Abstract
Scrotal calcinosis is a rare benign pathology and its etiology is still discussed. The main complaint is mostly aesthetic. The treatment of extended forms is a one-staged excision. The aim of our study was to study clinical and anatomopathological aspects and report our surgical management of a case of diffuse scrotal calcinosis.
We report a case of 24-year-old patient who consulted for painless scrotal nodules lasting for 2 years. Scrotal calcinosis diagnostic was based on clinical examination. The treatment was a one-staged scrotal excision taking all nodules and the plasty of the scrotum. The diagnosis was confirmed by a histopathological examination of surgical specimen.
Keywords: Scrotal, Calcinosis, Idiopathic, Excision
Introduction
Scrotal calcinosis is a rare benign condition characterized by the presence of multiple calcified nodules on the scrotal skin. Despite many theories that have been developed over the years, its pathogenesis remains controversial. The discomfort is mainly aesthetic and the confirmation is obtained by histological examination. Treatment consists in surgical excision of the lesions for both diagnostic and therapeutic purposes.
We report a new case of idiopathic scrotal calcinosis in a 24-year-old patient that underwent complete surgical excision.
Observation
A 24-year-old male, with no medical history, was referred to our department with scrotal nodules that had gradually increased in size and number during the past two years. Physical examination revealed painless, multiple subcutaneous nodules within the scrotal wall that measured from 2 to 20 mm in diameter. There was no itching, no areas of ulceration or chalky discharge. The patient stated that he had never experienced any scrotal inflammatory disease or infection, or scrotal trauma. He had no history of metabolic disease.
No other lesions were discovered on the physical exam (Fig. 1).
Fig. 1.
Multiple white nodules involving scrotal skin.
Laboratory examinations, including serum calcium, phosphorus and parathyroid hormone levels were within normal range.
Based on the clinical examination, these lesions were diagnosed as scrotal calcinosis and we decided to perform a surgical excision under general anesthesia.
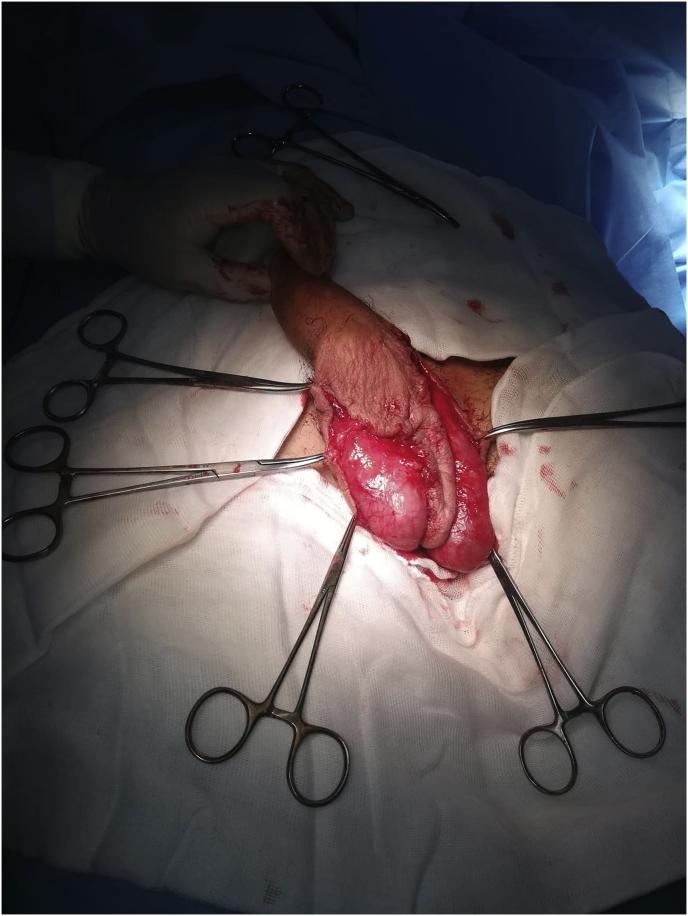
The procedure consisted in fine dissection between the dermis and the dartoic muscle to allow an excision of the involved scrotal skin, centered on the scrotal median raphe as scrotal lift shape. The defect was closed on both sides of the median raphe by interrupted sutures. (Fig. 2).
Fig. 2.
Per operative view: Scrotal skin defect.
The operative specimens included hard and thick-walled calcified nodules.
Histopathological examination confirmed the diagnosis of scrotal calcinosis.
Postoperative recovery was uneventful. The patient was discharged after 2 days on oral analgesics. Aesthetic result was satisfying and sexual quality of life was highly improved. No recurrence was encountered during 18 months of follow-up (Fig. 3).
Fig. 3.
Post-operative view of scrotal calcinosis treated by surgical excision.
Discussion
Idiopathic scrotal calcinosis is a rare and benign condition, first described by Lewinski in 1883.1 It involves the development of scrotal nodules in the skin and subcutaneous tissue. Despite of its benignity, the impact on the patient's quality of life can be very important.
It appears mainly in men aged 20–40 years old and it is more common among dark colored skin patients, suggesting an ethnic susceptibility.2 The diagnosis is often delayed, because of the indolent nature and the intimate localization of the nodules. The main complaint is an aesthetic issue, affecting the sexual life of the patient.
The pathogenesis of this entity remains unclear and controversial. Numerous theories have been proposed concerning its origin, whether the disease is idiopathic or the result of dystrophic calcification of preexistent epidermal inclusion cysts or if they have emerged de novo without any triggering metabolic condition, infiltration of foreign body material or induced by trauma.3 The calcification of preexistent epidermal cysts is the most suggested theory by many authors as a possible pathogenesis.4
Despite the controversy about the origin of this entity, surgery is the treatment of choice that provides excellent results.4 Surgical excision must be limited to the scrotal skin since the calcified nodules are limited to the dermis, leaving the dartos layer intact.5
Scrotal skin is characterized by high laxity. Hence, in case of diffuse scrotal calcinosis, a large cutaneous defect can be easily closed by interrupted sutures.5
Multi-staged resection of the nodules is often performed despite being a time-consuming and expensive approach. The extent of excision must include the whole lesion-even the smallest ones-to avoid rapid recurrence. However, a one-staged treatment may increase the patient quality of life and self-esteem.5
In case of large loss of substance from the scrotal skin with impossibility of primary closure, it is recommended to realize purse-string sutures at the remaining scrotal skin edges to reduce the loss of the substance. Then, it is possible to perform a total skin graft from inguinal area or the lower abdominal fold. The limit of this technique is especially the accessibility to a specialized reconstruction service (plastic surgery or some urology departments). The surgical technique is similar to scrotum lifting. Literature is extremely rare concerning this type of surgery. Reconstruction and aesthetic surgery of the male genital organs in a new and growing discipline.5
Conclusion
Scrotal calcinosis is a rare and benign disease, with major impact on patient's life quality. The pathogenesis and basic origin remain controversial. The theory of the calcification of the preexistent epidermoid cysts appears to be most likely to believe. Complete surgical excision is the recommended treatment, it appears to provide good clinical outcome with low risk of recurrence.
Contributor Information
Houcem Hedhli, Email: houc_m@hotmail.fr.
Amine Hermi, Email: hermiamine@gmail.com.
Mehdi Raboudi, Email: mehdi_raboudi@yahoo.fr.
Hamza Ichaoui, Email: hamzaichaoui360@gmail.com.
Ramzi Khiari, Email: khiariramzi@gmail.com.
Samir Ghozzi, Email: Ghouzzisamir@yahoo.fr.
Riadh Ouhichi, Email: o.riadh@gmail.com.
References
- 1.Lewinski. Lymphangiome der Haut mit verkalktem inhalt. Arch Für Pathol Anat Physiol Für Klin Med 1 févr. 1883;91(2):371–373. [Google Scholar]
- 2.Ahlam A, Hassam B. Scrotal calcinoses [in French] Pan Afr Med J. 2014;18:297. doi: 10.11604/pamj.2014.18.297.4971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tareen A., Ibrahim R.M. Idiopathic scrotal calcinosis - a case report. Int J Surg Case Rep. 2018;44:51–53. doi: 10.1016/j.ijscr.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yuyucu Karabulut Y., Kankaya D., Şenel E., Dölek Y., Uslu A., Sertçelik A. Idiopathic scrotal calcinosis: the incorrect terminology of scrotal calcinosis. G Ital Dermatol E Venereol Organo Uff Soc Ital Dermatol E Sifilogr. 2015;150(5):495–499. [PubMed] [Google Scholar]
- 5.Noel W., Hersant B., Meningaud J.-P. One-staged surgical technique for scrotal calcinosis. Progres En Urol J Assoc Francaise Urol Soc Francaise Urol mars. 2016;26(3):176–180. doi: 10.1016/j.purol.2015.12.004. [DOI] [PubMed] [Google Scholar]