Abstract
During the last decades, further knowledge of hepatocellular carcinoma (HCC) molecular mechanisms has led to development of effective systemic treatments including tyrosine kinase inhibitors (TKIs) and immunotherapy. In this review, we describe first and second line systemic treatment options for advanced HCC. Several trials have evaluated new drugs for the treatment of HCC patients: In first line, lenvatinib resulted non-inferior to sorafenib and it can be used as alternative, even in the lack of evidence for sequential treatment options in second line after lenvatinib. Recently, atezolizumab plus bevacizumab have shown superiority over sorafenib in first-line. Sorafenib-regorafenib sequential administration in selected patients has opened a new paradigm of treatment in advanced HCC with a life expectancy exceeding two years. Other TKIs for second line treatment include cabozantinib and ramucirumab (specifically for patients with Alpha-fetoprotein values ≥ 400 ng/mL). The combination of TKIs with immunotherapy may represent a big step forward for these patients in the near future.
Keywords: Hepatocellular carcinoma, Systemic, Options, Sequencing, Advanced, Future
Core tip: The prognosis of advanced hepatocellular carcinoma (HCC) has been improved in the last years due to new available drugs for first and second line systemic treatments. Recent improvements in HCC molecular mechanisms have led to development of effective systemic treatments including tyrosine kinase inhibitors and immunotherapy. In this review, we describe first and second line systemic treatment options for advanced HCC focusing on sequencing therapy and comparison of different second line options.
INTRODUCTION
Primary liver cancer or hepatocellular carcinoma (HCC) is the fifth most common neoplasm and the third leading cause of cancer related death worldwide[1]. Its prognosis in advanced stages has been improved in the last years because of new available drugs for first and second line systemic treatment options[2].
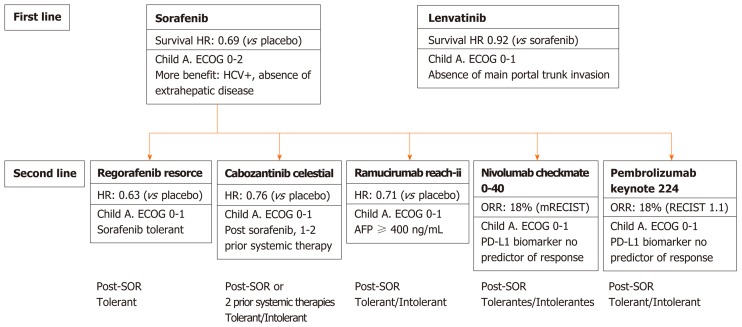
During the last decades, further knowledge of HCC molecular mechanisms has led to the development of effective systemic treatment including tyrosine kinase inhibitors (TKIs) and immunotherapy. In this review, we describe first and second line systemic treatment options for advanced HCC focusing on sequencing therapy (sorafenib-based treatment) and comparison of different second line options (Figure 1).
Figure 1.
First and second line therapies for advanced hepatocellular carcinoma. RECIST: Response Evaluation Criteria for Solid Tumors; ECOG: Eastern Cooperative Oncology Group; SOR: Sorafenib.
FIRST LINE SYSTEMIC TREATMENT
Sorafenib was the first effective treatment approved for advanced HCC[3]. Two double-blind, randomized clinical trials (RCTs) demonstrated a better overall survival (OS) with a relative risk reduction of death of 70% [HR (hazard ratio) of 0.69 [95% confidence interval (CI): 0.55; 0.87)] for sorafenib against placebo/best supportive care[3,4]. Likewise, a benefit was observed in prolonging time to radiological progression (TTP), evaluated through Response Evaluation Criteria for Solid Tumors (RECIST 1.0)[HR: 0.58 (95%CI: 0.45; 0.74)][5,6]. In these trials, sorafenib could be continued even after radiological tumor progression, i.e., until symptomatic progression, intolerance or death. The median TTP under sorafenib was 5.5 mo. In the SHARP and Asia-Pacific trials, although there was a low objective response rate (ORR) (less than 2%), stable disease (SD) was observed in more than 70% with a disease control rate (DCR) of 43% and 53%, respectively[3,4]. Thus, sorafenib reached its main primary end-point with a benefit in overall survival, even without significant tumor shrinkage. This phenomenon opened a paradigm in clinical oncology and trial design for systemic treatment for HCC.
Several observational cohort studies validated the use of sorafenib in the real life setting. The GIDEON study was an observational prospective cohort study whose primary objective was to evaluate the effectiveness of sorafenib in these scenarios, particularly in patients with advanced liver disease[7]. There was a higher incidence of adverse events (AEs) and treatment discontinuation due to AEs in patients with Child Pugh B-C when compared to Child Pugh A. Median survival was significantly lower in patients with unpreserved liver function. Other series from Italy and Argentina reported similar outcomes[8,9].
Some authors still argue that systemic chemotherapy has a therapeutic role in these patients since sorafenib showed a low radiological response, a poor gain in survival, absence of predictive response factors and a high cost. However, over the past decades, trials or uncontrolled interventional studies with doxorubicin[10-13], cisplatin, oxaliplatin or FOLFOX, gemcitabine-based GEMOX[14-19], capecitabine-based XELOX[20] or in combination with bevacizumab[21], have all failed with no proven efficacy and eventually accompanied by high toxicity rates. Finally, recent trials exploring the efficacy of sorafenib in combination with arterial chemotherapy have shown contradictory results[22,23].
Since 2008, different molecular pathways of HCC development and progression have been studied in depth. Based on these studies, many clinical trials were conducted testing new drugs for HCC first-line treatment. To date only lenvatinib has demonstrated to be non-inferior to sorafenib (Table 1). Sunitinib, an endothelial growth factor inhibitor (EGFR), has failed to demonstrate non-inferiority in a phase III RCT[24]. There was a lot of expectation with brivanib (BRISK-FL trial) given its anti-angiogenic effect and different inhibition of pathways than sorafenib (vascular-endothelial growth factor -VEGF- and fibroblast growth factor–FGF-pathways). However, it was also not efficient in a non-inferiority trial[25]. Other phase III trials failed to show superiority, including: erlotinib + sorafenib vs sorafenib + placebo (SEARCH trial, anti EGFR)[26], linifanib vs sorafenib (VEGF and platelet-derived growth factor inhibitor-PDGF)[27]. Likewise, dovitinib (VEGF, FGF and PDGF inhibitor)[28] and bevacizumab (anti-VEGF monoclonal antibody) did not demonstrate efficacy in phase II trials, presenting excessive toxicity and high incidence of sepsis, not allowing for further studies[29].
Table 1.
First line agents failed for the treatment of advanced hepatocellular carcinoma
| Study drug | Population | Design-intervention | Results |
| Sunitinib (EGFR), Cheng et al[24], 2013 | n = 1074, BCLC B-C, ECOG 0-1, Child Pugh A/B | RCT Fase III. Non-inferiority. Sunitinib vs Sorafenib | Failed to reach its primary end-point. Higher rate of EAs |
| Brivanib (VEGF, FGF), Johnson et al[25], 2013 | n = 1150, BCLC B-C, ECOG 0-1, Child Pugh A/B | RCT Fase III. Non-inferiority. Brivanib vs Sorafenib (Bristol) | Failed to reach its primary end-point. Higher rate of EAs |
| Erlotinib (EGFR), Zhu et al[14], 2006 | n = 720, BCLC B-C, ECOG 0-1, Child Pugh A/B | RCT Fase III. Superiority, Erlotinib + Sorafenib vs Placebo + Sorafenib | OS similar, TTP similar, Similar EAs |
| Linifanib (VEGF, PDGF), Cainap et al[27], 2015 | n = 1035, BCLC B-C, ECOG 0-1, Child Pugh A/B | RCT Fase III. Superiority, Linifanib vs Sorafenib | Failed to reach its primary end-point. TTP better for linifanib, Similar EAs |
| Tigatuzumab, Bruix et al[30], 2017 | n = 162, BCLC B-C, ECOG 0-1, Child Pugh A/B | RCT Fase II, Tigatuzumab + Sorafenib vs Placebo + Soraf | Safety profile adequate but no better TTP and OS |
| Dovitinib (VEGF, FGF, PDGF), Cheng et al[28], 2016 | n = 165, BCLC B-C, ECOG 0-1, Child Pugh A/B | RCT Fase II. Dovitinib vs Sorafenib | OS non superior, TTP similar, Higher rate of EAs |
| Bevacizumab (Ab VEGF), Hubbard et al[29], 2016 | n = 17, BCLC B-C, ECOG 0-1, Child Pugh A/B | RCT Fase I/II, Bevacizumab + Sorafenib | Higher rate of EAs, Excessive toxicity |
BCLC: Barcelona Clinic Liver Cancer; ECOG: Eastern Cooperative Oncology Group; EGFR: Endothelial growth factor; FGF: Fibroblast growth factor; OS: Overall survival; PDGF: Platelet-derived growth factor inhibitor; TTP: Time to progression; VEGF: Vascular-endothelial growth factor; RCT: Randomized clinical trials.
The only pre-treatment sorafenib predictors of better survival are the absence of extrahepatic disease, hepatitis C as an underlying disease and a low neu-trophil/leukocyte ratio[30]. High serum Alpha-fetoprotein (AFP) values (> 200 ng/mL) and macroscopic vascular invasion are baseline variables associated with poor prognosis in these patients, but even in these subgroups, sorafenib showed a survival benefit vs placebo[30].
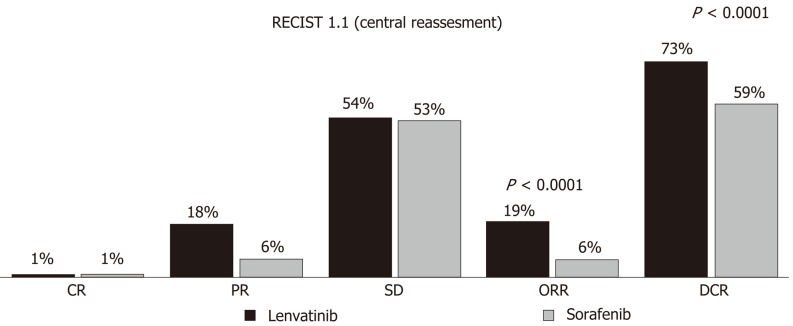
Results of a phase II and then a phase III RCT (REFLECT trial), have shown that lenvatinib, a VEGF receptors 1-3, FGF receptors 1-4 and PDGF α receptor inhibitor, was the first agent achieving non-inferiority against sorafenib[31,32]. The eligibility criteria in the REFLECT study were different from SHARP and Asia-Pacific studies, i.e., excluding those patients with main portal trunk tumor invasion and those subjects with intrahepatic tumor involvement of more than 50% of total liver volume[32]. The REFLECT study was an open-labeled phase 3 RCT, in which the primary objective was non-inferiority survival with respect to sorafenib (upper HR confidence interval limit of 1.08)[32]. In the intention-to-treat analysis, patients with lenvatinib presented a median survival of 13.6 mo, whereas those in the sorafenib arm had a median survival of 12.3 mo (HR: 0.92, 95%CI: 0.79-1.06). Likewise, a better progression-free survival (PFS) and TTP were observed, together with a higher ORR for lenvatinib over sorafenib (Figure 2).
Figure 2.
Radiological tumor response between sorafenib and lenvatinib according to RECIST 1.1 criteria, reported in the REFLECT trial. RECIST: Response Evaluation Criteria for Solid Tumors; ORR: Objective response rate.
Although this study demonstrated that lenvatinib is an effective first-line treatment option for advanced HCC, there are some important points to be considered. First, the non-inferiority design should have been characterized by less toxicity rates with lower discontinuation rates due to AEs as a co-primary end-point. However, these events were not included as co-primary end-points[32]. Second, the non-blinded design might have generated a possible intervention bias, justifying the longer treatment duration in lenvatinib arm (median treatment duration of 5.7 mo) compared to sorafenib arm (median treatment duration of 3.7 mo)[32]. Thus, if there was a similar tolerance between groups, this observation is striking and can only be explained by the design. Treatment duration with sorafenib was shorter, even when compared with previous RCT[3,4] and there was not a significant difference regarding treatment discontinuation rates between both arms. Consequently, the effect upon survival might have been biased due to a premature sorafenib interruption. Indeed, a higher incidence of severe AEs were observed in the lenvatinib arm (57% vs 49%)[32]. Lenvatinib was characterized by a higher incidence of arterial hypertension, proteinuria, dysphonia and hypothyroidism, while diarrhea, hand-foot reaction and alopecia were more frequent with sorafenib. However, this is opposed to the fact that lenvatinib showed higher tumor shrinkage rates[32]. Moreover, the adoption of different second line drugs (that subsequently revealed to be effective) following sorafenib and lenvatinib, might have influenced the post-progression overall survival.
The REFLECT trial modifies the future therapeutic options in patients with advanced HCC. It remains unclear which subgroup of patients will benefit more with one drug or another, as well as what will be the drug of choice for second line after tumor progression with lenvatinib. Thus, the appropriate selection of each treatment should be individualized.
More recently, immunotherapy has evolved as a potential first line systemic option. From a previous phase Ib-II trial escalating-dose, nivolumab (3 mg/kg every 2 wk-schedule) showed promising tumor responses in sorafenib-experienced patients[33]. These results leaded to perform a phase III RCT, in which nivolumab was tested against sorafenib in the first-line setting (Check-Mate 459 study; NCT02576509). Unfortunately, results were negative for both co-primary end-points of OS [16.4 mo (95%CI: 13.9-18.4) vs 14.7 mo (95%CI: 11.9-117.2), P = 0.0752] and PFS [3.7 mo (95%CI: 3.1-3.9) vs 3.8 mo (95%CI: 3.7-4.5)].
These negative results have been recently counterbalanced by positive results of a phase III, open-label, randomized trial evaluating the combination of atezolizumab, another immune-checkpoint inhibitor, with bevacizumab, an anti-VEGF monoclonal antibody, compared to sorafenib. Eligibility criteria included preserved liver function, advanced HCC, ECOG 0-1 in the absence of main portal trunk invasion and immunological disorders. Both co-primary end-points, OS HR 0.58 (CI: 0.42-0.79) [median survival not reached vs 13.2 mo with sorafenib alone, P = 0.0006] and PFS HR 0.59 (CI: 0.47-0.76; P < 0.0001) were longer for the new treatment combination (NCT03434379; IMbrave150 study). A significant higher ORR rate in the combination arm 27% vs 12% and DCR of 74% vs 55% (P < 0.0001) were observed. Similar incidence of all grade adverse events and a lower incidence of grades 3/4 related adverse events were observed with the combination arm (36% vs 46%). The most frequent adverse events were systemic hypertension, diarrhea, proteinuria, hyporexia, elevated liver enzymes and infusional reaction. However, treatment discontinuation was higher in atezolizumab + bevacizumab arm (16% and 10%, respectively) These results opened a new and potentially unlimited therapeutic options and are currently being studied in several phase-3 trials.
SECOND LINE SYSTEMIC TREATMENT: WHEN AND TO WHOM?
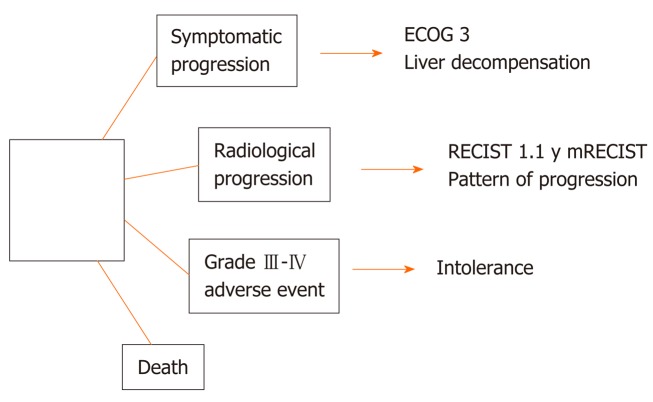
Three potential scenarios can develop during first line systemic treatment, which determine the subsequent patients’ management: (1) Tolerance or intolerance; (2) Radiological progression; and (3) Symptomatic progression (Figure 3).
Figure 3.
Clinical “stopping rules” of first and second line tyrosine kinase inhibitors. RECIST: Response Evaluation Criteria for Solid Tumors; ECOG: Eastern Cooperative Oncology Group; RECIST: Response Evaluation Criteria for Solid Tumors criteria.
Tolerance has been defined and applied as eligibility criteria in second line phase III RCTs after sorafenib treatment. In the RESORCE trial, tolerance was defined according to a specific time-dosing schedule as ≥ 400 mg during at least 20 d of the last 28 d under sorafenib[34]. In another trial, this definition was focused on the severity of adverse events, its complete resolution and no recurrence after reintroduction of sorafenib[35]. Consequently, tolerance or intolerance have been differently defined in RCT, focusing on the dosing-scheme or based on AEs severity. These clinical definitions are important to systematize the decision-making process in the daily practice.
The concept of radiological tumor progression has been focused during the last decade. As previously discussed, sorafenib granted an OS benefit even without tumor shrinkage[3,4]. On the other hand, TTP has failed to be a surrogate marker of survival benefit in HCC. For this reason, the reliability of TTP as a survival predictor is questionable in HCC, eventually other measures like disease free survival should be taken into account. Several examples have been published showing a benefit in TTP without any significant improvement in OS[36,37]. Thus, it seems that TTP does not accurately correlate with OS in advanced HCC. TTP might be exposed to several bias. Tumor progression can be evaluated by RECIST 1.1 or modified RECIST criteria for HCC (mRECIST)[38]. It should be noted that there might be some inconsistencies defining new lesions between both criteria. Moreover, RECIST 1.1 is more stringent than mRECIST when defining partial and complete responses and mRECIST could be more difficult to assess under heterogeneous tumor enhancement areas.
Radiological tumor defines eligibility for second-line treatment. However, radiological tumor progression can be distinguished in four different patterns with a different impact on OS[39,40]. The key clinical question is when to move to second line treatment under tumor progression in a patient tolerating treatment or even more strikingly, if during treatment the patient has shown clinical benefit hallmarks such as dermatological events[41]. A new intrahepatic lesion has a better prognosis than a new extrahepatic lesion or a new vascular invasion[39,40]. Therefore, second-line systemic treatment might be initiated under worst types of patterns of progression and may be delayed for a second progression in case of intrahepatic progression pattern.
Symptomatic progression is defined as progression beyond an ECOG PS 2[42]. Since most HCCs develop in patients with chronic liver disease, the conjunction of tolerability, treatment complications and risk of cirrhosis decompensation, make this cancer a huge therapeutic challenge. In the same patient, symptomatic progression might be due to cancer-related symptoms or those associated with liver disease decompensation. Therefore, in the same patient there may be “tumor radiological progression” or “untreatable progression” due to development of liver de-compensation as a competing event for OS[40].
Following systemic treatment, drug-related adverse events and complications due to liver disease should be evaluated at each visit, which will determine the need for dose reduction, transient or definitive suspension of the drug. These events define a patient as “intolerant” or “not a candidate” for second line treatment at all. This definition is important in the clinical practice since it defines not only who is potential candidate to start treatment with second-line drugs but also with which drug may be treated.
SECOND LINE COMPETITORS
Several clinical trials failed to show any benefit as 2nd line treatment option for advanced HCC in terms of OS when compared to placebo until the RESORCE study[34]. Brivanib (BRISK-PS, phase III RCT)[36], axitinib (phase II study)[43], everolimus (EVOLVE-1 phase III RCT)[44] and tivantinib[45] have all failed to show a benefit in OS vs placebo (Table 2). In particular, Tivantinib, a MET pathway inhibitor (hepatocyte growth factor blockade), had shown promising results in a phase II RCT[46]. However, a phase III study paradoxically turned negative, even in patients highly expressing MET mutation[45]. This RCT has shown the lack of utility of tumor biopsy as a predictor of the therapeutic response in HCC (c-MET), subsequently confirmed in the CHECKMATE 040 and KEYNOTE-240 studies with nivolumab and pem-brolizumab[33,35], where the expression on PD-1 in tumor tissue failed to predict treatment response.
Table 2.
Second line tyrosine kinase inhibitors approved for the treatment of advanced hepatocellular carcinoma
| Study drug | Population | Design-intervention | Results |
| Regorafenib, Bruix et al[34], 2017, resorce | n = 553, BCLC B-C, ECOG 0-1, Child Pugh A, SOR-Tolerant | RCT phase III. Superiority. Regorafenib vs placebo | OS HR 0.63 (CI: 0.50-0.79), ORR 11%, DCR 65% (mRECIST) |
| Cabozantinib, Abou-Alfa et al[47], Celestial | n = 707, BCLC B-C, ECOG 0-1, Child Pugh A, 1-2 prior systemic treatment, SOR-Tolerant/intolerant | RCT phase III. Superiority. Cabozantinib vs placebo | OS HR 0.76 (CI: 0.63-0.93), ORR 4%, DCR 64% (RECIST 1.1) |
| Ramucirumab, Zhu et al[48], reach I-II | n = 542, BCLC B-C, ECOG 0-1, Child Pugh A, AFP ≥ 400 ng/mL, SOR-Tolerant/intolerant | RCT phase III. Superiority. Ramucirumab vs placebo | OS HR 0.69 (CI: 0.57-0.84), ORR 5%, DCR 60%, (RECIST 1.1) |
Comparison across studies should cautiously analyzed. BCLC: Barcelona Clinic Liver Cancer; ECOG: Eastern Cooperative Oncology Group; OS: Overall survival; HR: Hazard ratio; SOR: Sorafenib; ORR: Objective response rate; RCT: Randomized clinical trials; DCR: Disease control rate; AFP: Alpha-fetoprotein.
Currently, regorafenib[34], cabozantinib (CELESTIAL phase III RCT)[47] and ramucirumab (REACH I and REACH II phase III RCTs)[48] have demonstrated second-line efficacy. A controversial issue has raised with pembrolizumab regarding statistical and clinical results of the KEYNOTE-224 RCT. Although the trial was negative according to its pre-established primary efficacy end-points, it showed a survival benefit that promoted its acceptance as a new second line systemic option[35]. On the other hand, nivolumab can be used as a second line option–at least in United States, following positive results of the uncontrolled phase I/II CHECK MATE 040 trial[33].
ANTI-TYROSIN KINASE INHIBITORS FOR SECOND LINE THERAPY
Both sorafenib and regorafenib are TKIs, but regorafenib is more active on VEGF, produces more intense inhibition on c-KIT receptor and partially blocks the TIE2 receptor[49]. The RESORCE phase III RCT included patients with advanced HCC who were tolerant and progressed under treatment with sorafenib[34]. The randomization was stratified 2:1 according to AFP values > 400 ng/mL, presence of macrovascular invasion, extrahepatic spread and ECOG 0-1. The median OS was 10.6 mo (CI: 9.1; 12.1) for regorafenib and 7.8 mo (CI 6.3; 8.8) for placebo, with a HR of 0.62 (95%CI: 0.50-0.79)[34]. Likewise, regorafenib presented a benefit over TTP, with an ORR of 11% and a DCR of 65%; evaluated through both RECIST 1.1 and mRECIST. In post-hoc analyzes, regorafenib presented an OS benefit in all clinical scenarios including patients with baseline worst prognosis[34]. Overall, 93% of the patients receiving regorafenib presented AEs (i.e., high blood pressure, fatigue, diarrhea and hand–foot reaction), 46% grade III and 4% grade IV, with drug discontinuation due to intolerance in 10% of the patients[34] (Table 3).
Table 3.
Scheme dose, adverse events and discontinuation rate of first and second line tyrosine kinase inhibitors and anti-vascular-endothelial growth factor agents approved for the treatment of advanced hepatocellular carcinoma
| Study drug | Dose reduction - interruption | Discontinuation rate |
| Sorafenib | 26% dose reduction (any AE), 44% drug interruption (any AE), most frequent AE leading to dose reductions: diarrhea, hand-foot skin reaction and rash | 11% |
| Lenvatinib | 37% dose reduction (related-AE), 40% drug interruption (related-AE), Most frequent AE leading to dose reductions: not reported | 9% |
| Regorafenib | 68% dose reduction or drug interruption (any AE), most frequent AE leading to dose reductions: diarrhea, hand-foot skin reaction | 10% |
| Cabozantinib | 62% dose reduction or drug interruption (any AE), most frequent AE leading to dose reductions: diarrhea, hand-foot skin reaction | 16% |
| Ramucirumab | 34% dose reduction or drug interruption (any AE), most frequent AE leading to dose reductions: fatigue, peripheral edema, hypertension and anorexia | 11% |
Comparison across studies should cautiously analyzed. AE: Adverse event.
Cabozantinib has been recently approved by both EMA and FDA as another second line treatment option. The phase III CELESTIAL RCT of cabozantinib 60 mg/d showed positive results vs placebo for OS [HR: 0.76 (CI: 0.63; 0.93); P = 0.005] and disease free survival [HR: 0.44 (CI: 0.36; 0.52)][47]. Cabozantinib, initially considered a dual VEGFR-2 and c-MET inhibitor, subsequently showed activity on MET, AXL, RET, FLT3 and Tie-2 pathways[50]. The CELESTIAL study included patients with advanced HCC, Child Pugh A, ECOG PS 0-1, with up to two previous systemic treatments, including sorafenib prior exposure, independently from tolerance. Patients were stratified according to etiology of liver disease (HBV or HCV), presence of macrovascular invasion, extrahepatic spread and world region and were randomized 2:1. The OS was 10.2 mo (CI: 9.1-12.0) for cabozantinib and 8 mo (CI: 6.8-9.4) for placebo. Cabozantinib presented lower TTP, with an ORR of 4%, SD of 60% and a DCR of 64%[47]. Dose reductions and discontinuations were more common in the cabozantinib arm, as were AEs (Table 3). No data have been reported in the post-hoc analysis regarding the effect of cabozantinib according to sorafenib tolerance, while cabozaninib showed higher survival than placebo with a median survival of 11.3 mo vs 7.2 mo [HR: 0.74 (CI: 0.59-0.92] among patients receiving sorafenib as the single prior systemic therapy[47].
OTHER ANTIANGIOGENIC AGENTS FOR SECOND LINE THERAPY
Prior studies have shown that AFP values are associated with worst OS in patients with advanced HCC and correlate with VEGF pathways, a critical role in angiogenesis. The anti-VEGF monoclonal antibody, ramucirumab, has been initially tested in second line treatment (whether sorafenib tolerant or not) in two phase III RCTs[48,51]. In the REACH I study, there was not a significant difference in OS[51]. However, from a post hoc analysis, ramucirumab showed better OS when compared to placebo in patients with AFP values equal or higher than 400 ng/mL[51]. This led to the design of the REACH II trial, which included patients with advanced HCC with AFP values ≥ 400 ng/mL who were intolerant or progressed under sorafenib[48]. This study confirmed that ramucirumab reduced the risk of death by 29%, with a median OS of 8.5 mo vs 7.3 mo for the placebo group [HR of 0.71 (95%CI: 0.53-0.95)]. Moreover, a better TTP was observed with an ORR and DCR of 5% and 60%, respectively. Ramucirumab was associated with a higher incidence of AEs, mainly hyponatremia and arterial hypertension (Table 3). This study was the first one showing efficacy based on a specific biomarker.
IMMUNOTHERAPY IN SECOND LINE THERAPY
Immunotherapy in HCC has been initially explored as second line options in patients with post-sorafenib tumor progression (tolerant or intolerant). Tremelimumab (anti-CTLA4) has been explored in an uncontrolled phase II exploratory trial in HCV+ patients following at least one prior systemic treatment[52]. The CheckMate 040 study, a phase I/II uncontrolled trial, evaluated nivolumab (anti PD-1) dose expansion and escalation scheme in patients with advanced HCC, Child Pugh A or B[33]. There was a promising ORR of 20%, with 3 complete responses (CR) and a DCR of 64%. The 9-mo survival rate was 74% (CI: 67%-79%). Baseline tumor levels of PD-L1 expression did not impact overall responses. The most common adverse effects observed were rash, elevation of liver and pancreatic enzymes and pruritus. Immunological adverse events were reported in less than 10% of the patients. This led to its temporary approval by the FDA in the United States as a second-line treatment option.
Finally, the KEYNOTE-224 (NCT02702401) phase III RCT compared the anti-PD1 pembrolizumab vs placebo for patients with advanced HCC, with tumor progression or intolerant to prior treatment with sorafenib[35]. Included patients had advanced HCC without main portal trunk tumor invasion, ECOG PS 0-1 and preserved liver function and were stratified according to baseline AFP values > 200 ng/mL, ECOG 0-1 and world region. The trial did not meet its primary efficacy end-points (OS and PFS). However, median OS was longer for pembrolizumab (13.9 mo) vs placebo (10.6 mo) with a HR of 0.78 (CI: 0.61-0.99); P = 0.024. The upper limit of the CI almost crossed the line of no effect as proposed by the null hypothesis with an expected statistical significance of P = 0.017. Thus, this was the reason for this negative trial, although there was a higher ORR (18.8% vs 4.4%) and DCR (62% vs 53%). Most common treatment-related AEs were pruritus in 13%, fatigue 10%, increased liver function tests 9%, diarrhea 8% and rash 8%. Immune-mediated adverse events were reported in 18% of the patients with pembrolizumab, 7.2% being grade 3 or 4. However, OS was longer in pembrolizumab arm vs placebo when survival was adjusted for subsequent anticancer therapies (13.9 vs 9.3 mo; HR: 0.67; CI: 0.48-0.92; P = 0.0066) or a two-stage survival analysis model (10.6 vs 7.6 mo; HR: 0.68; CI: 0.53-0.86; P = 0.0011).
FIRST AND SECOND LINE SEQUENTIAL TREATMENT
A post-hoc retrospective analysis of the RESORCE trial evaluated the effect on survival of the sequential treatment of first and second line treatment with sorafenib-regorafenib: The sequential treatment granted 26 mo of median overall survival compared to 19.2 mo for the patients treated by sorafenib and placebo thereafter[53]. Sixty percent of the study population had a prior last sorafenib dose of 800 mg/d. Regorafenib was effective regardless the last treatment dose of sorafenib (full dose vs lower dose) but patients with lower doses of sorafenib presented higher rates of hand-foot skin reaction, fatigue and anorexia when compared to placebo. Thus, caution should be taken when treating patients who were tolerant to lower doses of sorafenib after initiation of regorafenib.
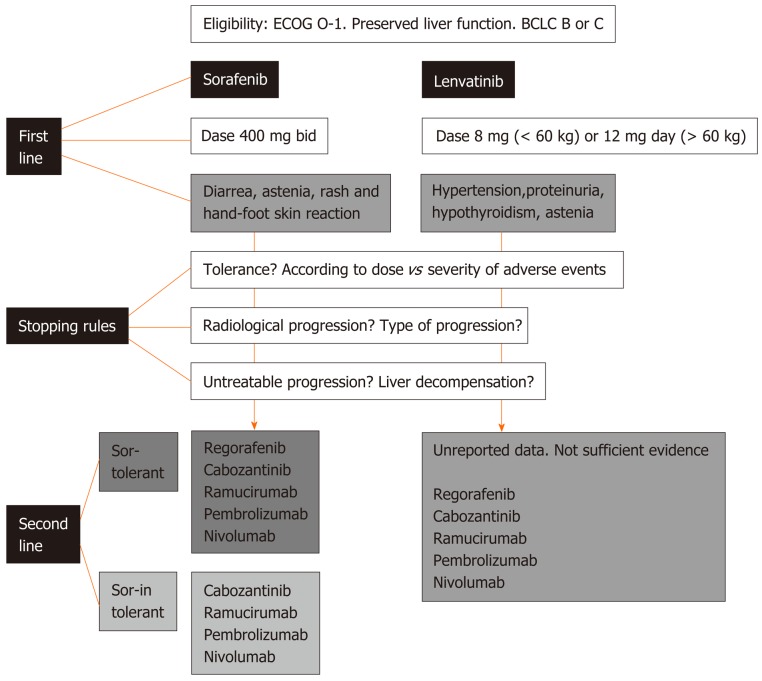
Other data regarding sequential treatment of sorafenib-other TKIs are lacking, however data on sequential use of lenvatinib and sorafenib will be soon available by the post-hoc analysis of the REFLECT trial in those patients treated with sorafenib after lenvatinib discontinuation (Figure 4).
Figure 4.
Flow chart for clinical-decision making processes of first and second line systemic treatment for advanced hepatocellular carcinoma. BCLC: Barcelona Clinic Liver Cancer; ECOG: Eastern Cooperative Oncology Group.
SEQUENTIAL SYSTEMIC TREATMENT IN SPECIAL POPULATIONS
A special population excluded from RCT are patients with recurrent HCC following liver transplantation. The effect of sorafenib was reported in retrospective cohort studies with similar outcomes regarding survival and tolerability[54]. More recently, a retrospective cohort study including 28 patients evaluated the sequential therapy of sorafenib-regorafenib in this setting[55]. During regorafenib all patients had at least one adverse event, the most common grade 3/4 adverse events were fatigue and hand-foot skin reaction. Interaction between CYP3A4 metabolism was reported with higher plasma levels of immunosuppressive drugs increased. Median OS from regorafenib initiation was 12.9 (CI: 6.7-19.1 mo) and 38.4 mo (CI: 18.5-58.4 mo) from sorafenib initiation.
CONCLUSION
Atezolizumab plus bevacizumab may be the future standard of care over in first-line. However, some patients may be still be treated with with sorafenib or lenvatinib, particularly those patients with immunotherapy contraindication or main portal trunk invasion (not for lenvatinib). Both are equivalent, except for the orphan-based evidence of sequential post-lenvatinib treatment for second line. Sorafenib-regorafenib sequencing therapy has opened a new paradigm with a life expectancy exceeding two years at least for those patients tolerant for sorafenib. This data being previously unthinkable 10 years ago. Other therapeutic options for second line treatment include cabozantinib (for both sorafenib-tolerant and intolerant patients) and ramucirumab (only for patients with AFP values ≥ 400 ng/mL). While some regulatory agencies have approved the use of immunotherapy even after failing trials (i.e., nivolumab and pembrolizumab), the identification of patients who could benefit from one or another option is still unclear. Other trials, either in first and second lines are being tested, with combination of immunotherapy plus TKIs, showing positive preliminary results. Further predictive biomarkers of treatment response are needed in order to better select patients for each specific treatment.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Argentina
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: There is no conflict of interest associated with any of the senior author or other coauthors contributed their efforts in this manuscript.
Peer-review started: December 28, 2019
First decision: January 11, 2020
Article in press: April 4, 2020
P-Reviewer: Kao JT, Kohla MA, Suda T, Yang L S-Editor: Zhang L L-Editor: A E-Editor: Zhang YL
Contributor Information
Federico Piñero, Hospital Universitario Austral, Facultad de Ciencias Biomédicas, Universidad Austral, Buenos Aires B1629HJ, Argentina; Latin American Liver Research Educational and Awareness Network, Buenos Aires B1629HJ, Argentina. fpinerof@cas.austral.edu.ar.
Marcelo Silva, Hospital Universitario Austral, Facultad de Ciencias Biomédicas, Universidad Austral, Buenos Aires B1629HJ, Argentina; Latin American Liver Research Educational and Awareness Network, Buenos Aires B1629HJ, Argentina.
Massimo Iavarone, Division of Gastroenterology and Hepatology, CRC “A.M. e A. Migliavacca” Center for the Study of Liver Disease, University of Milan, Fondazione IRCCS Ca’ Granda Maggiore Hospital, Milan 20121, Italy.
References
- 1.Global Burden of Disease Liver Cancer Collaboration. Akinyemiju T, Abera S, Ahmed M, Alam N, Alemayohu MA, Allen C, Al-Raddadi R, Alvis-Guzman N, Amoako Y, Artaman A, Ayele TA, Barac A, Bensenor I, Berhane A, Bhutta Z, Castillo-Rivas J, Chitheer A, Choi JY, Cowie B, Dandona L, Dandona R, Dey S, Dicker D, Phuc H, Ekwueme DU, Zaki MS, Fischer F, Fürst T, Hancock J, Hay SI, Hotez P, Jee SH, Kasaeian A, Khader Y, Khang YH, Kumar A, Kutz M, Larson H, Lopez A, Lunevicius R, Malekzadeh R, McAlinden C, Meier T, Mendoza W, Mokdad A, Moradi-Lakeh M, Nagel G, Nguyen Q, Nguyen G, Ogbo F, Patton G, Pereira DM, Pourmalek F, Qorbani M, Radfar A, Roshandel G, Salomon JA, Sanabria J, Sartorius B, Satpathy M, Sawhney M, Sepanlou S, Shackelford K, Shore H, Sun J, Mengistu DT, Topór-Mądry R, Tran B, Ukwaja KN, Vlassov V, Vollset SE, Vos T, Wakayo T, Weiderpass E, Werdecker A, Yonemoto N, Younis M, Yu C, Zaidi Z, Zhu L, Murray CJL, Naghavi M, Fitzmaurice C. The Burden of Primary Liver Cancer and Underlying Etiologies From 1990 to 2015 at the Global, Regional, and National Level: Results From the Global Burden of Disease Study 2015. JAMA Oncol. 2017;3:1683–1691. doi: 10.1001/jamaoncol.2017.3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruix J, da Fonseca LG, Reig M. Insights into the success and failure of systemic therapy for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2019;16:617–630. doi: 10.1038/s41575-019-0179-x. [DOI] [PubMed] [Google Scholar]
- 3.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 4.Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 5.European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, Zhu AX, Murad MH, Marrero JA. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358–380. doi: 10.1002/hep.29086. [DOI] [PubMed] [Google Scholar]
- 7.Marrero JA, Kudo M, Venook AP, Ye SL, Bronowicki JP, Chen XP, Dagher L, Furuse J, Geschwind JH, de Guevara LL, Papandreou C, Takayama T, Sanyal AJ, Yoon SK, Nakajima K, Lehr R, Heldner S, Lencioni R. Observational registry of sorafenib use in clinical practice across Child-Pugh subgroups: The GIDEON study. J Hepatol. 2016;65:1140–1147. doi: 10.1016/j.jhep.2016.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Iavarone M, Cabibbo G, Piscaglia F, Zavaglia C, Grieco A, Villa E, Cammà C, Colombo M SOFIA (SOraFenib Italian Assessment) study group. Field-practice study of sorafenib therapy for hepatocellular carcinoma: a prospective multicenter study in Italy. Hepatology. 2011;54:2055–2063. doi: 10.1002/hep.24644. [DOI] [PubMed] [Google Scholar]
- 9.Piñero F, Marciano S, Fernández N, Silva J, Anders M, Zerega A, Ridruejo E, Romero G, Ameigeiras B, D'Amico C, Gaite L, Bermúdez C, Reggiardo V, Colombato L, Gadano A, Silva M. Intermediate-advanced hepatocellular carcinoma in Argentina: Treatment and survival analysis. World J Gastroenterol. 2019;25:3607–3618. doi: 10.3748/wjg.v25.i27.3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yeo W, Mok TS, Zee B, Leung TW, Lai PB, Lau WY, Koh J, Mo FK, Yu SC, Chan AT, Hui P, Ma B, Lam KC, Ho WM, Wong HT, Tang A, Johnson PJ. A randomized phase III study of doxorubicin versus cisplatin/interferon alpha-2b/doxorubicin/fluorouracil (PIAF) combination chemotherapy for unresectable hepatocellular carcinoma. J Natl Cancer Inst. 2005;97:1532–1538. doi: 10.1093/jnci/dji315. [DOI] [PubMed] [Google Scholar]
- 11.Gish RG, Porta C, Lazar L, Ruff P, Feld R, Croitoru A, Feun L, Jeziorski K, Leighton J, Gallo J, Kennealey GT. Phase III randomized controlled trial comparing the survival of patients with unresectable hepatocellular carcinoma treated with nolatrexed or doxorubicin. J Clin Oncol. 2007;25:3069–3075. doi: 10.1200/JCO.2006.08.4046. [DOI] [PubMed] [Google Scholar]
- 12.Abou-Alfa GK, Johnson P, Knox JJ, Capanu M, Davidenko I, Lacava J, Leung T, Gansukh B, Saltz LB. Doxorubicin plus sorafenib vs doxorubicin alone in patients with advanced hepatocellular carcinoma: a randomized trial. JAMA. 2010;304:2154–2160. doi: 10.1001/jama.2010.1672. [DOI] [PubMed] [Google Scholar]
- 13.Qin S, Bai Y, Lim HY, Thongprasert S, Chao Y, Fan J, Yang TS, Bhudhisawasdi V, Kang WK, Zhou Y, Lee JH, Sun Y. Randomized, multicenter, open-label study of oxaliplatin plus fluorouracil/leucovorin versus doxorubicin as palliative chemotherapy in patients with advanced hepatocellular carcinoma from Asia. J Clin Oncol. 2013;31:3501–3508. doi: 10.1200/JCO.2012.44.5643. [DOI] [PubMed] [Google Scholar]
- 14.Zhu AX, Blaszkowsky LS, Ryan DP, Clark JW, Muzikansky A, Horgan K, Sheehan S, Hale KE, Enzinger PC, Bhargava P, Stuart K. Phase II study of gemcitabine and oxaliplatin in combination with bevacizumab in patients with advanced hepatocellular carcinoma. J Clin Oncol. 2006;24:1898–1903. doi: 10.1200/JCO.2005.04.9130. [DOI] [PubMed] [Google Scholar]
- 15.Louafi S, Boige V, Ducreux M, Bonyhay L, Mansourbakht T, de Baere T, Asnacios A, Hannoun L, Poynard T, Taïeb J. Gemcitabine plus oxaliplatin (GEMOX) in patients with advanced hepatocellular carcinoma (HCC): results of a phase II study. Cancer. 2007;109:1384–1390. doi: 10.1002/cncr.22532. [DOI] [PubMed] [Google Scholar]
- 16.Asnacios A, Fartoux L, Romano O, Tesmoingt C, Louafi S S, Mansoubakht T, Artru P, Poynard T, Rosmorduc O, Hebbar M, Taieb J. Gemcitabine plus oxaliplatin (GEMOX) combined with cetuximab in patients with progressive advanced stage hepatocellular carcinoma: results of a multicenter phase 2 study. Cancer. 2008;112:2733–2739. doi: 10.1002/cncr.23489. [DOI] [PubMed] [Google Scholar]
- 17.Zaanan A, Williet N, Hebbar M, Dabakuyo TS, Fartoux L, Mansourbakht T, Dubreuil O, Rosmorduc O, Cattan S, Bonnetain F, Boige V, Taïeb J. Gemcitabine plus oxaliplatin in advanced hepatocellular carcinoma: a large multicenter AGEO study. J Hepatol. 2013;58:81–88. doi: 10.1016/j.jhep.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Liu Y, Yue H, Xu S, Wang F, Ma N, Li K, Qiao L, Wang J. First-line gemcitabine and oxaliplatin (GEMOX) plus sorafenib, followed by sorafenib as maintenance therapy, for patients with advanced hepatocellular carcinoma: a preliminary study. Int J Clin Oncol. 2015;20:952–959. doi: 10.1007/s10147-015-0796-5. [DOI] [PubMed] [Google Scholar]
- 19.Assenat E, Pageaux GP, Thézenas S, Peron JM, Bécouarn Y, Seitz JF, Merle P, Blanc JF, Bouché O, Ramdani M, Poujol S, de Forges H, Ychou M, Boige V. Sorafenib alone vs. sorafenib plus GEMOX as 1st-line treatment for advanced HCC: the phase II randomised PRODIGE 10 trial. Br J Cancer. 2019;120:896–902. doi: 10.1038/s41416-019-0443-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boige V, Raoul JL, Pignon JP, Bouché O, Blanc JF, Dahan L, Jouve JL, Dupouy N, Ducreux M Fédération Francophone de Cancérologie Digestive. Multicentre phase II trial of capecitabine plus oxaliplatin (XELOX) in patients with advanced hepatocellular carcinoma: FFCD 03-03 trial. Br J Cancer. 2007;97:862–867. doi: 10.1038/sj.bjc.6603956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsu CH, Yang TS, Hsu C, Toh HC, Epstein RJ, Hsiao LT, Chen PJ, Lin ZZ, Chao TY, Cheng AL. Efficacy and tolerability of bevacizumab plus capecitabine as first-line therapy in patients with advanced hepatocellular carcinoma. Br J Cancer. 2010;102:981–986. doi: 10.1038/sj.bjc.6605580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He M, Li Q, Zou R, Shen J, Fang W, Tan G, Zhou Y, Wu X, Xu L, Wei W, Le Y, Zhou Z, Zhao M, Guo Y, Guo R, Chen M, Shi M. Sorafenib Plus Hepatic Arterial Infusion of Oxaliplatin, Fluorouracil, and Leucovorin vs Sorafenib Alone for Hepatocellular Carcinoma With Portal Vein Invasion: A Randomized Clinical Trial. JAMA Oncol. 2019;5:953–960. doi: 10.1001/jamaoncol.2019.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kudo M, Ueshima K, Yokosuka O, Ogasawara S, Obi S, Izumi N, Aikata H, Nagano H, Hatano E, Sasaki Y, Hino K, Kumada T, Yamamoto K, Imai Y, Iwadou S, Ogawa C, Okusaka T, Kanai F, Akazawa K, Yoshimura KI, Johnson P, Arai Y SILIUS study group. Sorafenib plus low-dose cisplatin and fluorouracil hepatic arterial infusion chemotherapy versus sorafenib alone in patients with advanced hepatocellular carcinoma (SILIUS): a randomised, open label, phase 3 trial. Lancet Gastroenterol Hepatol. 2018;3:424–432. doi: 10.1016/S2468-1253(18)30078-5. [DOI] [PubMed] [Google Scholar]
- 24.Cheng AL, Kang YK, Lin DY, Park JW, Kudo M, Qin S, Chung HC, Song X, Xu J, Poggi G, Omata M, Pitman Lowenthal S, Lanzalone S, Yang L, Lechuga MJ, Raymond E. Sunitinib versus sorafenib in advanced hepatocellular cancer: results of a randomized phase III trial. J Clin Oncol. 2013;31:4067–4075. doi: 10.1200/JCO.2012.45.8372. [DOI] [PubMed] [Google Scholar]
- 25.Johnson PJ, Qin S, Park JW, Poon RT, Raoul JL, Philip PA, Hsu CH, Hu TH, Heo J, Xu J, Lu L, Chao Y, Boucher E, Han KH, Paik SW, Robles-Aviña J, Kudo M, Yan L, Sobhonslidsuk A, Komov D, Decaens T, Tak WY, Jeng LB, Liu D, Ezzeddine R, Walters I, Cheng AL. Brivanib versus sorafenib as first-line therapy in patients with unresectable, advanced hepatocellular carcinoma: results from the randomized phase III BRISK-FL study. J Clin Oncol. 2013;31:3517–3524. doi: 10.1200/JCO.2012.48.4410. [DOI] [PubMed] [Google Scholar]
- 26.Zhu AX, Rosmorduc O, Evans TR, Ross PJ, Santoro A, Carrilho FJ, Bruix J, Qin S, Thuluvath PJ, Llovet JM, Leberre MA, Jensen M, Meinhardt G, Kang YK. SEARCH: a phase III, randomized, double-blind, placebo-controlled trial of sorafenib plus erlotinib in patients with advanced hepatocellular carcinoma. J Clin Oncol. 2015;33:559–566. doi: 10.1200/JCO.2013.53.7746. [DOI] [PubMed] [Google Scholar]
- 27.Cainap C, Qin S, Huang WT, Chung IJ, Pan H, Cheng Y, Kudo M, Kang YK, Chen PJ, Toh HC, Gorbunova V, Eskens FA, Qian J, McKee MD, Ricker JL, Carlson DM, El-Nowiem S. Linifanib versus Sorafenib in patients with advanced hepatocellular carcinoma: results of a randomized phase III trial. J Clin Oncol. 2015;33:172–179. doi: 10.1200/JCO.2013.54.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheng AL, Thongprasert S, Lim HY, Sukeepaisarnjaroen W, Yang TS, Wu CC, Chao Y, Chan SL, Kudo M, Ikeda M, Kang YK, Pan H, Numata K, Han G, Balsara B, Zhang Y, Rodriguez AM, Zhang Y, Wang Y, Poon RT. Randomized, open-label phase 2 study comparing frontline dovitinib versus sorafenib in patients with advanced hepatocellular carcinoma. Hepatology. 2016;64:774–784. doi: 10.1002/hep.28600. [DOI] [PubMed] [Google Scholar]
- 29.Hubbard JM, Mahoney MR, Loui WS, Roberts LR, Smyrk TC, Gatalica Z, Borad M, Kumar S, Alberts SR. Phase I/II Randomized Trial of Sorafenib and Bevacizumab as First-Line Therapy in Patients with Locally Advanced or Metastatic Hepatocellular Carcinoma: North Central Cancer Treatment Group Trial N0745 (Alliance) Target Oncol. 2017;12:201–209. doi: 10.1007/s11523-016-0467-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruix J, Cheng AL, Meinhardt G, Nakajima K, De Sanctis Y, Llovet J. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: Analysis of two phase III studies. J Hepatol. 2017;67:999–1008. doi: 10.1016/j.jhep.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 31.Ikeda K, Kudo M, Kawazoe S, Osaki Y, Ikeda M, Okusaka T, Tamai T, Suzuki T, Hisai T, Hayato S, Okita K, Kumada H. Phase 2 study of lenvatinib in patients with advanced hepatocellular carcinoma. J Gastroenterol. 2017;52:512–519. doi: 10.1007/s00535-016-1263-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng AL. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163–1173. doi: 10.1016/S0140-6736(18)30207-1. [DOI] [PubMed] [Google Scholar]
- 33.El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, Meyer T, Kang YK, Yeo W, Chopra A, Anderson J, Dela Cruz C, Lang L, Neely J, Tang H, Dastani HB, Melero I. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, Gerolami R, Masi G, Ross PJ, Song T, Bronowicki JP, Ollivier-Hourmand I, Kudo M, Cheng AL, Llovet JM, Finn RS, LeBerre MA, Baumhauer A, Meinhardt G, Han G RESORCE Investigators. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56–66. doi: 10.1016/S0140-6736(16)32453-9. [DOI] [PubMed] [Google Scholar]
- 35.Zhu AX, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer D, Verslype C, Zagonel V, Fartoux L, Vogel A, Sarker D, Verset G, Chan SL, Knox J, Daniele B, Webber AL, Ebbinghaus SW, Ma J, Siegel AB, Cheng AL, Kudo M KEYNOTE-224 investigators. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19:940–952. doi: 10.1016/S1470-2045(18)30351-6. [DOI] [PubMed] [Google Scholar]
- 36.Llovet JM, Decaens T, Raoul JL, Boucher E, Kudo M, Chang C, Kang YK, Assenat E, Lim HY, Boige V, Mathurin P, Fartoux L, Lin DY, Bruix J, Poon RT, Sherman M, Blanc JF, Finn RS, Tak WY, Chao Y, Ezzeddine R, Liu D, Walters I, Park JW. Brivanib in patients with advanced hepatocellular carcinoma who were intolerant to sorafenib or for whom sorafenib failed: results from the randomized phase III BRISK-PS study. J Clin Oncol. 2013;31:3509–3516. doi: 10.1200/JCO.2012.47.3009. [DOI] [PubMed] [Google Scholar]
- 37.Vilgrain V, Pereira H, Assenat E, Guiu B, Ilonca AD, Pageaux GP, Sibert A, Bouattour M, Lebtahi R, Allaham W, Barraud H, Laurent V, Mathias E, Bronowicki JP, Tasu JP, Perdrisot R, Silvain C, Gerolami R, Mundler O, Seitz JF, Vidal V, Aubé C, Oberti F, Couturier O, Brenot-Rossi I, Raoul JL, Sarran A, Costentin C, Itti E, Luciani A, Adam R, Lewin M, Samuel D, Ronot M, Dinut A, Castera L, Chatellier G SARAH Trial Group. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. Lancet Oncol. 2017;18:1624–1636. doi: 10.1016/S1470-2045(17)30683-6. [DOI] [PubMed] [Google Scholar]
- 38.Lencioni R, Montal R, Torres F, Park JW, Decaens T, Raoul JL, Kudo M, Chang C, Ríos J, Boige V, Assenat E, Kang YK, Lim HY, Walters I, Llovet JM. Objective response by mRECIST as a predictor and potential surrogate end-point of overall survival in advanced HCC. J Hepatol. 2017;66:1166–1172. doi: 10.1016/j.jhep.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 39.Reig M, Rimola J, Torres F, Darnell A, Rodriguez-Lope C, Forner A, Llarch N, Ríos J, Ayuso C, Bruix J. Postprogression survival of patients with advanced hepatocellular carcinoma: rationale for second-line trial design. Hepatology. 2013;58:2023–2031. doi: 10.1002/hep.26586. [DOI] [PubMed] [Google Scholar]
- 40.Iavarone M, Cabibbo G, Biolato M, Della Corte C, Maida M, Barbara M, Basso M, Vavassori S, Craxì A, Grieco A, Cammà C, Colombo M. Predictors of survival in patients with advanced hepatocellular carcinoma who permanently discontinued sorafenib. Hepatology. 2015;62:784–791. doi: 10.1002/hep.27729. [DOI] [PubMed] [Google Scholar]
- 41.Díaz-González Á, Sanduzzi-Zamparelli M, Sapena V, Torres F, LLarch N, Iserte G, Forner A, da Fonseca L, Ríos J, Bruix J, Reig M. Systematic review with meta-analysis: the critical role of dermatological events in patients with hepatocellular carcinoma treated with sorafenib. Aliment Pharmacol Ther. 2019;49:482–491. doi: 10.1111/apt.15088. [DOI] [PubMed] [Google Scholar]
- 42.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655. [PubMed] [Google Scholar]
- 43.McNamara MG, Le LW, Horgan AM, Aspinall A, Burak KW, Dhani N, Chen E, Sinaei M, Lo G, Kim TK, Rogalla P, Bathe OF, Knox JJ. A phase II trial of second-line axitinib following prior antiangiogenic therapy in advanced hepatocellular carcinoma. Cancer. 2015;121:1620–1627. doi: 10.1002/cncr.29227. [DOI] [PubMed] [Google Scholar]
- 44.Zhu AX, Kudo M, Assenat E, Cattan S, Kang YK, Lim HY, Poon RT, Blanc JF, Vogel A, Chen CL, Dorval E, Peck-Radosavljevic M, Santoro A, Daniele B, Furuse J, Jappe A, Perraud K, Anak O, Sellami DB, Chen LT. Effect of everolimus on survival in advanced hepatocellular carcinoma after failure of sorafenib: the EVOLVE-1 randomized clinical trial. JAMA. 2014;312:57–67. doi: 10.1001/jama.2014.7189. [DOI] [PubMed] [Google Scholar]
- 45.Rimassa L, Assenat E, Peck-Radosavljevic M, Pracht M, Zagonel V, Mathurin P, Rota Caremoli E, Porta C, Daniele B, Bolondi L, Mazzaferro V, Harris W, Damjanov N, Pastorelli D, Reig M, Knox J, Negri F, Trojan J, López López C, Personeni N, Decaens T, Dupuy M, Sieghart W, Abbadessa G, Schwartz B, Lamar M, Goldberg T, Shuster D, Santoro A, Bruix J. Tivantinib for second-line treatment of MET-high, advanced hepatocellular carcinoma (METIV-HCC): a final analysis of a phase 3, randomised, placebo-controlled study. Lancet Oncol. 2018;19:682–693. doi: 10.1016/S1470-2045(18)30146-3. [DOI] [PubMed] [Google Scholar]
- 46.Santoro A, Rimassa L, Borbath I, Daniele B, Salvagni S, Van Laethem JL, Van Vlierberghe H, Trojan J, Kolligs FT, Weiss A, Miles S, Gasbarrini A, Lencioni M, Cicalese L, Sherman M, Gridelli C, Buggisch P, Gerken G, Schmid RM, Boni C, Personeni N, Hassoun Z, Abbadessa G, Schwartz B, Von Roemeling R, Lamar ME, Chen Y, Porta C. Tivantinib for second-line treatment of advanced hepatocellular carcinoma: a randomised, placebo-controlled phase 2 study. Lancet Oncol. 2013;14:55–63. doi: 10.1016/S1470-2045(12)70490-4. [DOI] [PubMed] [Google Scholar]
- 47.Abou-Alfa GK, Meyer T, Cheng AL, El-Khoueiry AB, Rimassa L, Ryoo BY, Cicin I, Merle P, Chen Y, Park JW, Blanc JF, Bolondi L, Klümpen HJ, Chan SL, Zagonel V, Pressiani T, Ryu MH, Venook AP, Hessel C, Borgman-Hagey AE, Schwab G, Kelley RK. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N Engl J Med. 2018;379:54–63. doi: 10.1056/NEJMoa1717002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhu AX, Kang YK, Yen CJ, Finn RS, Galle PR, Llovet JM, Assenat E, Brandi G, Pracht M, Lim HY, Rau KM, Motomura K, Ohno I, Merle P, Daniele B, Shin DB, Gerken G, Borg C, Hiriart JB, Okusaka T, Morimoto M, Hsu Y, Abada PB, Kudo M REACH-2 study investigators. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:282–296. doi: 10.1016/S1470-2045(18)30937-9. [DOI] [PubMed] [Google Scholar]
- 49.Bruix J, Tak WY, Gasbarrini A, Santoro A, Colombo M, Lim HY, Mazzaferro V, Wiest R, Reig M, Wagner A, Bolondi L. Regorafenib as second-line therapy for intermediate or advanced hepatocellular carcinoma: multicentre, open-label, phase II safety study. Eur J Cancer. 2013;49:3412–3419. doi: 10.1016/j.ejca.2013.05.028. [DOI] [PubMed] [Google Scholar]
- 50.Kelley RK, Verslype C, Cohn AL, Yang TS, Su WC, Burris H, Braiteh F, Vogelzang N, Spira A, Foster P, Lee Y, Van Cutsem E. Cabozantinib in hepatocellular carcinoma: results of a phase 2 placebo-controlled randomized discontinuation study. Ann Oncol. 2017;28:528–534. doi: 10.1093/annonc/mdw651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhu AX, Park JO, Ryoo BY, Yen CJ, Poon R, Pastorelli D, Blanc JF, Chung HC, Baron AD, Pfiffer TE, Okusaka T, Kubackova K, Trojan J, Sastre J, Chau I, Chang SC, Abada PB, Yang L, Schwartz JD, Kudo M REACH Trial Investigators. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2015;16:859–870. doi: 10.1016/S1470-2045(15)00050-9. [DOI] [PubMed] [Google Scholar]
- 52.Sangro B, Gomez-Martin C, de la Mata M, Iñarrairaegui M, Garralda E, Barrera P, Riezu-Boj JI, Larrea E, Alfaro C, Sarobe P, Lasarte JJ, Pérez-Gracia JL, Melero I, Prieto J. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J Hepatol. 2013;59:81–88. doi: 10.1016/j.jhep.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 53.Finn RS, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Gerolami R, Caparello C, Cabrera R, Chang C, Sun W, LeBerre MA, Baumhauer A, Meinhardt G, Bruix J. Outcomes of sequential treatment with sorafenib followed by regorafenib for HCC: Additional analyses from the phase III RESORCE trial. J Hepatol. 2018;69:353–358. doi: 10.1016/j.jhep.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 54.Sposito C, Mariani L, Germini A, Flores Reyes M, Bongini M, Grossi G, Bhoori S, Mazzaferro V. Comparative efficacy of sorafenib versus best supportive care in recurrent hepatocellular carcinoma after liver transplantation: a case-control study. J Hepatol. 2013;59:59–66. doi: 10.1016/j.jhep.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 55.Iavarone M, Invernizzi F, Czauderna C, Sanduzzi-Zamparelli M, Bhoori S, Amaddeo G, Manini MA, López MF, Anders M, Pinter M, Rodríguez MJB, Cristóbal MR, Soteras GA, Piñero F, Villadsen GE, Weinmann A, Crespo G, Mazzaferro V, Regnault H, Giorgio M, González-Diéguez ML, Donato MF, Varela M, Wörns MA, Bruix J, Lampertico P, Reig M. Preliminary experience on safety of regorafenib after sorafenib failure in recurrent hepatocellular carcinoma after liver transplantation. Am J Transplant. 2019;19:3176–3184. doi: 10.1111/ajt.15551. [DOI] [PubMed] [Google Scholar]