To the Editor:
PROVIDING ADEQUATE care to the large number of patients critically ill with coronavirus disease 2019 (COVID-19) with severe acute respiratory distress syndrome (ARDS) is a resource-intensive task. Reducing duration of mechanical ventilation may assist in decompressing intensive care units (ICUs). Standard of care in managing ARDS includes lung-protective ventilation and appropriate diuresis.1 , 2 Recent literature regarding using portable ultrasonography at the bedside (point-of-care ultrasound or POCUS) on critically ill patients suggested current use in modern ICUs.3 We propose that a focused lung and heart ultrasound may help follow progression of pneumonia and pulmonary edema and characterize volume status.
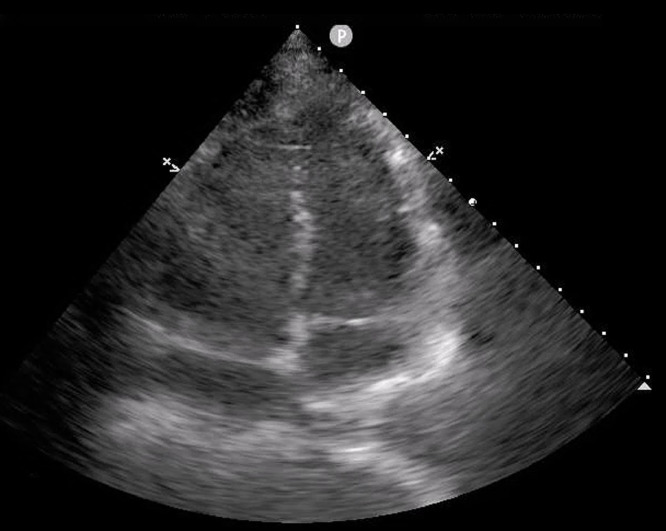
As anesthesiologists are being tasked to provide critical care, it is necessary to take the lessons of judicious fluid use from our operating rooms to the ICUs. Indeed, daily weights and fluid balance help guide diuretic and fluid therapy. However, the inflammatory state in COVID-19 patients may contribute to vascular permeability and intravascular depletion despite increased total body water. Periodic vasoplegia, high positive end-expiratory pressure, and cardiac dysfunction also confuse typical hemodynamic estimations of total body water such as blood pressure and central venous pressure.4 Using an apical 4-chamber view and a parasternal short-axis view, we can obtain a quick estimation of left and right ventricular function and fluid status (Fig 1 ). These findings could then be interpreted in the context of hemodynamics and fluid balance to guide treatment.
Fig 1.
Apical 4-chamber view demonstrating an enlarged right ventricle consistent with elevated intravascular volume.
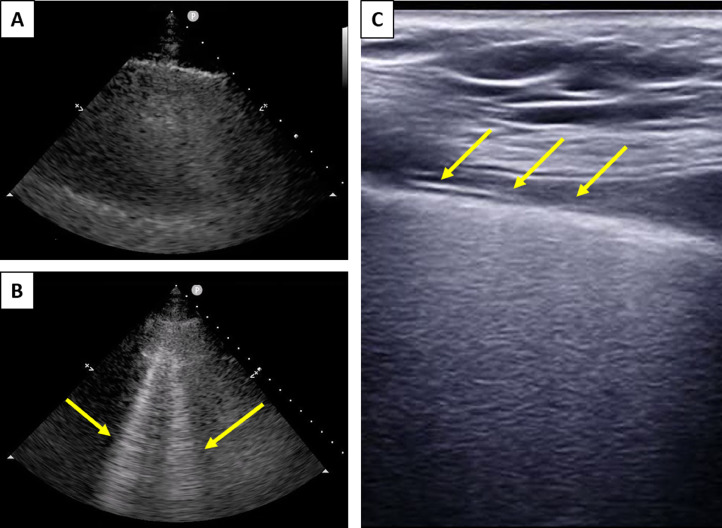
Lung ultrasound can help characterize normal and abnormal lung regions. In addition to ventilatory settings, partial pressure of oxygen, and pulse oximetry, a scoring of diseased- to- normal lung regions may add to patient assessment. Placing patients with severe ARDS in the prone position is used as high settings or limits of mechanical ventilation are reached.5 Posterior lung ultrasound, if identifying significant areas of normal lung parenchyma, may identify patients in whom early proning may reduce precipitous increases in ventilator settings, escalation of vasopressors, and need for neuromuscular paralysis. We depict a COVID-19 patient pre- and post-proning demonstrating improved lung aeration and reduced consolidation (Fig 2 ).
Fig 2.
(A) Lung ultrasound demonstrates area of consolidation prior to placing the patient in the prone position. Consolidation in a nonaerated lung, which results in a significant shunt. (B) Lung ultrasound after placing the patient in the prone position demonstrates significant “B lines” (arrows) consistent with acute respiratory distress syndrome, however, with improved aeration. Clinically, the patient's oxygenation improved as well after proning. (C) Linear probe demonstrates a thickened pleural line (arrows).
In a time when there is an increase in telemedicine, limited physical examinations, and limited provider-patient direct contact, it is difficult to recommend the use of personnel and personal protective equipment to perform specialized and technical tasks. However, the potential benefit of possible reduced end-stage lung failure, reduced ventilator days, and reduced critical care resource use needs to be carefully weighed. As noncritical care–trained physicians are called to provide critical care, the utility of a curriculum of very focused POCUS may also assist in patient management.
Conflict of Interest
No conflicts of interest for any authors reported.
Footnotes
No external sources of funding were provided for this study.
References
- 1.Acute Respiratory Distress Syndrome Network. Brower R.G., Matthay M.A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 2.National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Wiedemann H.P., Wheeler A.P. Comparison of 2 fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 3.Sanjan A., Krishnan S.V., Abraham S.V. Utility of point-of-care lung ultrasound for initial assessment of acute respiratory distress syndrome patients in the emergency department. J Emerg Trauma Shock. 2019;12:248–253. doi: 10.4103/JETS.JETS_47_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guérin C., Reignier J., Richard J.C. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]