Introduction
Neurofibromatosis type 1 (NF1) is an autosomal dominant multisystem genodermatosis resulting from a mutation on chromosome 17q11.2, characterized by diverse clinical expression with involvement of the skin, nervous system, bones, eyes, and other systems. Café-au-Lait spots, axillary freckles, and neurofibromas are the main cutaneous manifestations. Neurofibromas are tumors located along nerve bundles; when they become large, they are called plexiform neurofibromas.1 They often lack function and aesthetic value, thereby negatively affecting quality of life.2
There is no specific treatment for NF1, and clinical manifestations are treated individually. Surgery is the preferred treatment for plexiform neurofibromas, but the significant vascularization of the tumor and the consequent possibility of large intraoperative hemorrhages make the procedure difficult.3 Thus, preoperative embolization becomes useful to reduce potential surgical complications.
Case report
We report the case of a 34-year-old woman with NF1 with a large plexiform neurofibroma (39.5 × 20 × 15.7 cm) on the right flank, impairing appearance and mobility (Fig 1).
Fig 1.

Plexiform neurofibroma.
High-frequency ultrasound scan (24 MHz) with Doppler flowmetry found a hyperechoic solid mass with irregular borders with multiple hypoechogenic nodules and permeating large-caliber vascular pedicles. Because of the intense vascularization, angiotomography of the abdomen and pelvis was performed to characterize the arterial supply, and vascularization with multiple intercostal, lumbar, iliac, and gluteal branches was observed.
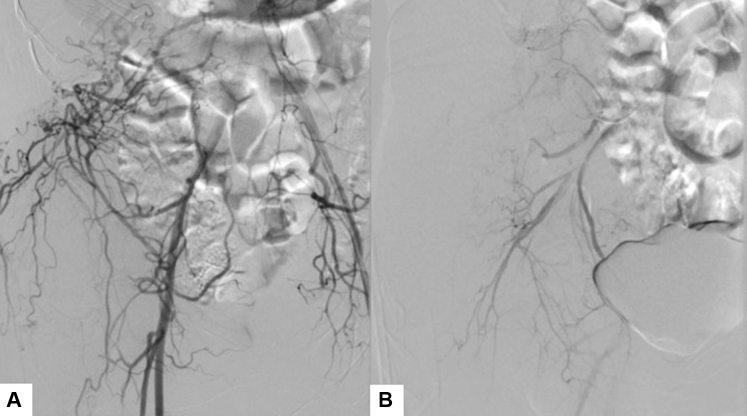
According to the clinical-radiologic findings, a 2-stage approach was planned: first, embolization with polyvinyl alcohol particles of the inferior epigastric, lumbar, and superior gluteal arteries on the right (Fig 2) and, second, 24 hours after embolization, excision of the lesion, which weighed 2.5 kg (Fig 3).
Fig 2.
Embolization. Arteriography performed before (A) and after (B) the embolization, shows devascularization of the embolized territory with preservation of the other nontarget arterial branches.
Fig 3.

Plexiform neurofibroma. Lesion weighing 2.5 kg.
Histopathologic examination and immunohistochemistry confirmed a nonmalignant neurogenic tumor with degenerative atypia, confirming the diagnosis of neurofibroma. Intraoperative blood loss was moderate, but the hemoglobin decrease from 14.2 g/dL to 8 g/dL on the day after the procedure required transfusion of 2 packed red blood cell units.
The patient was treated using a multidisciplinary team that included individuals from the dermatology, plastic surgery, and interventional radiology departments. Two years after surgery, the patient was asymptomatic, without tumor recurrence, and with an important improvement in self-esteem and quality of life (Fig 4).
Fig 4.
Plexiform neurofibroma. Patient before (A) and 2 years after (B) the treatment with surgery and embolization.
Discussion
Plexiform neurofibromas have variable clinical presentations, ranging from asymptomatic to invasive and disfiguring superficial lesions. In some cases, transformation to malignant tumors is observed. Surgical intervention is important for histopathologic diagnosis as well as for therapeutics, restoring appearance and function.3
The intense vascularization and characteristic capillary fragility of the disease predisposes patients to a high risk of potentially fatal intraoperative hemorrhages. Therefore, preoperative embolization can be performed in an attempt to devascularize the embolized area, reduce intraoperative bleeding and, consequently, achieve rapid hemostasis.4
There is no evidence regarding the size of the neurofibroma to be treated by embolization before surgical removal. Preoperative angiography and angiotomography should be performed to clarify the tumor vascular features. Except in the presence of contraindications to the procedure, plexiform neurofibromas with a plethora of abnormal vessels forming an integral part of the lesion are benefited by preoperative embolization.5
In the reports of 9 cases of preoperative embolization followed by surgery in patients aged 15 to 55 years, 5 men and 4 women had plexiform neurofibromas, mainly located in the trunk.3, 4, 5, 6, 7, 8, 9, 10
To minimize complications, it is important to properly select the material that will be used for embolization based on safety, efficacy, polymerization properties, and ease of use.4 Different embolization techniques were used by the authors: lyophilized dura mater strips, fascia lata strips, gelatine sponge, microsprings and an ethylene-vinyl alcohol copolymer. In the current case, polyvinyl alcohol was chosen as the embolizable particle, also used by Cavallaro et al6 and Vélez et al7 and was found to be safe and effective.
There is no consensus on the ideal interval between embolization and surgical resection. Littlewood and Stilwell5 embolized a plexiform neurofibroma 3 weeks before surgery, with significant blood loss and the need for transfusion of 11 units of packed red blood cells. In our case, we performed selective embolization followed by surgery after 24 hours. This approach is important for reduction of flow in the vascular pedicles at the level of dissection and lowering the risk of adjacent tissue necrosis.
Resection of plexiform neurofibromas is a difficult procedure because of the rich vascular proliferation, infiltration of deep planes, and reconstruction of large areas. Therefore, adequate preoperative planning using new technologies combined with a multidisciplinary approach is important for achieving satisfactory results through functional restoration and improved appearance.
Footnotes
Funding sources: Sírio-Libanês Teaching and Research Institute.
Conflicts of interest: None disclosed.
References
- 1.Antônio J.R., Goloni-Bertollo E.M., Trídico L.A. Neurofibromatose: histórico cronológico e aspectos atuais. An Bras Dermatol. 2013;88:333–347. doi: 10.1590/abd1806-4841.20132125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen L., Guo C., Song X. Long-Term results for a one-stage surgery technique for patients with craniofacial plexiform neurofibroma. J Craniofac Surg. 2018;29:e746–e750. doi: 10.1097/SCS.0000000000004685. [DOI] [PubMed] [Google Scholar]
- 3.Kolker S., Wunder J.S., Roche-Nagle G. Hybrid resection of a giant thigh plexiform neurofibroma. Int J Surg Case Rep. 2015;8:1–4. doi: 10.1016/j.ijscr.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomei K.L., Gupta V., Prestigiacomo C.J. Spontaneous hemorrhage of a facial neurofibroma: endovascular embolization before surgical intervention. J Craniofac Surg. 2013;24:e514–e517. doi: 10.1097/SCS.0b013e3182a23535. [DOI] [PubMed] [Google Scholar]
- 5.Littlewood A.H.M., Stilwell J.H. The vascular features of plexiform neurofibroma with some observations on the importance of pre-operative angiography and the value of pre-operative intra-arterial embolization. Br J Plast Surg. 1983;36:501–506. doi: 10.1016/0007-1226(83)90140-6. [DOI] [PubMed] [Google Scholar]
- 6.Cavallaro G., Pedullà G., Crocetti D. Vacuum-assisted closure treatment of leg skin necrosis after angiographic embolization of a giant plexiform neurofibroma. G Chir. 2012;33:239–242. [PubMed] [Google Scholar]
- 7.Vélez R., Barrera-Ochoa S., Barastegui D. Multidisciplinary management of a giant plexiform neurofibroma by double sequential preoperative embolization and surgical resection. Case Reps Neurol Med. 2013;2013:987623. doi: 10.1155/2013/987623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones R.G., Kiatisevi P., Morris D.C. Intravascular embolisation and surgical resection of a giant neurofibroma with intratumoural haemorrhage. Br J Radiol. 2010;83:e225–e229. doi: 10.1259/bjr/42783229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanaka J., Kuramochi A., Nishi N. Preoperative transarterial embolization enhances the surgical management of diffuse plexiform neurofibroma: a case report. Cardiovasc Intervent Radiol. 2005;28:686–688. doi: 10.1007/s00270-004-0230-2. [DOI] [PubMed] [Google Scholar]
- 10.D'Arpa S., Tuttolomondo A., Melloni C. Management of large dorsal diffuse plexiform neurofibroma. Eur J Plast Surg. 2014;37:349–352. [Google Scholar]