Abstract
The nasal cavity and turbinates play important physiological functions by filtering, warming and humidifying inhaled air. Paranasal sinuses continually produce nitric oxide (NO), a reactive oxygen species that diffuses to the bronchi and lungs to produce bronchodilatory and vasodilatory effects. Studies indicate that NO may also help to reduce respiratory tract infection by inactivating viruses and inhibiting their replication in epithelial cells. In view of the pandemic caused by the novel coronavirus (SARS-CoV-2), clinical trials have been designed to examine the effects of inhaled nitric oxide in COVID-19 subjects. We discuss here additional lifestyle factors such as mouth breathing which may affect the antiviral response against SARS-CoV-2 by bypassing the filtering effect of the nose and by decreasing NO levels in the airways. Simple devices that promote nasal breathing during sleep may help prevent the common cold, suggesting potential benefits against coronavirus infection. In the absence of effective treatments against COVID-19, the alternative strategies proposed here should be considered and studied in more detail.
Keywords: Innate immunity, Coronavirus, COVID-19, Nitric oxide, Breathing
The first cases of COVID-19 pneumonia caused by the novel coronavirus (SARS-CoV-2) were reported in Wuhan, China, in December 2019 [1,2]. Within a few months, SARS-CoV-2 had spread to most countries around the globe and is now responsible for more than 3,400,000 infections and 240,000 deaths, leading the World Health Organization to declare a worldwide pandemic crisis in March 2020. While early travel restrictions, quarantine measures, and face masks have helped to reduce the spread of the virus [3], new means to prevent and treat COVID-19 infections are urgently needed.
Inhalation of nitric oxide (NO) gas is currently being investigated as a preventive measure and treatment against COVID-19 (e.g., clinical trials NCT04306393, NCT04312243, NCT04338828, NCT04305457). Inhaled NO therapy has been used as rescue treatment to improve arterial oxygenation against acute respiratory distress syndrome (ARDS) [4], which represents a major complication of COVID-19. During the 2002–2003 severe acute respiratory syndrome (SARS) epidemic, also caused by a coronavirus, inhaled NO was tested in six SARS patients, producing beneficial effects that include decreased pulmonary hypertension, improved arterial oxygenation, and reduced spread and density of lung infiltrates [5]. Other possible options to increase NO levels in the human body include use of NO donor molecules (e.g., arginine, citrulline, nitroglycerin), phosphodiesterase inhibitors (e.g., Viagra) and consumption of nitrate-rich foods such as leafy green vegetables, beetroots and herbal spices [6,7], although the effects may be less targeted to the respiratory tract in these cases.
The rationale for using inhaled NO against SARS-CoV-2 infection stems from the fact that this molecule plays a major role in pulmonary and cardiovascular physiology. NO is a reactive oxygen species (ROS) that is continually produced by epithelial cells of the paranasal sinuses and nasopharynx via NO synthase (NOS) enzymes [8]. Produced at 10 parts per million (ppm) in the human sinuses, NO can diffuse to the bronchi and lungs, where it induces vasodilatory and bronchodilatory effects [[8], [9], [10]]. NO also activates ciliary movement [11] and mucus secretion [12], which can increase removal of dust and viral particles from the respiratory tract. Notably, NO produces antimicrobial effects against a broad range of microbes including bacteria, fungi, helminths, protozoa and viruses, which may help prevent pulmonary infections [13,14]. NO inactivates viruses by modifying proteins and nucleic acids that are essential for viral replication [14], and can reduce replication of viruses in vitro, including herpesvirus [15], rhinovirus [16], hantavirus [17], Coxsackie virus [18], Japanese encephalitis virus [19], retrovirus [20], vaccinia virus [21], and the SARS coronavirus [[22], [23], [24]]. NO also inhibits pulmonary viral replication in an experimental animal model in pigs [25]. In humans, higher basal levels of exhaled NO are associated with fewer symptoms of the common cold [26], suggesting that nasally-produced NO represents one of the body’s endogenous defense mechanisms against viruses in the airways.
Nonetheless, a study showed that inhaled NO at 80 or 160 ppm failed to improve survival or viral load in mice infected intranasally with a lethal dose of influenza virus [27]. Moreover, high levels of NO are produced by epithelial cells and leukocytes in subjects with acute viral infection and asthma, as seen by increased orally-exhaled NO levels under these conditions [28,29]. High exhaled NO levels are currently used as a marker for eosinophilic airway inflammation in asthmatic subjects [30], and some authors propose that NO may contribute to tissue damage during airway inflammation [14,31]. It thus remains to be seen whether increasing NO levels by inhalation or treatment with NO donors may produce antiviral effects in COVID-19 subjects. The possible effect of inhaled NO on bronchodilation and oxygenation appears promising, especially in view of the current shortage of ventilators.
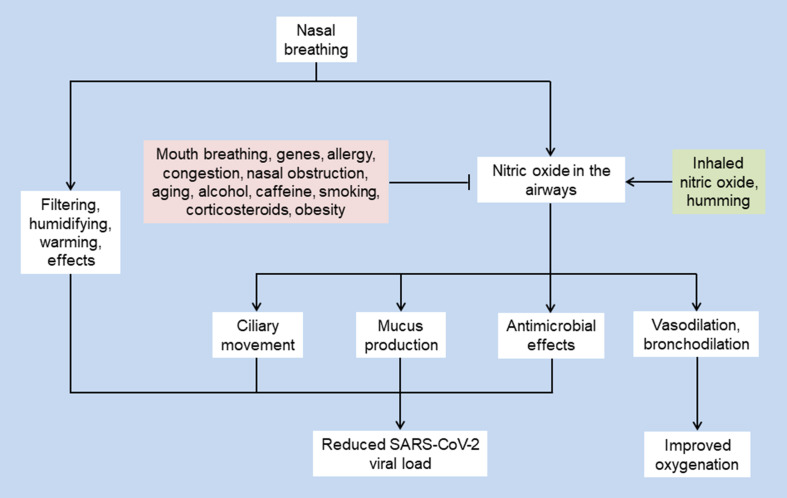
Conversely, low NO levels in the airways may facilitate SARS-CoV-2 infection and the development of COVID-19 in some individuals. Accordingly, conditions associated with reduced nasal NO production, including Kartagener’s syndrome [32] and cystic fibrosis [33], are associated with recurrent respiratory infections and inflammation. Similarly, mice that are deficient in NOS or that are treated with NOS inhibitors are also susceptible to viral infections [34,35]. In the general population, orally-exhaled and nasal NO levels are reduced in white people (compared to Asians) and in individuals who smoke or consume alcohol, caffeine, or corticosteroids [[36], [37], [38]] (Fig. 1 ).
Fig. 1.
Potential effects of nasal breathing and nitric oxide on SARS-CoV-2 viral load and oxygenation. Nasal breathing may reduce viral load and improve oxygenation in COVID-19 subjects by filtering the air and by increasing NO levels in the airways. Several factors may reduce or increase the levels of nitric oxide as shown in the pink and green rectangles, respectively.
Another phenomenon that reduces NO levels in the airways—as well as the filtering, warming and humidifying effects of the nose on inhaled air—is mouth breathing. Measurements indicate that mouth breathers have lower levels of NO within the respiratory tract compared to nasal breathers [39]. Mouth breathing has been associated with many health issues, including abnormal facial and dental development, cardiovascular disease, fatigue, halitosis, headaches, hypertension, inflammation, sleep apnea, snoring, stress, and tooth decay, to name a few [[40], [41], [42], [43]]. While most people spontaneously report breathing through the nose, mouth breathing may occur during talking, exercise and sleep or in people with allergies, congestion or nasal obstruction, suggesting that it may be more prevalent than usually appreciated. For instance, switching between nasal and mouth breathing is common during sleep, especially in older individuals [44]. Studies indicate that individuals who snore or breathe through the mouth during sleep—conditions which are highly prevalent in males—are more likely to develop respiratory tract infections [45]. Our anecdotal observations also suggest that favoring nasal breathing during sleep by sealing the mouth with adhesive tape reduces common colds. This phenomenon may be due to the filtration and humidifying effects of the nose on inhaled air and to increased NO levels in the airways, which may decrease viral load during sleep and allow the immune system more time to mount an effective antiviral response. Conversely, following viral infection of airway epithelial cells, constant or intermittent mouth breathing in daytime and during sleep may reduce the beneficial effects of the nose and NO against the virus, therefore leading to unobstructed viral replication (Fig. 1). Mouth breathing during sleep may therefore worsen the symptoms of COVID-19, consistent with the observation that symptoms of respiratory infections are usually worse in the morning.
The studies described here suggest that therapies designed to increase airway NO levels via gas inhalation and donor molecules may improve oxygenation and produce health benefits in COVID-19 subjects. In addition, limiting the lifestyle factors that reduce endogenous NO levels in the airways—such as mouth breathing and smoking—may also help to reduce SARS-CoV-2 viral load and symptoms of COVID-19 pneumonia by promoting more efficient antiviral defense mechanisms in the respiratory tract. In the absence of effective treatments targeting SARS-CoV-2, we believe that these strategies should be considered and tested to mitigate the symptoms of COVID-19. Finally, the overall severity of disease would also be decreased by combining nasal breathing with a healthy lifestyle that includes exercise, a full night’s sleep, and a balanced diet.
Declaration of Competing Interest
Y.-F.K. is President of Chang Gung Biotechnology Corporation. J.D.Y. is Chairman of the Board of Chang Gung Biotechnology Corporation. D.M.O. is an editor with Microbes and Infection. The other author (J.M.) declares that no competing interests.
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pan X., Ojcius D.M., Gao T., Li Z., Pan C. Lessons learned from the 2019-nCoV epidemic on prevention of future infectious diseases. Microb Infect. 2020;22:86–91. doi: 10.1016/j.micinf.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teman N.R., Thomas J., Bryner B.S., Haas C.F., Haft J.W., Park P.K. Inhaled nitric oxide to improve oxygenation for safe critical care transport of adults with severe hypoxemia. Am J Crit Care. 2015;24:110–117. doi: 10.4037/ajcc2015570. [DOI] [PubMed] [Google Scholar]
- 5.Chen L., Liu P., Gao H., Sun B., Chao D., Wang F. Inhalation of nitric oxide in the treatment of severe acute respiratory syndrome: a rescue trial in Beijing. Clin Infect Dis. 2004;39:1531–1535. doi: 10.1086/425357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lundberg J.O., Weitzberg E., Gladwin M.T. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov. 2008;7:156–167. doi: 10.1038/nrd2466. [DOI] [PubMed] [Google Scholar]
- 7.Lundberg J.O., Carlstrom M., Weitzberg E. Metabolic effects of dietary nitrate in health and disease. Cell Metabol. 2018;28:9–22. doi: 10.1016/j.cmet.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Lundberg J.O., Farkas-Szallasi T., Weitzberg E., Rinder J., Lidholm J., Anggaard A. High nitric oxide production in human paranasal sinuses. Nat Med. 1995;1:370–373. doi: 10.1038/nm0495-370. [DOI] [PubMed] [Google Scholar]
- 9.Lundberg J.O., Weitzberg E. Nasal nitric oxide in man. Thorax. 1999;54:947–952. doi: 10.1136/thx.54.10.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lundberg J.O. Nitric oxide and the paranasal sinuses. Anat Rec. 2008;291:1479–1484. doi: 10.1002/ar.20782. [DOI] [PubMed] [Google Scholar]
- 11.Runer T., Cervin A., Lindberg S., Uddman R. Nitric oxide is a regulator of mucociliary activity in the upper respiratory tract. Otolaryngol Head Neck Surg. 1998;119:278–287. doi: 10.1016/S0194-5998(98)70063-4. [DOI] [PubMed] [Google Scholar]
- 12.Nagaki M., Shimura M.N., Irokawa T., Sasaki T., Shirato K. Nitric oxide regulation of glycoconjugate secretion from feline and human airways in vitro. Respir Physiol. 1995;102:89–95. doi: 10.1016/0034-5687(95)00042-c. [DOI] [PubMed] [Google Scholar]
- 13.Nathan C., Xie Q.W. Nitric oxide synthases: roles, tolls, and controls. Cell. 1994;78:915–918. doi: 10.1016/0092-8674(94)90266-6. [DOI] [PubMed] [Google Scholar]
- 14.Xu W., Zheng S., Dweik R.A., Erzurum S.C. Role of epithelial nitric oxide in airway viral infection. Free Radic Biol Med. 2006;41:19–28. doi: 10.1016/j.freeradbiomed.2006.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Croen K.D. Evidence for antiviral effect of nitric oxide. Inhibition of herpes simplex virus type 1 replication. J Clin Invest. 1993;91:2446–2452. doi: 10.1172/JCI116479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaul P., Singh I., Turner R.B. Effect of nitric oxide on rhinovirus replication and virus-induced interleukin-8 elaboration. Am J Respir Crit Care Med. 1999;159:1193–1198. doi: 10.1164/ajrccm.159.4.9808043. [DOI] [PubMed] [Google Scholar]
- 17.Klingstrom J., Akerstrom S., Hardestam J., Stoltz M., Simon M., Falk K.I. Nitric oxide and peroxynitrite have different antiviral effects against hantavirus replication and free mature virions. Eur J Immunol. 2006;36:2649–2657. doi: 10.1002/eji.200535587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saura M., Zaragoza C., McMillan A., Quick R.A., Hohenadl C., Lowenstein J.M. An antiviral mechanism of nitric oxide: inhibition of a viral protease. Immunity. 1999;10:21–28. doi: 10.1016/S1074-7613(00)80003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin Y.L., Huang Y.L., Ma S.H., Yeh C.T., Chiou S.Y., Chen L.K. Inhibition of Japanese encephalitis virus infection by nitric oxide: antiviral effect of nitric oxide on RNA virus replication. J Virol. 1997;71:5227–5235. doi: 10.1128/jvi.71.7.5227-5235.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akarid K., Sinet M., Desforges B., Gougerot-Pocidalo M.A. Inhibitory effect of nitric oxide on the replication of a murine retrovirus in vitro and in vivo. J Virol. 1995;69:7001–7005. doi: 10.1128/jvi.69.11.7001-7005.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris N., Buller R.M., Karupiah G. Gamma interferon-induced, nitric oxide-mediated inhibition of vaccinia virus replication. J Virol. 1995;69:910–915. doi: 10.1128/jvi.69.2.910-915.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keyaerts E., Vijgen L., Chen L., Maes P., Hedenstierna G., Van Ranst M. Inhibition of SARS-coronavirus infection in vitro by S-nitroso-N-acetylpenicillamine, a nitric oxide donor compound. Int J Infect Dis. 2004;8:223–226. doi: 10.1016/j.ijid.2004.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akerstrom S., Mousavi-Jazi M., Klingstrom J., Leijon M., Lundkvist A., Mirazimi A. Nitric oxide inhibits the replication cycle of severe acute respiratory syndrome coronavirus. J Virol. 2005;79:1966–1969. doi: 10.1128/JVI.79.3.1966-1969.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akerstrom S., Gunalan V., Keng C.T., Tan Y.J., Mirazimi A. Dual effect of nitric oxide on SARS-CoV replication: viral RNA production and palmitoylation of the S protein are affected. Virology. 2009;395:1–9. doi: 10.1016/j.virol.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jung K., Gurnani A., Renukaradhya G.J., Saif L.J. Nitric oxide is elicited and inhibits viral replication in pigs infected with porcine respiratory coronavirus but not porcine reproductive and respiratory syndrome virus. Vet Immunol Immunopathol. 2010;136:335–339. doi: 10.1016/j.vetimm.2010.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ritz T., Trueba A.F., Vogel P.D., Auchus R.J., Rosenfield D. Exhaled nitric oxide and vascular endothelial growth factor as predictors of cold symptoms after stress. Biol Psychol. 2018;132:116–124. doi: 10.1016/j.biopsycho.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 27.Darwish I., Miller C., Kain K.C., Liles W.C. Inhaled nitric oxide therapy fails to improve outcome in experimental severe influenza. Int J Med Sci. 2012;9:157–162. doi: 10.7150/ijms.3880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kharitonov S.A., Yates D., Barnes P.J. Increased nitric oxide in exhaled air of normal human subjects with upper respiratory tract infections. Eur Respir J. 1995;8:295–297. doi: 10.1183/09031936.95.08020295. [DOI] [PubMed] [Google Scholar]
- 29.Kharitonov S.A., Chung K.F., Evans D., O’Connor B.J., Barnes P.J. Increased exhaled nitric oxide in asthma is mainly derived from the lower respiratory tract. Am J Respir Crit Care Med. 1996;153:1773–1780. doi: 10.1164/ajrccm.153.6.8665033. [DOI] [PubMed] [Google Scholar]
- 30.Taylor D.R., Pijnenburg M.W., Smith A.D., De Jongste J.C. Exhaled nitric oxide measurements: clinical application and interpretation. Thorax. 2006;61:817–827. doi: 10.1136/thx.2005.056093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akaike T., Maeda H. Nitric oxide and virus infection. Immunology. 2000;101:300–308. doi: 10.1046/j.1365-2567.2000.00142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lundberg J.O., Weitzberg E., Nordvall S.L., Kuylenstierna R., Lundberg J.M., Alving K. Primarily nasal origin of exhaled nitric oxide and absence in Kartagener’s syndrome. Eur Respir J. 1994;7:1501–1504. doi: 10.1183/09031936.94.07081501. [DOI] [PubMed] [Google Scholar]
- 33.Lundberg J.O., Nordvall S.L., Weitzberg E., Kollberg H., Alving K. Exhaled nitric oxide in paediatric asthma and cystic fibrosis. Arch Dis Child. 1996;75:323–326. doi: 10.1136/adc.75.4.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karupiah G., Xie Q.W., Buller R.M., Nathan C., Duarte C., MacMicking J.D. Inhibition of viral replication by interferon-gamma-induced nitric oxide synthase. Science. 1993;261:1445–1448. doi: 10.1126/science.7690156. [DOI] [PubMed] [Google Scholar]
- 35.Noda S., Tanaka K., Sawamura S., Sasaki M., Matsumoto T., Mikami K. Role of nitric oxide synthase type 2 in acute infection with murine cytomegalovirus. J Immunol. 2001;166:3533–3541. doi: 10.4049/jimmunol.166.5.3533. [DOI] [PubMed] [Google Scholar]
- 36.Lundberg J.O., Weitzberg E., Lundberg J.M., Alving K. Nitric oxide in exhaled air. Eur Respir J. 1996;9:2671–2680. doi: 10.1183/09031936.96.09122671. [DOI] [PubMed] [Google Scholar]
- 37.Yates D.H. Role of exhaled nitric oxide in asthma. Immunol Cell Biol. 2001;79:178–190. doi: 10.1046/j.1440-1711.2001.00990.x. [DOI] [PubMed] [Google Scholar]
- 38.Kovesi T., Kulka R., Dales R. Exhaled nitric oxide concentration is affected by age, height, and race in healthy 9- to 12-year-old children. Chest. 2008;133:169–175. doi: 10.1378/chest.07-1177. [DOI] [PubMed] [Google Scholar]
- 39.Tornberg D.C., Marteus H., Schedin U., Alving K., Lundberg J.O., Weitzberg E. Nasal and oral contribution to inhaled and exhaled nitric oxide: a study in tracheotomized patients. Eur Respir J. 2002;19:859–864. doi: 10.1183/09031936.02.00273502. [DOI] [PubMed] [Google Scholar]
- 40.Lavie P. Rediscovering the importance of nasal breathing in sleep or, shut your mouth and save your sleep. J Laryngol Otol. 1987;101:558–563. doi: 10.1017/s0022215100102245. [DOI] [PubMed] [Google Scholar]
- 41.Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics, and behavior. Gen Dent. 2010;58:18–25. [PubMed] [Google Scholar]
- 42.Padzys G.S., Thornton S.N., Martrette J.M., Trabalon M. Effects of short term forced oral breathing in rat pups on weight gain, hydration and stress. Physiol Behav. 2011;102:175–180. doi: 10.1016/j.physbeh.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 43.Trabalon M., Schaal B. It takes a mouth to eat and a nose to breathe: abnormal oral respiration affects neonates’ oral competence and systemic adaptation. Int J Pediatr. 2012;2012:207605. doi: 10.1155/2012/207605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Madronio M.R., Di Somma E., Stavrinou R., Kirkness J.P., Goldfinch E., Wheatley J.R. Older individuals have increased oro-nasal breathing during sleep. Eur Respir J. 2004;24:71–77. doi: 10.1183/09031936.04.00004303. [DOI] [PubMed] [Google Scholar]
- 45.Kukwa W., Guilleminault C., Tomaszewska M., Kukwa A., Krzeski A., Migacz E. Prevalence of upper respiratory tract infections in habitually snoring and mouth breathing children. Int J Pediatr Otorhinolaryngol. 2018;107:37–41. doi: 10.1016/j.ijporl.2018.01.022. [DOI] [PubMed] [Google Scholar]