Abstract
In a recent publication [1], we introduced and described a novel means (i.e. VT Prediction Model) to correctly categorize wide complex tachycardias (WCTs) into ventricular tachycardia (VT) and supraventricular wide complex tachycardia (SWCT) using routine measurements shown on electrocardiogram (ECG) paper recordings. In this article, we summarize data components relating to the derivation and validation of the VT Prediction Model.
Keywords: Electrocardiogram, Wide complex tachycardia, Ventricular tachycardia, Supraventricular tachycardia, Computerized electrocardiogram interpretation
Specifications table
| Subject area | Cardiology |
| More specific subject area | Electrocardiology, computerized electrocardiogram interpretation |
| Type of data | Tables, figures, and images |
| How data was acquired | Review of health records and automated measurements provided by computerized electrocardiogram interpretation software (MUSE by GE Healthcare; Milwaukee, WI) |
| Data format | Raw and analyzed data |
| Parameters for data collection | Evaluated electrocardiograms were paired wide complex tachycardia and baseline electrocardiograms attained within clinical settings throughout the entire Mayo Clinic enterprise between September 2011 and December 2018. |
| Description of data collection | Evaluated electrocardiograms were standard 12-lead recordings obtained from Mayo Clinic's centralized electrocardiogram data archives. Wide complex tachycardias were required to fulfill wide complex tachycardia criteria (QRS duration ≥ 120 ms; heart rate ≥ 100 bpm) plus a formal ECG laboratory interpretation of (i) "ventricular tachycardia," (ii) "supraventricular tachycardia," or (iii) "wide complex tachycardia." Baseline electrocardiograms were either the first subsequent electrocardiogram or most proximate that did not fulfill wide complex tachycardia criteria. |
| Data source location | Mayo Clinic |
| Data accessibility | Data is included in this article |
| Related research article | A.M. May, C.V. DeSimone, A.H. Kashou, H. Sridhar, D.O. Hodge, R. Carter, G. Lin, S.J. Asirvatham, P.A. Noseworthy, A.J. Deshmukh. The VT Prediction Model: A Simplified Means to Differentiate Wide Complex Tachycardias. Journal of Cardiovascular Electrophysiology. December 2019. 10.1111/jce.14321. |
Value of the data
-
•
Enclosed data summarizes the patient demographics, clinical features, and ECG laboratory interpretation codes of patient cohorts used to derive and validate a novel WCT differentiation method known as the VT Prediction Model. Featured data also describes electrocardiographic characteristics of WCTs accurately and erroneously classified by the VT Prediction Model.
-
•
Data would be valuable to researchers wanting to understand the patient demographics, clinical characteristics, and electrocardiographic features of WCT events customarily encountered in general clinical practice.
-
•
Data would be of value to researchers aiming to specify clinical and ECG features to be examined in prospective evaluations that compare the diagnostic performance of WCT differentiation algorithms.
1. Data description
Table 1 summarizes the clinical and ECG laboratory diagnosis data for the derivation cohort. Heart rhythm or non-heart rhythm cardiologists were responsible for most (85.6%) clinical diagnoses. The ECG laboratory assigned definitive or probable interpretive diagnoses to a sizeable majority (94.8%) of WCTs. A minority of evaluated WCTs (32.1%) were derived from patients who underwent an electrophysiology procedure. A sizeable proportion of evaluated WCTs (38.2%) was derived from patients who possessed an implantable intra-cardiac device (e.g., pacemaker).
Table 1.
Derivation Cohort: clinical and ECG laboratory diagnosis.
| SWCT (n = 328) | VT (n = 273) | P-Value | |
|---|---|---|---|
| Diagnosing provider | |||
| Heart rhythm cardiologists | 141 (43.0) | 248 (90.8) | |
| Non-heart rhythm cardiologists | 109 (33.2) | 17 (6.2) | < 0.0001 |
| Non-cardiologists | 78 (23.8) | 8 (2.9) | |
| ECG lab interpretation | |||
| Definite VT | 10 (3.0) | 226 (82.8) | < 0.0001 |
| Probable VT | 16 (4.9) | 26 (9.5) | |
| Definite SWCT | 265 (80.8) | 6 (2.2) | |
| Probable SWCT | 16 (4.9) | 5 (1.8) | |
| Undifferentiated | 21 (6.4) | 10 (3.7) | |
| Time separation between WCT and baseline ECG (hours) | |||
| Mean (SD) | 381.7 (2183.2) | 160.2 (632.4) | 0.77 |
| Median | 6.3 | 8.1 | |
| Q1, Q3 | 1.0, 43.1 | 1.1, 46.3 | |
| Time separation between WCT and baseline ECG | |||
| < 3 h | 134 (40.9) | 111 (40.8) | 0.04 |
| 3 - 24 h | 88 (26.8) | 63 (23.1) | |
| 24 h - 30 days | 78 (23.8) | 87 (319) | |
| > 30 days | 28 (8.5) | 12 (4.4) | |
| Electrophysiology procedure | |||
| Yes | 51 (15.5) | 142 (52.0) | < 0.0001 |
| Implanted Device | |||
| Yes | 49 (14.9) | 181 (66.3) | < 0.0001 |
Numbers in parentheses are percent (%) of n or standard deviation. SD = standard deviation; SWCT = supraventricular tachycardia; VT = ventricular tachycardia.
Table 2 describes the patient characteristics of the derivation cohort. The VT group included more ECG pairs from patients with coronary artery disease, prior myocardial infarction, ischemic cardiomyopathy, non-ischemic cardiomyopathy, active antiarrhythmic drug use, and implanted cardioverter-defibrillator. The supraventricular wide complex tachycardia (SWCT) group comprised more patients having an implanted pacemaker. Baseline ECGs demonstrating ventricular pacing were more prevalent in the ventricular tachycardia (VT) group than the SWCT group. Baseline bundle branch block was more common in the SWCT group than the VT group. No SWCTs (0.0%) demonstrated pre-excitation.
Table 2.
Derivation cohort: patient characteristics.
| SWCT (n = 328) | VT (n = 273) | P-Value | |
|---|---|---|---|
| Age (years) | |||
| Mean (SD) | 70.6 (14.6) | 65.8 (13.1) | < 0.0001 |
| Range | 18.0 - 98.0 | 27.0 - 90.0 | |
| Gender | |||
| Male | 212 (64.6) | 225 (82.4) | < 0.0001 |
| Female | 116 (35.4) | 48 (17.6) | |
| Clinical Characteristics | |||
| Coronary artery disease | 160 (48.8) | 188 (68.9) | < 0.0001 |
| Prior myocardial infarction | 93 (28.4) | 157 (57.5) | < 0.0001 |
| Prior heart surgery | 123 (37.5) | 118 (43.2) | 0.15 |
| Congenital heart disease | 18 (5.5) | 19 (7.0) | 0.45 |
| Anti-arrhythmic drug use | 52 (15.9) | 165 (60.4) | < 0.0001 |
| Ischemic cardiomyopathy | 52 (15.9) | 138 (50.5) | < 0.0001 |
| Non-ischemic cardiomyopathy | 77 (23.5) | 89 (32.6) | 0.01 |
| AICD | 22 (6.7) | 176 (64.5) | < 0.0001 |
| Pacemaker | 27 (8.2) | 5 (1.8) | 0.0005 |
| Left ventricular ejection fraction (%) | |||
| Unknown LVEF | 14 (4.3) | 1 (0.4) | < 0.0001 |
| LVEF (<= 30) | 66 (20.1) | 118 (43.2) | |
| LVEF (49 - 31) | 59 (18.0) | 85 (31.1) | |
| LVEF (>= 50) | 189 (57.6) | 69 (25.3) | |
| Baseline ECG | |||
| Baseline bundle branch block | 217 (66.2) | 39 (14.3) | < 0.0001 |
| Baseline ventricular pacing | 19 (5.8) | 110 (40.3) | < 0.0001 |
| SWCT with pre-excitation | |||
| Yes | 0 (0.0%) | *** | *** |
Numbers in parentheses are percent (%) of n or standard deviation. AICD = automatic implantable cardioverter-defibrillator; LVEF = left ventricular ejection fraction; SD = standard deviation; SWCT = supraventricular tachycardia; VT = ventricular tachycardia.
Table 3 summarizes the clinical and ECG laboratory diagnosis data for the validation cohort. Heart rhythm or non-heart rhythm cardiologists were responsible for most (90.5%) clinical diagnoses. Definitive or probable diagnoses were assigned to the vast majority (95.0%) of WCTs interpreted by the ECG laboratory. About one-third (34.4%) of evaluated WCTs were derived from patients who underwent an electrophysiology procedure. A substantial percentage (40.2%) of evaluated WCTs were derived from patients who possessed an implantable intra-cardiac device.
Table 3.
Validation cohort: clinical and ECG laboratory diagnosis.
| SWCT (n = 144) | VT (n = 97) | P-Value | |
|---|---|---|---|
| Diagnosing provider | |||
| Heart rhythm cardiologists | 59 (41.0) | 82 (84.5) | < 0.001 |
| Non-heart rhythm cardiologists | 63 (43.8) | 14 (14.4) | |
| Non-cardiologists | 22 (15.3) | 1 (1.0) | |
| ECG lab interpretation | |||
| Definite VT | 9 (6.2) | 68 (70.1) | < 0.001 |
| Probable VT | 1 (0.7) | 9 (9.3) | |
| Definite SWCT | 87 (60.4) | 3 (3.1) | |
| Probable SWCT | 41 (28.5) | 11 (11.3) | |
| Undifferentiated | 6 (4.2) | 6 (6.2) | |
| Time separation between WCT and baseline ECG (hours) | |||
| Mean (SD) | 275.9 (1293.8) | 104.3 (434.8) | 0.075 |
| Median | 10.1 | 5.1 | |
| Q1, Q3 | 1.5, 46.6 | 0.6, 33.8 | |
| Time separation between WCT and Baseline ECG | |||
| < 3 h | 47 (32.6) | 45 (46.4) | 0.174 |
| 3 - 24 h | 46 (31.9) | 23 (23.7) | |
| 24 h - 30 days | 46 (31.9) | 27 (27.8) | |
| > 30 days | 5 (3.5) | 2 (2.1) | |
| Electrophysiology procedure | |||
| Yes | 26 (18.1) | 57 (58.8) | < 0.001 |
| Implanted device | |||
| Yes | 27 (18.8) | 70 (72.2) | < 0.001 |
Numbers in parentheses are percent (%) of n or standard deviation. SD = standard deviation; SWCT = supraventricular tachycardia; VT = ventricular tachycardia.
Table 4 details the clinical characteristics of patients comprising the validation cohort. The VT group included more ECG pairs from patients with coronary artery disease, prior myocardial infarction, ischemic cardiomyopathy, active antiarrhythmic drug use, and implanted cardioverter-defibrillator. The SWCT group comprised more ECG pairs from patients having an implanted pacemaker. Baseline ECGs demonstrating ventricular pacing were more prevalent in the VT group than the SWCT group. Baseline bundle branch block was more common in the SWCT group than the VT group. Four SWCTs (2.8%) demonstrated pre-excitation.
Table 4.
Validation cohort: clinical and ECG laboratory diagnosis.
| SWCT (n = 144) | VT (n = 97) | P-Value | |
|---|---|---|---|
| Age (years) | |||
| Mean (SD) | 69.4 (14.8) | 67.5 (10.8) | 0.027 |
| Gender | |||
| Male | 102 (70.8) | 87 (89.7) | < 0.001 |
| Female | 42 (29.2) | 10 (10.3) | |
| Clinical Characteristics | |||
| Coronary artery disease | 54 (37.5) | 71 (73.2) | < 0.001 |
| Prior myocardial infarction | 34 (23.6) | 67 (69.1) | < 0.001 |
| Prior heart surgery | 45 (31.2) | 29 (29.9) | 0.823 |
| Congenital heart disease | 5 (3.5) | 0 (0.0) | 0.064 |
| Anti-arrhythmic drug use | 25 (17.4) | 48 (49.5) | < 0.001 |
| Ischemic cardiomyopathy | 27 (18.8) | 63 (64.9) | < 0.001 |
| Non-ischemic cardiomyopathy | 49 (34.0) | 24 (24.7) | 0.124 |
| AICD | 21 (14.6) | 70 (72.2) | < 0.001 |
| Pacemaker | 7 (4.9) | 0 (0.0) | 0.028 |
| Left ventricular ejection fraction (%) | |||
| Unknown LVEF | 7 (4.9) | 1 (1.0) | < 0.001 |
| LVEF (<= 30) | 35 (24.3) | 45 (46.4) | |
| LVEF (49 - 31) | 27 (18.8) | 31 (32.0) | |
| LVEF (>= 50) | 75 (52.1) | 20 (20.6) | |
| Baseline ECG | |||
| Baseline bundle branch block | 90 (62.5) | 17 (17.5) | < 0.001 |
| Baseline ventricular pacing | 8 (5.6) | 33 (34.0) | < 0.001 |
| SWCT with Pre-excitation | |||
| Yes | 4 (2.8) | *** | *** |
Numbers in parentheses are percent (%) of n or standard deviation. AICD = automatic implantable cardioverter-defibrillator; LVEF = left ventricular ejection fraction; SD = standard deviation; SWCT = supraventricular tachycardia; VT = ventricular tachycardia.
Table 5 summarizes electrocardiographic characteristics of correct and incorrect diagnoses established by the VT Prediction Model for the derivation cohort. According to a 50% VT probability partition to establish VT diagnoses (VT > = 50.0% and SWCT < 50.0%), 53 out of 278 (19.1%) clinical VTs were incorrectly branded as SWCT by the VT Prediction Model. In comparison with correctly identified VTs, erroneous classifications of clinical VT as SWCT displayed shorter WCT QRS duration and constrained changes in QRS duration, QRS axis, and T axis between paired baseline and WCT ECGs. According to a 50% VT probability partition to establish VT diagnoses (VT > = 50.0% and SWCT < 50.0%), 38 out of 323 (11.8%) clinical SWCTs were erroneously categorized as VT by the VT Prediction Model. In comparison with correctly identified SWCTs, erroneous classifications of clinical SWCT as VT demonstrated more prolonged WCT QRS intervals and larger changes in QRS duration, QRS axis, and T axis between paired baseline and WCT ECGs.
Table 5.
Derivation cohort: correct and erroneous WCT diagnoses.
| WCT (n = 601) |
||||||
|---|---|---|---|---|---|---|
| VT (n = 273) |
SWCT (n = 328) |
|||||
| Erroneous SWCT Prediction (n = 53) | Correct VT Prediction (n = 220) | P-value | Erroneous VT Prediction (n = 38) | Correct SWCT Prediction (n = 290) | P-value | |
| WCT QRS duration (ms) | 147.7 (19.7) | 183.9 (30.3) | < 0.0001 | 163.6 (20.1) | 140.3.6 (15.7) | < 0.0001 |
| QRS duration change (ms) | 24.7 (17.9) | 51.5 (35.9) | < 0.0001 | 41.5 (33.6) | 13.7 (14.2) | < 0.0001 |
| QRS axis change (°) | 35.2 (36.5) | 99.0 (54.8) | < 0.0001 | 68.7 (56.9) | 20.1 (23.7) | < 0.0001 |
| T axis change (°) | 50.1 (46.4) | 101.8 (55.8) | < 0.0001 | 92.9 (47.8) | 34.1 (35.1) | < 0.0001 |
Displayed numbers represent mean values. Numbers in parentheses are standard deviation. The erroneous VT prediction group comprise clinical SWCTs assigned high VT probability (>= 50%). The erroneous SWCT prediction group comprise clinical VTs assigned low VT probability (< 50%). SWCT = supraventricular wide complex tachycardia; VT= ventricular tachycardia; WCT = wide complex tachycardia.
Fig. 1 illustrates the diagnostic performance of the VT Prediction Model for the derivation cohort (AUC 0.924; CI 0.903 – 0.944).
Fig. 1.
VT prediction model diagnostic performance: derivation cohort.
Fig. 2 illustrates the diagnostic performance of the VT Prediction Model when implemented on the validation cohort (AUC 0.900; CI 0.862 – 0.939).
Fig. 2.
VT prediction model diagnostic performance: validation cohort.
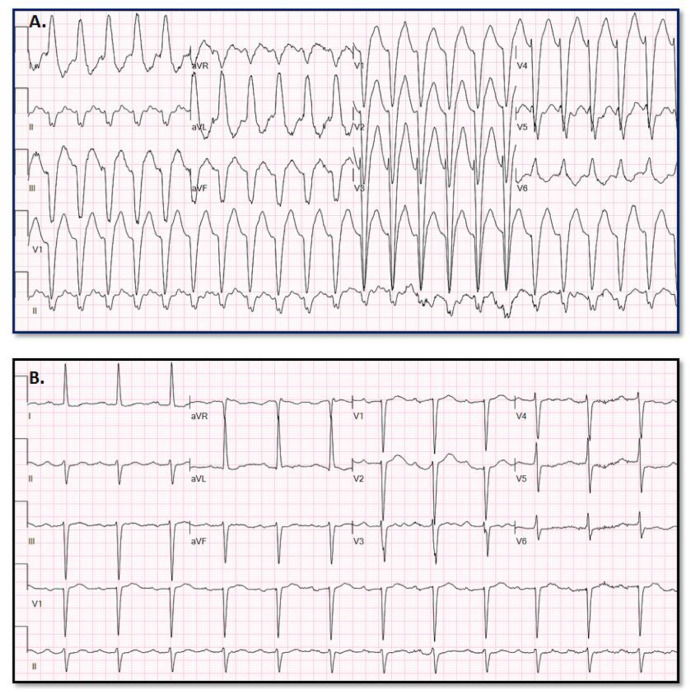
Fig. 3 provides an example of paired VT (A) and baseline (B) ECGs assigned high VT probability (99.0006%) by the VT Prediction Model. WCT QRS duration = 182 ms; QRS duration change = 48 ms; QRS axis change = 134°; T axis change = 93°
Fig. 3.
Appropriate high VT probability assignment.
Fig. 4 provides an example of paired SWCT (A) and baseline (B) ECGs assigned low VT probability (4.3609%) by the VT Prediction Model. WCT QRS duration = 130 ms; QRS duration change = 46 ms; QRS axis change = 1°; T axis change = 8°
Fig. 4.
Appropriate low VT probability assignment.
Fig. 5 provides an example of paired SWCT (A) and baseline (B) ECGs assigned low VT probability (6.3613%) by the VT Prediction Model. WCT QRS duration = 120 ms; QRS duration change = 36 ms; QRS axis change = 48°; change T axis change = 13°
Fig. 5.
Appropriate low VT probability assignment.
Fig. 6 provides an example of paired VT (A) and baseline (B) ECGs assigned low VT probability (9.8704%) by the VT Prediction Model. WCT QRS duration = 126 ms; QRS duration change = 6 ms; QRS axis change = 63°; T axis change = 30°
Fig. 6.
Erroneous low VT probability assignment.
Fig. 7 provides an example of paired SWCT (A) and baseline (B) ECGs assigned high VT probability (54.0039%) by the VT Prediction Model. WCT QRS duration = 170 ms; QRS duration change = 52 ms; QRS axis change = 3°; T axis change = 89°
Fig. 7.
Erroneous high VT probability assignment.
2. Experimental design, materials, and methods
Our recent publication [1] describes the derivation and implementation of a new WCT differentiation method that produces explicit VT probability estimations for paired WCT and baseline ECGs. In this report, a logistic regression model (i.e., VT Prediction Model) was derived and tested using two using separate patient cohorts: derivation and validation. First, a derivation cohort of paired WCT and baseline ECGs was evaluated to identify independent predictors to be consolidated into the VT Prediction Model. After that, the VT Prediction Model was trialed against a separate validation cohort of paired WCT and baseline ECGs. The overall diagnostic performance of the VT Prediction Model was appraised according to its agreement with the final clinical diagnosis established by patients' supervising physicians.
Paired WCT and baseline ECGs were derived from actual clinical settings throughout the entire Mayo Clinic enterprise between September 2011 and December 2018. Evaluated ECGs were standard 12-lead paper recordings (speed: 25 mm/s, voltage calibration: 10 mm/mV) acquired from Mayo Clinic's ECG data archives (GE Healthcare; Milwaukee, WI).
Included WCTs were required to fulfill WCT criteria (QRS duration ≥ 120 ms and heart rate ≥ 100 bpm) plus an official ECG laboratory interpretation of (1) "ventricular tachycardia," (2) "supraventricular tachycardia," or (3) "wide complex tachycardia." Baseline ECGs were either the first subsequent ECG (i.e., for the derivation cohort) or nearest ECG (i.e., for the validation cohort), not fulfilling WCT criteria.
The derivation cohort encompassed 601 paired WCT (273 VT, 328 SWCT) and baseline ECGs from 421 patients presenting to Mayo Clinic Rochester or Mayo Clinic Health System of South Eastern Minnesota (September 2011 through November 2016). The validation cohort comprised 241 WCT (97 VT, 144 SWCT) and baseline ECG pairs from 177 patients presenting to the whole Mayo Clinic enterprise (January 2018 through December 2018) – including three large medical centers (Rochester, Minnesota; Jacksonville, Florida; and Phoenix/Scottsdale, Arizona) and auxiliary patient care locations (e.g., community hospitals).
Data relating to clinical diagnosis, ECG laboratory examination, and patient characteristics were discovered from an electronic medical record review. Standard ECG measurements rendered by GE Healthcare's MUSE ECG interpretation software were acquired from archived ECG recordings. Basic arithmetical computations (QRS axis change, T wave axis change, QRS duration change) were processed using electronic measurements routinely displayed on ECG recordings.
The Mayo Clinic Institutional Review Board approved patient data acquisition and analysis. Similar patient selection processes and data reporting were previously adopted in a separate analysis [2,3].
Acknowledgments
Acknowledgments
No additional acknowledgments.
Competing interests
Authors, Adam May, Chris DeSimone, and Abhishek Deshmukh are obliged to disclose that they are "would be" beneficiaries of intellectual property that relates directly to this manuscript's content.
This technology was developed without industry funding or influence and was disclosed to Mayo Clinic Ventures, which possesses intellectual property rights. Attempts to market this invention to industry stakeholders have not yet taken place.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dib.2020.105515.
Appendix. Supplementary materials
References
- 1.May A.M., DeSimone C.V., Kashou A.H. The VT Prediction model: a simplified means to differentiate wide complex tachycardias. J. Cardiovasc. Electrophysiol. December 2019 doi: 10.1111/jce.14321. [DOI] [PubMed] [Google Scholar]
- 2.May A.M., DeSimone C.V., Kashou A.H. The WCT Formula: a novel algorithm designed to automatically differentiate wide-complex tachycardias. J. Electrocardiol. 2019;54:61–68. doi: 10.1016/j.jelectrocard.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 3.May A.M., DeSimone C.V., Kashou A.H. The wide complex tachycardia formula: derivation and validation data. Data Brief. 2019;24 doi: 10.1016/j.dib.2019.103924. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.