Abstract
Rhombencephalosynapsis is a rare defect in the development of the cerebellum, characterized by partial or total agenesis of the vermis, with fusion of the cerebellar hemispheres in the midline. It is usually related to Gómez-López-Hernández Syndrome (cerebellar-trigeminal dermal dysplasia) and VACTERL association association (vertebral defects, vascular anomalies, anal atresia, cardiac anomalies, tracheoesophageal fistula with esophageal atresia, renal dysplasia and limb anomalies). A 5-year-old female patient with spastic cerebral palsy and hydrocephalus presented here, neuroimages documented the next features: absence of cerebellar vermis, periventricular leukomalacia, cerebellar tonsils descent and rhombencephalosynapsis. Other important imaging findings and associations in these cases are discussed.
Keywords: Rhombencephalosynapsis, VACTERL, MRI, Cerebellar abnormalities, Malformation
Introduction
Posterior fossa malformations are classified in 2 groups: malformations with large posterior fossa and malformations with normal or small posterior fossa. Rhombencephalosynapsis (RES) correspond to the second group. It is a rare defect in the development of the cerebellum, characterized by partial or total agenesis of the vermis, with fusion of the cerebellar hemispheres in the midline, with main involvement of the dorsal portion of the vermis [1,2]. This condition appears sporadically but a genetic relationship is presumed, possibly due to the under-expression of a dorsalization gene [3,4]. It has been reported that the frequency of RES is 0.13% [5]. Almost all published cases have been isolated, or can be found in relation to other types of brain malformations, VACTERL association or Gómez-López-Hernández syndrome [1,3,6]. This article reports a new case of RES diagnosed by MRI in a 5-year-old patient with spastic cerebral palsy and obstructive hydrocephalus.
Case report
A 5-year-old female patient, with a history of severe mental retardation, and obstructive hydrocephalus with ventriculoperitoneal shunt and spastic cerebral palsy. She is referred to the Diagnostic Imaging Department for a cerebral-cervical and lumbosacral spine magnetic resonance imaging under general anesthesia, which was performed without complications in a Toshiba Vantage Titan 1.5 Teslas. MRI documented the absence of cerebellar vermis with continuity of the hemisphere folias in the midline (Fig. 1A, B and C); descending of the cerebellar tonsils reaching the level of C1 (Fig. 2A, B and C), marked thinning of the corpus callosum with radial arrangement of posterior gyros; as well as thinning of the white matter in both cerebral hemispheres mainly in parieto-occipital areas (Fig. 3A and B), and T2 hyperintensity of occipital subependymal white matter (Fig. 4A and B). Additionally, findings showed ventricular shunt system with right anterior catheter, collapse of the right ventricle and irregularities of the walls of the ventricular atria (Fig. 5A, B, C and D).
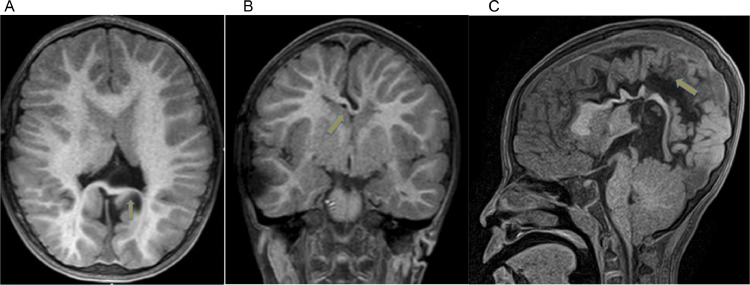
Fig. 1.
Cerebellar tonsils descent, that reaches the level of C1 (Arrow) in Axial T1 sequence (Fig.1A). Sagittal T1 (Fig.1B). Coronal T1 (Fig.1C) sections.
Fig. 2.
Marked thinning of the corpus callosum (arrow) in Fig.2A, predominantly in the body and splenium (arrow) in Fig.2B, associated with posterior gyros radial organization (arrow) in Fig. 2C. MRI T1 sequences.
Fig. 3.
Decrease in white matter volume with occipital predominance is observed in the axial sections in T1 at the level of the basal ganglia (arrow) (3A) and above basal ganglia level (arrow) (3B).
Fig. 4.
Absence of the cerebellar vermis represented in axial (arrow) (4A) and coronal (arrow)(4B) section in T2 sequences.
Fig. 5.
Axial sections show hyperintense aspect of subependymal white matter in occipital lobes (arrow). (5A) T2 sequence, (5B) FLAIR, (5C) diffusion representation and (5D) ADC maps.
Imaging findings of this patient cannot be framed in any syndromic diagnosis associated with this condition; however, it has defects in the development of the supratentorial gyros, rhombencephalosynapsis and Arnold Chiari type 1.
Discussion
This is a new case of RES diagnosed by MRI in a 5-year-old live patient. It is a rare entity with few reports in the literature and without exact knowledge of its prevalence; it is still considered as a sporadic condition with poorly understood etiological factors [7], similar to known genetic brain malformations, the RES malformation is highly stereotyped, yet no genetic causes have been identified. [7] RES is associated with a wide spectrum of anomalies and its diagnosis usually occurs at an earlier age. It is suspected after 22 weeks of gestation and diagnosed usually by ultrasound. Generally the abnormality is suggested by ventriculomegaly [8]. Ongoing genomic investigations will incorporate strategies to address the limitations of current genetic approaches for the diagnosis [7]. The additional anomalies reported in association with RES are variable; hydrocephalus or ventriculomegaly, corpus callosum dysgenesis, and the absence of septum pellucidum are the most commonly associated anomalies whit rhombencephalosynapsis. Thalamus, tectum and fornixes fusion, hypoplasia of the temporal lobes, olivary nuclei, anterior commissure and optic chiasm and agenesis of the posterior lobe of the pituitary can be seen occasionally. On the other hand, extracranial anomalies are very rare [6]. Patients can be included in four categories: (1) RES associated with the Gómez-López-Hernández syndrome, also known as cerebellar-trigeminal-dermal dysplasia; (2) RES with association VACTERL; (3) RES with atypical holoprosencephaly mostly occipital, and (4) isolated RES [1,8]. In this case, other associated brain malformations are identified, such as hydrocephalus, dysgenesis of the corpus callosum and Arnold Chiari type 1. However, it is not included within any syndromic diagnosis described. The severity of the clinical manifestations and the prognosis of RES depends on the findings of the posterior fossa and associated anomalies [6].
In conclusion, in the presence of RES it is important to evaluate in detail every developmental defect, and possible associated syndromes. Given the low prevalence of this pathology, it is important that medical community continue reporting its findings and associations, to build the natural history of the disease.
Contributor Information
Nathalia Tafur Gómez, Email: nathaliatago@unisabana.edu.co.
Carlos Hernán Roa Mejía, Email: carlos.roa@shaio.org.
Juan Carlos Aldana Leal, Email: juan.aldana@shaio.org.
References
- 1.Ishak G.E., Dempsey J.C., Shaw D.W.W., Tully H., Adam M.P., Sanchez-Lara P.A. Rhombencephalosynapsis: a hindbrain malformation associated with incomplete separation of midbrain and forebrain, hydrocephalus and a broad spectrum of severity. Brain. 2012;135(5):1370–1386. doi: 10.1093/brain/aws065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agut T., Muchart J., Delgadillo V., García-Alix A. Rombencefalosinapsis, una rara alteración del desarrollo del cerebelo de fácil diagnóstico. An Pediatr. 2014;81(6):e3–e4. doi: 10.1016/j.anpedi.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 3.Tully H.M., Dempsey J.C., Ishak G.E., Adam M.P., Curry C.J.R., Sanchez-Lara P. Beyond Gómez-López-Hernández syndrome: recurring phenotypic themes in rhombencephalosynapsis. Am J Med Genet Part A. 2012;158(10):2393–2406. doi: 10.1002/ajmg.a.35561. A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarnat H. Molecular genetic classification of central nervous system malformations. J Child Neurol. 2000;15:675–687. doi: 10.1177/088307380001501007. [DOI] [PubMed] [Google Scholar]
- 5.Sener R.N. Unusual MRI findings in rhombencephalosynapsis. Comput Med Imaging Graph. 2000;24(4):277–282. doi: 10.1016/s0895-6111(00)00025-2. [DOI] [PubMed] [Google Scholar]
- 6.Chemli J., Abroug M., Tlili K., Harbi A. Rhombencephalosynapsis diagnosed in childhood: clinical and MRI findings. Eur J Paediatr Neurol. 2007;11(1):35–38. doi: 10.1016/j.ejpn.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Aldinger K.A., Dempsey J.C., Tully H.M., Grout M.E., Mehaffey M.G., Dobyns W.B. Rhombencephalosynapsis: fused cerebellum, confused geneticists. Am J Med Genet Part C Semin Med Genet. 2018;178(4):432–439. doi: 10.1002/ajmg.c.31666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasquier L., Marcorelles P., Loget P., Pelluard F., Carles D., Perez M.J. Rhombencephalosynapsis and related anomalies: a neuropathological study of 40 fetal cases. Acta Neuropathol. 2009;117(2):185–200. doi: 10.1007/s00401-008-0469-9. [DOI] [PubMed] [Google Scholar]