Abstract
Background
Injuries to the acromioclavicular (AC) joint disrupting the AC and Coracoclavicular (CC) ligaments could lead to loss of clavicular strut function. A High-grade AC joint injury remain challenging because of highly variety of treatment and limited evidence exists comparing clinical outcomes and complications after surgery.
Purpose
The purpose of this study was to compare the clinical and radiological outcome after arthroscopic assisted acromioclavicular Joint fixation and anatomic acromioclavicular joint reconstruction.
Study design
Retrospective Clinical Cohort Study.
Methods
Twenty-nine patients with a high grade (Rockwood Type III-V) Acromioclavicular Joint Injury, operatively treated with arthroscopic assisted acromioclavicular joint fixation and anatomic acromioclavicular joint reconstruction from 2012 to 2018. The clinical assessment consists of Specific AC Score (SACS) and Nottingham Score. The radiographic evaluations were performed to evaluate the stability of reduction and the complications are assessed.
Results
There were a significant different between groups with AC joint reconstruction and fixation group (20 vs. 8, p < 0.005) and (19 vs. 10, p < 0.005) in SAC score and Nottingham score, respectively. There were no significant different in CC dstance between two groups. At the last follow up 6 patient develop loss of reduction with CC percentage >50% in AC joint fixation. Complication developed in 5 patients (17%) including 2 mild osteolysis, 1 superficial infection, 1 implant failure, and 1 clavicle fracture.
Conclusion
Anatomic AC joint reconstruction was associated with functional and radiologic benefits and better restored the stability.
Keywords: Acromioclavicular joint injury, AC joint Fixation, AC joint Reconstruction
1. Introduction
Injuries to the AC joint are common, comprising approximately 12% of shoulder injuries.1(2) More common in men in their third decade of life, during high-speed biking and motorcross, or sports related.3 The mechanism of injury is typically direct force to the acromion with the shoulder adducted or indirect force from falling of an outstretched arm.4
The Rockwood classification takes into account the clavicular attachment of the deltoid and trapezius muscles, and the direction of dislocation of the clavicle. Recommendations for management of these injuries are typically nonsurgical for types 1 and 2, surgical for types 4 through 6. Controversial for type 3,5 but tending to surgery in younger or functional high demand patients.
Acromioclavicular (AC) joint stability depends on contributions from both the coracoclavicular (CC) ligaments and the AC capsular structure. The capsuloligamentous of AC joint not only control horizontal and vertical translation of the distal clavicle but also controll rotation. AC capsule contribute to the resistance against horizontal and rotational stresses. By controlled rotation of more than 40°–50° for the acromion in relation to the lateral clavicle while simultaneously preserving a centered motion.6
No consensus is available regarding the best practices for diagnosis, evaluation, or treatment of acute or chronic of the AC joint. Chronic ACJ instability may be associated with periscapular muscle fatigue, scapular dyskinesia, dead-arm syndrome, and painful horizontal adduction. A recent study suggest that there are no significant differences between acute and chronic repair of AC joint dislocations if all other aspects of treatment are similar.7
There are more than 160 acromioclavicular joint stabilizing techniques are described including both open and arthroscopic techniques, anatomic and non-anatomic procedure.2 Postoperative complication rates have been reported to be greater than 20%. Radiographic loss of reduction has also been reported in as high as over 30% of cases.8 Surgical treatment is based on CC fixation and/or ligament reconstruction and combined stabilization of the AC capsule and CC ligaments demonstrated the greatest capacity to restore native stability against translational and rotational loads.1 Synthetic fixation provided equivalent loss of reduction in comparison with all other reconstruction techniques.2 Biological fixation using tendon graft better to promote biological tissue healing to maintain vertical and horizontal stability.9
The purpose of this study was to evaluate the clinical and radiologic outcome of the high grade AC joint injury in patients were treated with both anatomic reconstruction of all AC and CC ligaments and AC joint fixation. The hypothesis was anatomic AC joint reconstruction leads to better clinical and radiological result.
2. Material and methods
2.1. Patient selection
This is a retrospective clinical cohort study to reassess patients that were diagnosed and treated at our institution between January 2012 until December 2018. The inclusion criteria were1 Rockwood grade III, IV, V AC separation,2 no previous acromioclavicular injury,3 operative treatment arthroscopic assisted AC joint fixation or anatomic AC joint reconstruction4 no preoperative osteoarthritic change,5 no prior shoulder surgery. The exclusion criteria were1 patients with minimal or moderate ACJ displacement (Rockwood type I or II),2 neurological disease that affect shoulder function,3 patient with fractures of distal clavicle. In 2016, our surgical approach for grade III, IV, V AC joint separation has change from fixation to reconstruction. Of the 29 patients selected, 14 were operated in using AC joint fixation and 15 with AC joint reconstruction. The diagnoses were confirmed with preoperative radiographs. This study were retrospectively reviewed and the following demographic information any concomitant injuries were documented.
2.2. Surgical technique
All surgery done by a single senior author. If associated intra-articular lesions were found, they were treated arthroscopically at that time.
2.2.1. Arthroscopy assisted acromioclavicular joint fixation
The beach chair position is used for acromioclavicular (AC) reconstruction surgery. Kim's portal is used for visualization. Diagnostic arthroscopy is performed to check for any associated pathology. An anterior portal is made just inferolateral to the tip of the coracoid (Fig. 1). The bony undersurface of the coracoid is exposed and roughened (Fig. 2).
Fig. 1.
Kim's portal is used for visualization, an anterior portal is made just inferolateral to the tip of the coracoid.
Fig. 2.
Arthroscopic view from Kim's portal. Exposed and roughened the coracoid.
The arthroscope is removed, and an approximately 4- to 5-cm skin incision close to the anterior border of the clavicle extending laterally 1 cm beyond the AC joint is made. No. 5 ethibond is then passed under the coracoid from the medial side close to the bone. The arthroscope is inserted again, the suture is retrieved lateral to the coracoid process under direct visualization. A suture loop is thus placed under the coracoid process. Using a #2 PDS suture as a shuttle relay, Fibersuture was passed under coracoid (Fig. 3).
Fig. 3.
After AC joint is exposed, the arthroscope is inserted again and fibersuture is placed under the coracoid.
Both limb of the suture are held vertically parallel to each other, and two points are marked on the clavicle. Two tunnels in the clavicle process are then drilled. Acromioclavicular joint was overreduced and temporary fixation using Kirschner wire (Fig. 4), and the suture was tightened over the titanium plate or endobutton(Fig. 5).
Fig. 4.
AC joint is placed in over reduced position, and temporary fixation using Kirschner wire.
Fig. 5.
The four free ends of the suture were passed through the endobutton hole. and the suture was tightened over the titanium plate or endobutton.
2.2.2. Arthroscopic assisted acromioclavicular joint reconstruction using Hamstring graft (20)
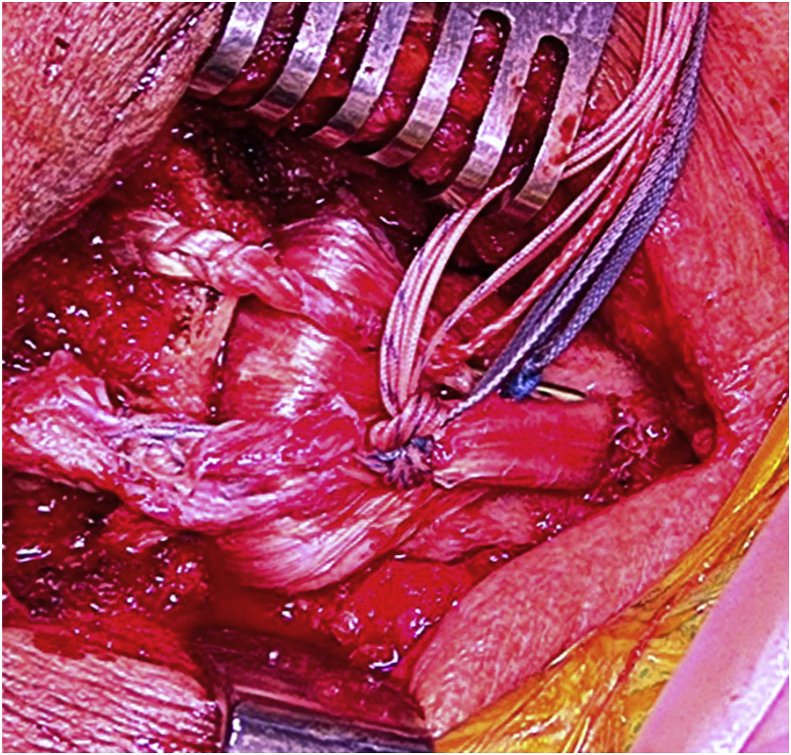
The beach chair position is used for acromioclavicular (AC) reconstruction surgery. Kim's portal is used for visualization. Diagnostic arthroscopy is performed to check for any associated pathology. An anterior portal is made to reach the base of the coracoid. The bony undersurface of the coracoid is exposed and roughened for graft healing. The arthroscope is removed, and an approximately 4- to 5-cm skin incision. A suture loop is thus placed under the coracoid process. Then, the semitendinosus-gracilis autograft is pulled under the coracoid process (Fig. 6).
Fig. 6.
Arthroscopic view from Kim's portal demonstrate semitendinosus-gracilis autograft under the coracoid process.
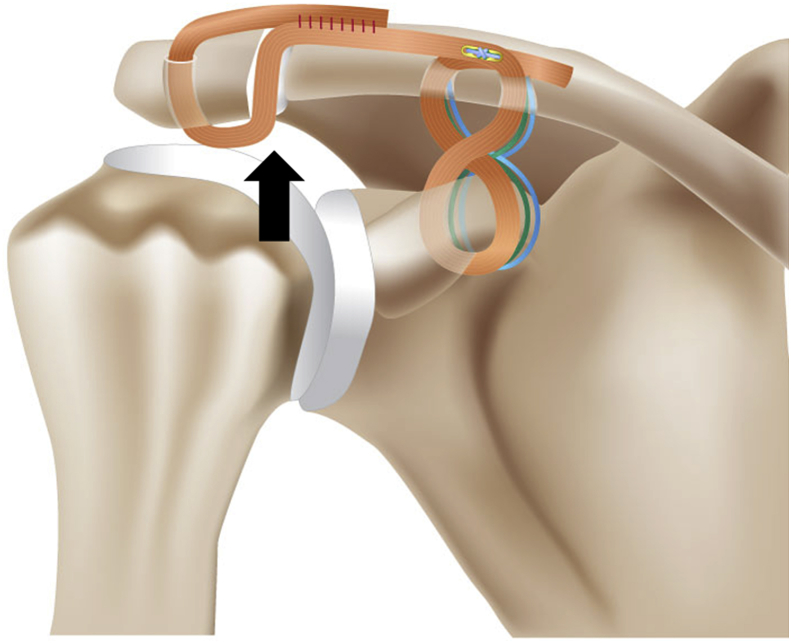
Both limbs of the graft are held vertically parallel to each other, which will be approximately at the same distance as the width of the coracoid process base. This more individualized approach is preferable, as a fixed distance may not consistently restore anatomy, since bone dimensions differ with each patient. Two tunnels in the clavicle (Fig. 7) and two in the acromion process are then drilled at a diameter that matches the graft diameter.
Fig. 7.
Two tunnels in the clavicle and two in the acromion process are then drilled at a diameter that matches the graft diameter. For clavicle tunnels, both limbs of the graft are held vertically parallel to each other, and two points are marked on the clavicle, which will be approximately at the same distance as the width of the coracoid process base. Two tunnel in the acromion are placed on the anterior and posterior side of the acromion.
The graft is crossed, and the medial end is pulled through the lateral tunnel and vice versa. (Fig. 8). The graft, passing the acromion tunnel (anterior an posterior) to provide adequate coverage for AC joint reconstruction. Acromioclavicular joint was overreduced and temporary fixation using Kirschner wire (Fig. 9) An Ultrabraid #5 suture and Endobutton are used to provide fixation augmentation and to avoid tissue cut-through (Fig. 10).
Fig. 8.
The graft is crossed, and the medial end is pulled through the lateral tunnel and the lateral end is pulled through the medial tunnel.
Fig. 9.
AC joint is placed in over reduced position, and temporary fixation using Kirschner wire.
Fig. 10.
Showing the final reconstruction of AC joint. An Ultrabraid #5 suture and Endobutton are used to provide fixation augmentation and to avoid tissue cut-through.
In addition to serving as reconstructed ligaments, the interposed graft also serves as an interposition spacer, replacing the function of the AC joint disc (Fig. 11). The deltotrapezial fascia is closed with interrupted non-absorbable sutures.
Fig. 11.
The interposed graft also serves as an interposition spacer, replacing the function of the AC joint disc.
2.3. Postoperative rehabilitation
The affected shoulder was immobilized in abduction brace for a minimum of 4 weeks. Active assisted external rotation until neutral position (00) and pendulum exercises were allowed on postoperative day 1. Active abduction and flexion was started 14 days after the operation. K-wires were removed about 4–6 weeks after the initial surgery. By the 7th week start the range of active movement. Muscle strengthening exercise were delayed until 3 months post operatively.
2.4. Clinical and radiological evaluation
Clinical outcomes were assessed postoperatively using Specific AC Score (SACS) and Nottingham Score. Anteroposterior radiographs for the affected AC joints and axillary radiographs for the affected side were collected immediately postoperatively and at the last follow up. The degree of displacement of the AC joint was evaluated measuring the CC distance on the anteroposterior view for vertical displacement and assessing the horizontal displacement on the axillary view.
We calculated the increase of CC distance using picture archiving and communicate system (PACS) on the injured shoulder over the non-injury side with the percentage of the CC distance (CC percentage), with a negative number indicating an over-reduction (Fig. 12). The maintenance of initial reduction and the effectiveness of surgery. First, a “loss of reduction” was defined as more than 25% increase of CC inter-space, comparing the CC percentage of the injured shoulder between immediately postoperatively and the final follow-up visit. A value of 25% was chosen because a side-to-side CC interspace difference of more than 25% indicates complete disruption of the CC ligaments.8
Fig. 12.
AC joint is reduced in over-reduction position.
2.5. Statistical analysis
The CC distance and CC percentage were compared between AC Joint fixation group with a AC joint reconstruction group immediately postoperative and 6 months post operatively. Clinical scores, horizontal translation were compared between groups by the Mann-Whitney test. CC Distance were compared using independent sample T test. CC percentage were compared using Kolmogorov smirnov test. The significance level was set at P = 0 0.005.
3. Result
A total of 29 patients fulfilled the inclusion criteria. 15 patients (51.7%) underwent AC joint reconstruction and 14 patients (48.3%) underwent AC joint fixation surgery. Mean last postoperative follow-up was 13.7 months for AC joint reconstruction, and 31.8 months for AC Joint fixation, represent change in our operative treatment strategies. We describe the demographic data in Table 1. In 10 patients with AC joint reconstruction, and 8 patients with AC joint fixation, the dominant side was involved. There were 24 men (82.8%) and 5 women (17.2%), with mean age is 38 years, the right shoulder was involved in 18 patients (62%). Mechanism of injury was fall from bike in 11 patients (37%), vehicle accident in 15 patients (51%), and a simple fall in 3 patients (12%). Associated lesion detected and mechanism of injury were comparable between the groups. The various time intervals with regard to operative treatment therefore did not bias results in further subgroup analysis.
Table 1.
Demographics data with mechanism of injury and associated lesion.
| AC Reconstruction | AC Fixation | P value | |
|---|---|---|---|
| Sex, n | |||
| Male | 13 | 11 | |
| Female | 2 | 3 | |
| Age, mean ± SD,y | 38 ± 12 | 39 ± 13 | 0.192 |
| Time from injury to surgery, mean ± SD,mo | 4.2 ± 3.8 | 4.6 ± 2.7 | 0.482 |
| Dominant side injury, n | 10 | 8 | |
| Mechanism of Injury,n | |||
| Bike | 5 | 6 | |
| Motorbike | 8 | 7 | |
| Simple fall | 2 | 1 | |
| Associated lesions,n | |||
| SLAP lesion | 4 | 2 | |
| Scapula fracture | 1 | 1 | |
| Labral tear | – | 1 | |
The median of SAC Score was 26 (1st- 3rd quartile 23.8–27.2, range 19–29) in the AC joint reconstruction group, and 20 (1st-3rd quartile 17.7–20.9, range 16–24) in the AC Joint fixation group. There were a significant different between groups with AC joint reconstruction and fixation group (20 vs. 8, p < 0.005) (Table 2). The median of Nottingham Score was 98 (1st- 3rd quartile 92–99, range 78–100) in the AC joint reconstruction group, and 80 (1st-3rd quartile 73.9–89, range 58–100) in the AC Joint fixation group. There were a significant different between groups with AC joint reconstruction and fixation group (19 vs. 10, p < 0.005) (Table 2). The mean value of the CC distance in AC joint Reconstruction group was 4.13 ± 0.35 and 4.07 ± 0.3 mm in AC joint fixation group.
Table 2.
Post operative assessment AC Reconstruction vs AC Fixation.
| Mean ± sd | Mean Difference (CI 95%) | P | |
|---|---|---|---|
| SAC Score | |||
| AC Reconstruction | 25.5 ± 3.0 | 6.2 (3.95–8.40) | 0.001 |
| AC Fixation | 19.4 ± 2.8 | ||
| Nottingham Score | |||
| AC Reconstruction | 95.73 ± 6.1 | 9.7(4.84–9.33) | 0.003 |
| AC Fixation | 81.64 ± 13.3 | ||
| CCD P0 | |||
| AC Reconstruction | 4.13 ± 1.3 | 0.062(0.96–1.086) | 0.902 |
| AC Fixation | 4.07 ± 1.3 | ||
| CCD PL | |||
| AC Reconstruction | 5.27 ± 1.5 | 0.124 (−1.501–1.749) | 0.877 |
| AC Fixation | 5.14 ± 2.5 | ||
| PT P0 | |||
| AC Reconstruction | 0.8 ± 0.13 | 0.9(3.95–8.40) | 0.003 |
| AC Fixation | 1.5 ± 0.13 | ||
| PT PL | |||
| AC Reconstruction | 1.01 ± 0.15 | 1.5 (1.24–1.81) | 0.001 |
| AC Fixation | 3.27 ± 0.15 | ||
SAC: Specific Acromioclavicular Score, CCD: Coracoclavicular Distance, PT: Posterior Translation, P0: Immediate postoperative, PL: last follow up.
There were no significant different in CC dstance between two groups in immediately post-operative (p > 0.05) (Table 2). The mean of horizontal translation in A joint reconstruction group was 0.8 mm and 1.5 in AC joint fixation group. There were a significatant different between two groups (p < 0.05) in immediately post-operative evaluation (Table 2).
In the last follow up post-operative evaluation, the mean value of the CC distance in AC joint Reconstruction group was 5.27 ± 0.48 and 5.14 ± 0.69 mm in AC joint fixation group. There were no significant different in CC dstance between two groups in the last follow up (p > 0.05) (Table 2). The mean of horizontal translation in AC joint reconstruction group was 1.0 and 3.27 in AC joint fixation group. There were a significatant different between two groups (p < 0.05) in immediately post-operative evaluation (Table 2).
Immediately post-operative, over reduction was found in 6 patient with AC joint reconstruction and 3 in AC joint fixation with a CC percentage less than 25%, no loss of reduction was found. Six patient develop loss of reduction with CC percentage >50%in AC joint fixation. There were no significant different in CC percentage between 2 groups (p < 0.05) (Table 3).
Table 3.
Coracoclavicular percentage
| CC Persentage |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Over |
normal |
Loss |
||||||||||
| N |
% |
N |
% |
N |
% |
|||||||
| P0 | PL | P0 | PL | P0 | PL | P0 | PL | P0 | PL | P0 | P6L | |
| AC Reconstruction | 6 | 0 | 40% | 0% | 9 | 14 | 60% | 93% | 0 | 1 | 0% | 7% |
| AC Fixation | 3 | 1 | 21.4% | 7% | 10 | 8 | 71.4% | 57% | 1 | 5 | 7.1% | 36% |
| Total | 9 | 1 | 31% | 3.4% | 19 | 22 | 65.5% | 68.9% | 1 | 6 | 3.4% | 20.7% |
CC: Coracoclavicular, P0: Immediate postoperative, PL: last follow up.
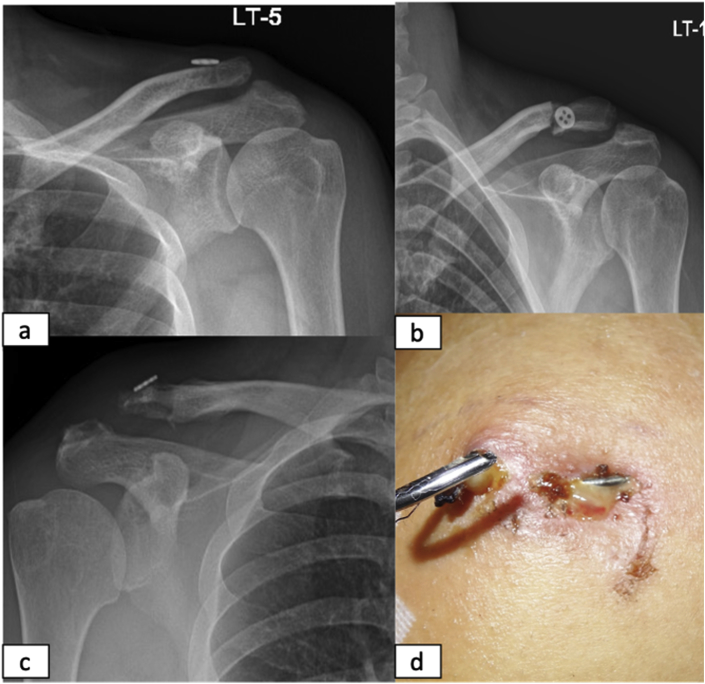
Complication (Fig. 13) developed in 5 patients (17%) including 2 mild osteolysis, 1 superficial infection, 1 implant failure, and 1 clavicle fracture. Associated injury was found in 6 patients with SLAP lesion (20%), 1 patient with labral tear (3%), and 2 patient with scapular fracture (6%). No significant different in clinical score (SAC score and Nottingham score) between patient with and without associate injury.
Fig. 13.
Complication including (a) loss of reduction, (b) clavicle fracture, (c) osteolysis, and (d) superficial infection.
4. Discussion
Korsten et al. conducted a systematic review comparing operative to nonoperative treatment of type III AC joint dislocations. And found that objective and subjective shoulder function outcomes were better in the operative group, especially in young adults.10 In our study, we treated a Rockwood grade III,IV,V AC Joint Injury with surgical intervention.
The incidence of coracoid or clavicular fractures was greater in open procedures compared with arthroscopic procedures but this procedure do not demonstrate significant differences in failure rates compared with open procedures.2 We prefer arthroscopic procedure to treat AC joint injuries to allow for excellent and safe visualization of the coracoid process and to reduce the risk of neurovascular structures damage when attempting to pass suture or graft material also for diagnosing and treating glenohumeral pathologies.11
Hook plates and K-wires had the highest rate of complications (26.3%), and unplanned reoperation rates were 1.2%, 2.8%, 0.9%, 5.4%, and 2.6% in free tendon graft, suspensory devices, synthetic ligament devices, modified Weaver-Dunn, and hook plate/K-wires techniques, respectively.12 Tauber et al. found that combined AC and CC ligament reconstruction better restored horizontal stability.
In this study, we compare 2 different reconstructive technique of AC joint injuries. Previous study have reported using synthetic material is a way to circumvent the use of tendon grafts and avoid donor site morbidity or excess cost.13 And tendon graft construct had an average failure rate 20.7% there is concern with this technique having the highest incidence of clavicular/coracoid fractures.14 Another study reported did not find significant differences in the fracture risk with respect to bone tunnel diameter.2,5
In our technique both limbs of the graft are held vertically parallel to each other, and two points are marked on the clavicle, which will be approximately at the same distance as the width of the coracoid process base. This more individualized approach is preferable, as a fixed distance may not consistently restore anatomy, since bone dimensions differ with each patient.
In both group we performed repair of AC capsule. The function of the AC capsule and CC ligaments allows a controlled rotation of more than 40°–50° for the acromion in relation to the lateral clavicle while preserving a centered motion.13 Combined stabilization of the AC capsule and CC ligaments demonstrated the greatest capacity to restore native stability against translational and rotational loads1
Because of this wide variety, it is hard and nearly impossible to compare clinical data. There is no gold standard for clinical evaluation in AC joint injuries. One of the main reasons these scores were required is that commonly used shoulder scores were developed to assess degenerative shoulder pathologies. In this study we use the Specific AC Score (SACS) and Nottingham Clavicle Score (NCS). Both of these scores have been validated for AC joint pathologies. Our study found that AC joint reconstruction group have significantly better clinical score compare with AC joint fixation.15
No gold standard for diagnostic measures of AC joint pathologies.3 We found that there is no significant different in CC distance between two groups, immediately after operation and in the last radiological evaluation. But we found a significantly different in posterior translation between two groups, immediately after operation and in the last radiological evaluation. And 6 patients was found loss of reduction at the last follow up in AC joint fixation group. As the previous study reported suture with Endobutton provided equivalent loss of reduction 18.4%.2
Complication developed in 5 patients (17%) including 2 mild osteolysis, 1 superficial infection, 1 implant failure, and 1 clavicle fracture. Previous studies have reported complication rates for these procedures to be as high as 30%,(49) and include loss of reduction (29%),(40) clavicle fracture (18%),(18) infection (6%) and hardware-related issues (4%).Another study, the most common complications were infection (6.3%), fracture of the coracoid or distal clavicle (5.7%), and hardware/button failure (4.2%).2
Associated injury was found in 6 patients with SLAP lesion (20%), 1 patient with labral tear (3%), and 2 patient with scapular fracture (6%). As in another study, recorded 7 SLAP lesions within 42 grade V AC joint separations (16.7%).12 And with arthroscopic assisted we perform diagnostic and treatment of associated injury of AC joint separation.
5. Conclusion
Although both complication and failure after ac joint reconstruction or repair remain significant crucial challenges, from our study we conclude that anatomic AC joint reconstruction have a better outcome rather than ac joint fixation. In this technique we restore the anatomy, reconstruct cc ligament and reinforced the ac ligament. And it is reliable for high grade acromioclavicular joint injury.
Declaration of competing interest
Both authors declare that they do not have any conflict of interest. Both authors have nothing to disclose.
Contributor Information
Bancha Chernchujit, Email: arrisna.ortho@gmail.com.
Arrisna Artha, Email: arrisna.ortho@gmail.com, arrisnarthaidaayu@gmail.com.
References
- 1.Dyrna F., Imhoff F.B., Haller B. Primary stability of an acromioclavicular joint repair is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med. 2018;46(14):3471–3479. doi: 10.1177/0363546518807908. [DOI] [PubMed] [Google Scholar]
- 2.Gowd A.K., Liu J.N., Cabarcas B.C. Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med. 2018:1–14. doi: 10.1177/0363546518795147. [DOI] [PubMed] [Google Scholar]
- 3.Braun S., Imhoff A.B., Martetschlaeger F. Primary fixation of acromioclavicular joint disruption. Oper Tech Sports Med. 2014;22(3):221–226. doi: 10.1053/j.otsm.2014.03.005. [Internet] Available at. [DOI] [Google Scholar]
- 4.Lee S., Bedi A. Shoulder acromioclavicular joint reconstruction options and outcomes. Curr Rev Musculoskelet Med. 2016;9(4):368–377. doi: 10.1007/s12178-016-9361-8. [Internet] Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cano-Martínez J.A., Nicolás-Serrano G., Bento-Gerard J., Picazo-Marín F., Andrés-Grau J. Acute high-grade acromioclavicular dislocations treated with triple button device (MINAR): preliminary results. Injury. 2016;47(11):2512–2519. doi: 10.1016/j.injury.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 6.Dyrna F.G.E., Imhoff F.B., Voss A. The integrity of the acromioclavicular capsule ensures physiological centering of the acromioclavicular joint under rotational loading. Am J Sports Med. 2018;46(6):1432–1440. doi: 10.1177/0363546518758287. [DOI] [PubMed] [Google Scholar]
- 7.Natera Cisneros L., Sarasquete Reiriz J. Unstable acromioclavicular joint injuries: is there really a difference between surgical management in the acute or chronic setting? J Orthop. 2017;14(1):10–18. doi: 10.1016/j.jor.2016.10.011. [Internet] Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spencer H.T., Hsu L., Sodl J., Arianjam A., Yian E.H. Radiographic failure and rates of re-operation after acromioclavicular joint reconstruction: a comparison of surgical techniques. Bone Jt J. 2016;98B(4):512–518. doi: 10.1302/0301-620X.98B4.35935. [DOI] [PubMed] [Google Scholar]
- 9.Chernchujit B., Tischer T., Imhoff A.B. Arthroscopic reconstruction of the acromioclavicular joint disruption: surgical technique and preliminary results. Arch Orthop Trauma Surg. 2006;126(9):575–581. doi: 10.1007/s00402-005-0073-6. [DOI] [PubMed] [Google Scholar]
- 10.Korsten K., Gunning A.C., Leenen L.P.H. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. Int Orthop. 2014;38(4):831–838. doi: 10.1007/s00264-013-2143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chernchujit B., Parate P. Surgical technique for arthroscopy-assisted anatomical reconstruction of acromioclavicular and coracoclavicular ligaments using autologous hamstring graft in chronic acromioclavicular joint dislocations. Arthrosc Tech. 2017;6(3) doi: 10.1016/j.eats.2017.01.009. e641–8. Available at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moatshe G., Kruckeberg B.M., Chahla J. Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: a systematic review of clinical and radiographic outcomes. Arthrosc - J Arthrosc Relat Surg. 2018;34(6):1979–1995. doi: 10.1016/j.arthro.2018.01.016. [Internet] e8. Tersedia pada: [DOI] [PubMed] [Google Scholar]
- 13.Triantafyllopoulos I.K., Lampropoulou-Adamidou K., Schizas N.P., Karadimas E.V. Surgical treatment of acute type V acromioclavicular joint dislocations in professional athletes: an anatomic ligament reconstruction with synthetic implant augmentation. J Shoulder Elbow Surg. 2017;26(12) doi: 10.1016/j.jse.2017.05.032. [Internet] e369–75. Available at: [DOI] [PubMed] [Google Scholar]
- 14.Banffy M.B., van Eck C.F., ElAttrache N.S. Clinical outcomes of a single-tunnel technique for coracoclavicular and acromioclavicular ligament reconstruction. J Shoulder Elbow Surg. 2018;27(6):S70–S75. doi: 10.1016/j.jse.2017.11.032. [Internet] [DOI] [PubMed] [Google Scholar]
- 15.Barwood S.A., French J.A., Watson L.A., Balster S.M., Hoy G.A., Pizzari T. The Specific AC Score (SACS): a new and validated method of assessment of isolated acromioclavicular joint pathology. J Shoulder Elbow Surg. 2018;27(12):2214–2223. doi: 10.1016/j.jse.2018.04.026. Available at: [DOI] [PubMed] [Google Scholar]