm in size, were observed in the apical segment of the right upper lobe |
| NIHSS | 16 | 5 | 10 | 2 |
| Stroke type | Large vessel stenosis (Total right median cerebral artery infarction) | Small vessel occlusion (Left lenticulostriate artery infarction) | Large vessel stenosis (Left median cerebral artery infarction) | Small vessel occlusion (Pontine infarction, basilar artery-pontine branches) |
| D-dimer (0–500 ugFEU/L) | 803 | 1040 | 644 | 378 |
| Ferritin (4.6–204 U/L) | 264 | 79 | 132 | 127 |
| C- reactive protein (0–5 mg/L) | 142 | 4 | 33 | 366 |
| Neutrophyl/Lymphocyte (K/uL) | 6.83/0.85 | 2.93/1.40 | 9.88/1.40 | 5.58/1.65 |
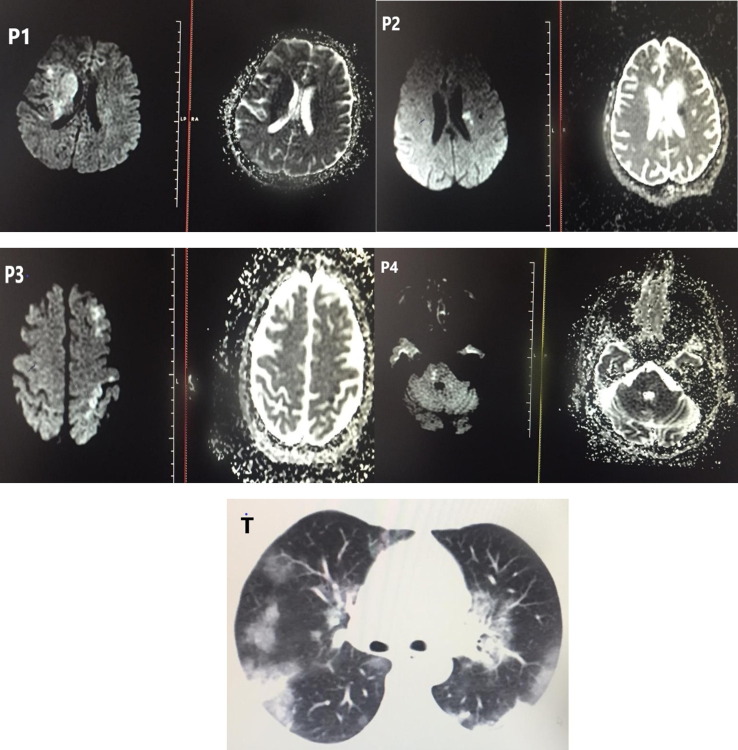
Case 1 is a 45-year-old woman, with no obvious vascular risk factors. She was admitted to emergency service with left facial paresis, dysarthria and left hemiparesis. She also reported high fever and cough with no known viral transmission history since 4 days. The National Institutes of Health Stroke Scale (NIHSS) score was 16. The diffusion magnetic resonance imaging (dMRI) of brain showed total left middle cerebral artery (MCA) infarction. Case 2 is a 67-year-old woman who suffered from dysarthria and right hemiparesis. The NIHSS score was 5. She had also intermittent fever and upper respiratory tract symptoms for 1 day. She was thought to be infected upon contact with her sick son. Brain dMRI showed left lenticulostriate artery infarction. Case 3 is a 72-year-old male with a history of hypertension. He was admitted with loss of consciousness, dysarthria, and right hemiparesis. The NIHSS score was 10. Although he had only mild cough, he had a viral transmission history 1 week before. The cortical branches of left MCA was affected in dMRI. Case 4 is a 77-year-old male admitting to emergency room with fever, cough and shortness of breath over the last two days. He had also left hemi-hypoesthesia and mild ataxia. The NIHSS score was 2. Brain dMRI showed right pontine infarction. Representative brain dMRI and chest CT images of COVID-19 patients are shown in Fig. 1 .
Fig. 1.
Representative brain dMRI and chest CT images of COVID-19 patients with acute stroke. (P1) Patient 1, right MCA infarction (P2) Patient 2, left lenticulostriate infarction (P3) Patient 3, left MCA cortical brances infarction (P4) Patient 4, right pontine infarction (T) Representative thorax CT image of the Patient 1.
Two of the cases had a high C-reactive protein (CRP) and three of them had high D-dimer levels. All of the patients with high D-dimer levels were diagnosed with anterior circulation infarction (see Table 1). Daily ECG follow ups did not reveal any arrhythmia.
3. Discussion
The present report describes a small case series of simultaneously diagnosed COVID-19 and acute ischemic cerebrovascular event. All the patients with stroke were elder, and had a history of hypertension with the exception of Case 1. None of the patients had severe SARS-CoV-2 infection, and 3 of them had elevated serum D-dimer levels, as well as two patients had high CRP levels.
In a recent study, 13 of 221 patients diagnosed with SARS-CoV-2 virus were reported to have ischemic stroke, as well as 1 cerebral venous sinus thrombosis and 1 cerebral bleeding [7]. The interesting aspect of our study was that stroke and infection appeared simultaneously. In the study of Li et al, the median durations from first symptoms of Covid-19 to cerebrovascular disease were 10 days [7]. The average of time from Covid-19 symptom onset to the diagnosis of stroke was 2 days in our cases. Of the patients with stroke, 2 were large vessel stenosis, 2 was small vessel occlusion. There was no cardioembolic type. Another interesting aspect of our study was that, unlike previous studies, none of the patients developed a severe Covid-19 infection [4], [7].
Inflammation has been increasingly accepted as a contributor to the thrombotic events [6]. Some blood inflammatory factors like CRP are thought to be responsible for early molecular events triggered by coagulation abnormalities [8]. In our study, 3 of the patients had elevated D-dimer levels, as well as two of them had high CRP levels. However, the clinical and radiological severity of Covid-19 infection in these patients were similar. There is a doubt regarding the increased inflammatory response underlying the abnormal blood coagulation in early stage of cerebrovascular diseases. It could also be speculated that Covid-19 patients were more prone to stroke, and the most accompanying comorbidity was hypertension. Our cases with anterior system infarction had higher D-dimer levels. Although our number of cases was limited, the severity of stroke offers an insight that it may vary depending on D-dimer levels.
COVID-19 is thought to have neuro-invasion potential as well as respiratory system involvement. As a result, cerebrovascular diseases such as ischemia and various central nervous system symptoms may develop independently of the critical disease process and increased inflammation predicted by CRP and D-dimer levels may play a role in the formation of ischemia. In particular, the elder Covid-19 patients with prothrombotic risk factors should also be considered for the signs of cerebrovascular events in addition to infectious symptoms.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patient included in the study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jocn.2020.05.018.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; NEJMoa2002032. doi:10.1056/NEJMoa2002032.
- 2.Johns Hopkins University & Medicine. COVID-19 map. Baltimore, MD: Johns Hopkins University; 2020. https://coronavirus.jhu.edu/map.html.
- 3.Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses. 2020;12(4):E372. Published 2020 Mar 27. doi:10.3390/v12040372. [DOI] [PMC free article] [PubMed]
- 4.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China [published online ahead of print, 2020 Apr 10]. JAMA Neurol. 2020;e201127. doi:10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed]
- 5.Moein ST, Hashemian SMR, Mansourafshar B, Khorram-Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID-19 [published online ahead of print, 2020 Apr 17]. Int Forum Allergy Rhinol. 2020; doi:10.1002/alr.22587. [DOI] [PMC free article] [PubMed]
- 6.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19 [published online ahead of print, 2020 Apr 10]. Thromb Res 2020; S0049-3848(20)30120-1. doi:10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed]
- 7.Li Y, Wang M, Zhou Y, Jiang C, Ying X, Ling M, et al. (2020). Acute Cerebrovascular Disease Following COVID-19: A Single Center, Retrospective, Observational Study. Lancet. 2020. In press. doi: 10.2139/ssrn.3550025. [DOI] [PMC free article] [PubMed]
- 8.Horvei L.D., Grimnes G., Hindberg K., Mathiesen E.B., Njølstad I., Wilsgaard T. C-reactive protein, obesity, and the risk of arterial and venous thrombosis. J Thromb Haemost. 2016;14(8):1561–1571. doi: 10.1111/jth.13369. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.