Abstract
Objective:
Evidence-informed alcohol warning labels (AWLs) are a promising, well-targeted strategy to increase consumer awareness of health risks. We assessed consumers’ baseline knowledge of alcohol-related cancer risk, standard drinks, and low-risk drinking guidelines as well as levels of support for AWLs. We further assessed associations with sociodemographic factors.
Method:
Forming part of a larger study testing new evidence-informed AWLs in a northern Canadian territory compared with a neighboring territory, baseline surveys were completed among liquor store patrons systematically selected in both sites. Chi-square and multivariable logistic regression analyses were performed to assess outcomes.
Results:
In total, 836 liquor store patrons (47.8% female) completed baseline surveys across both sites. Overall, there was low knowledge of alcohol-related cancer risk (24.5%), limited ability to calculate a standard drink (29.5%), and low knowledge of daily (49.5%) and weekly (48.2%) low-risk drinking guideline limits. There was moderate support for AWLs with a health warning (55.9%) and standard drink information (51.4%), and lower support for low-risk drinking guideline labels (38.7%). No sociodemographic characteristics were associated with cancer knowledge. Identifying as female and having adequate health literacy were associated with support for all three AWLs; high alcohol use was associated with not supporting standard drink (adjusted odds ratio = 0.60, 95% CI [0.40, 0.88]) and low-risk drinking guideline (adjusted odds ratio = 0.57, 95% CI [0.38, 0.87]) labels.
Conclusions:
Few consumers in this study had key alcohol-related health knowledge; however, there was moderate support for AWLs as a tool to raise awareness. Implementation of information-based interventions such as evidence-informed AWLs with health messages including alcohol-related cancer risk, standard drink information, and national drinking guidelines is warranted.
Alcohol is consumed by more than two billion people worldwide, with global estimates anticipating up to a 17% increase in consumption over the next decade (Manthey et al., 2019). The harms associated with its use are significant, and, in 2016, alcohol contributed to an estimated 3.3 million deaths globally (World Health Organization, 2018), accounting for approximately 4% of all cancer deaths (Global Burden of Disease 2016 Alcohol Collaborators, 2018). In Canada, 78% (22 million) of individuals age 15 years and older reported consuming alcohol in the previous year (Statistics Canada, 2018), and an estimated 15,000 people died of alcohol-attributable causes, one third related to cancer (Zhao et al., 2015). Despite these serious and significant harms, there is low knowledge of alcohol-related health harms, such as increased cancer risk, both internationally and in Canada. Alcohol is often perceived by the public to be less harmful than other controlled substances such as tobacco unless consumed in very high amounts (Buykx et al., 2015; Canadian Cancer Society, 2015; Pettigrew et al., 2016; Rehm et al., 2014; Rundle-Thiele at al., 2013; Wiseman & Klein, 2019), when in fact cancer risk increases even at low levels of alcohol consumption, particularly for breast cancer (Shield et al., 2016). This perception is of even greater consequence when considered in light of Canadian data where 69% of respondents indicated they would decrease their consumption levels if they knew that alcohol increased cancer risk (Canadian Cancer Society, 2015). International studies have found that greater knowledge of alcohol-related harms, particularly cancer risk, is associated with being female, older age, higher socioeconomic status, and adequate health literacy—defined as the ability to obtain and understand basic health information to make appropriate health decisions—as well as with lower levels of alcohol use (Buykx et al., 2015, 2016; Macdonald et al., 2011; Robb et al., 2009; Rundle-Thiele et al., 2013; Weiss, 2005).
Tools designed to inform alcohol consumers about minimizing alcohol-related health risks implemented in Canada and elsewhere include low-risk drinking guidelines (LRDG), which recommend daily and weekly consumption limits that are communicated using standard drink measurements (Butt et al., 2011; Kalinowski & Humphreys, 2016). However, to be effective, consumers must not only be aware of national drinking guidelines and the guidelines’ recommended limits but also understand how to apply them in relation to their own alcohol consumption, which is not often the case (Bowden et al., 2014; Bowring et al., 2012; De Visser & Birch, 2012; Livingston, 2012; McNally et al., 2019; Rosenberg et al., 2018). Similar to other countries with national drinking guidelines, only approximately one quarter of Canadian adults are aware that the LRDG exist, and more than 39% regularly drink in excess of the weekly and 27% in excess of the daily limits, after adjusting for underreporting (McNally et al., 2019; Statistics Canada, 2012; Zhao et al., 2015). Alcohol containers sold in Canada are mandated to list only percentage alcohol-by-volume information. Thus, the number of standard drinks (in Canada, one standard drink equals 13.45 g of pure alcohol), which is the unit of measurement used to convey Canada’s LRDG limits, is not provided on the alcohol container. The disconnect between the LRDG and the information currently listed on alcohol containers is likely one reason Canadian consumers are not aware of the LRDG and are unable to accurately monitor their alcohol consumption and comply with the recommended limits in the guidelines.
Presenting health messages on alcohol warning labels (AWLs) offers one relatively low-cost strategy to provide consumption information and to increase knowledge of alcohol-related risks, because heavier consumers are exposed to AWLs most often (Greenfield, 1997; World Health Organization, 2018). Previous experimental and laboratory based studies have indicated that not only did AWLs displaying standard drink information and LRDG limits improve consumers’ ability to estimate recommended consumption limits (Hobin et al., 2017; Osiowy et al., 2015), but adding labels with cancer warnings also decreased consumers’ motivation to drink (Blackwell et al., 2018). Recent real-world evidence using data from subsequent waves of the current study further showed that exposure to such labels increased knowledge of alcohol–cancer risk and daily and weekly LRDG limits, and reduced overall alcohol consumption over time (Hobin et al., 2020; Schoueri-Mychasiw et al., 2020; Weerasinghe et al., 2020; Zhao et al., 2020). Importantly, as knowledge of alcohol-related harms increases, so too does support for AWLs and other effective alcohol control measures shown to reduce alcohol harm, such as increasing minimum pricing and restricting alcohol availability and marketing; women, those who are older, and those who consume less alcohol are more likely to support such policies (Bates et al., 2018; Buykx et al., 2016; Li et al., 2017; Macdonald et al., 2011; Moskalewicz et al., 2013; Pechey et al., 2014; Weerasinghe et al., 2020). Unfortunately, the majority of labels implemented on alcohol containers globally to date do not communicate these types of messages, nor do they follow best practices for effective product label design, such as being larger, being prominently displayed on the container, having full-color graphics or images, and including personally relevant and direct messages that are regularly rotated to prevent wear-out effects (Ferrence et al., 2007; Fong, 2001; Hammond, 2011; Hobin et al., 2018; Vallance et al., 2018).
The current analysis forms part of a larger quasi-experimental study designed to test the real-world effectiveness of new evidence-informed AWLs presenting a cancer warning, national drinking guidelines, and standard drink information in two cities located in the northern Canadian territories, Whitehorse, Yukon, and Yellowknife, Northwest Territories. The aim of this article is to assess baseline levels of alcohol-related knowledge and of support for AWLs among consumers in the experimental sites, as well as associations with key sociodemographic and alcohol drinking factors. Specifically, this article investigates the degree to which participants know that alcohol can cause cancer, the number of standard drinks in an alcohol container, and the sex-specific daily and weekly standard drink limits recommended in Canada’s LRDG. The degree of support for labels on alcohol containers with a health warning, standard drink information, and Canada’s LRDG is also examined.
Method
Study design
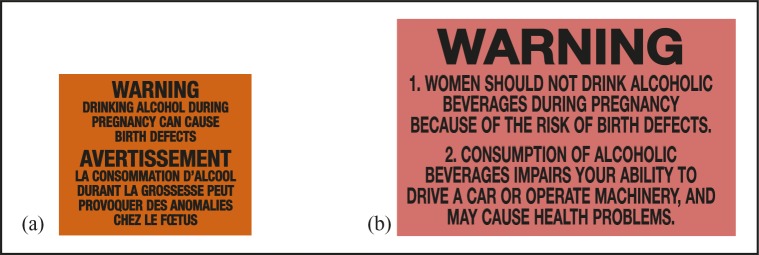
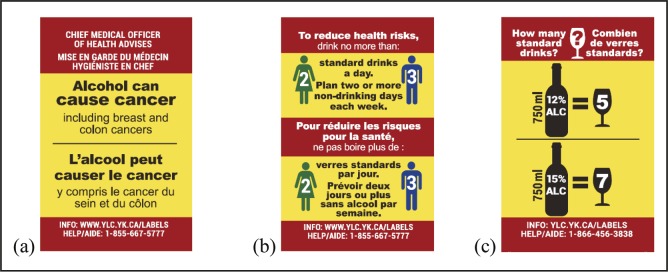
Yukon and Northwest Territories are two northern Canadian territories with similar alcohol distribution systems, population size and demographics, and patterns of alcohol consumption and related harm (higher than the rest of Canada) (Canadian Institute for Health Information, 2017; Canadian Substance Use Costs and Harms Scientific Working Group, 2018; Statistics Canada, 2011a, 2011b, 2018). Further, these two territories are the only jurisdictions in Canada to apply after-market alcohol warning labels by local directive since 1991 (Figures 1a–b) and have well-established labeling procedures. A baseline survey was conducted with systematically selected liquor store patrons in the single government-run liquor store in the capital city of Whitehorse, Yukon (intervention site), and the two government-run stores in Yellowknife, Northwest Territories (comparison site), over a 6-week period in May and June 2017. The surveys formed part of a larger pre–post quasi-experimental study (see Vallance et al., 2020a, for full study protocol) testing the effectiveness of new enhanced evidence-informed AWLs with a cancer warning, national drinking guidelines, and standard drink information. The study was planned for an 8-month intervention in the one government-operated liquor store in the intervention site while usual labeling practices continued in the two government-operated liquor stores in the comparison site (Figures 2a–c).
Figure 1.
Alcohol warning labels on alcohol containers in (a) Yukon (2.3 cm × 2.8 cm) and (b) Northwest Territories (3.0 cm × 5.0 cm) since 1991
Figure 2.
Intervention alcohol warning labels: (a) cancer warning, (b) low-risk drinking guidelines, and (c) standard drink information (5.0 cm × 3.0 cm)
Baseline survey participants were systematically recruited by trained research assistants (RAs) as they exited the liquor stores in the intervention and comparison sites, using a standard intercept technique of approaching every patron who passed a designated landmark. Surveys were administered on tablets in English and completed by participants independently without RA assistance. Up to two RAs recruited participants from Monday to Saturday (all stores are closed Sundays) between 10 A.M. and 6 P.M. in the intervention site and from 12 P.M. to 8 P.M. in the comparison site, covering comparable peak hours at both sites. Participants were screened for eligibility and had to be 19 years and older (legal drinking age in the two territories), had consumed alcohol in the previous month, had purchased alcohol at the liquor store the day of the initial recruitment, and did not self-report currently being pregnant or breastfeeding. Participants were offered a gift card in recognition of their time. The survey took an average of 18 minutes to complete, and participants were asked for email contact information to allow for email recruitment in subsequent waves of the study over the following year. Participants were recruited from the primary off-sale liquor stores in each city center in order to capture a broadly representative sample of adults purchasing alcohol in each site.
A total of 836 eligible participants were recruited and surveyed at baseline in the intervention (n = 505) and comparison sites (n = 331), with an overall response rate of 9.7% (American Association for Public Opinion Research, 2011). This response rate is consistent with other studies using a similar intercept technique (Hobin et al., 2017; Schneider, 2013; Wiggers et al., 2018). All recruitment and survey measures were consistent across the two sites. This study received ethics approval from the Research Ethics Board at Public Health Ontario (ID 2017-010.04) and the Human Research Ethics Board at the University of Victoria (Protocol 17-161), as well as the relevant research licenses required in Yukon and Northwest Territories.
Measures
Survey measures were adapted from items used in evaluations of the AWL in the United States and Canada, in Canadian nutritional labeling practices, and in studies of tobacco warning labels (Greenfield & Kaskutas, 1998; Greenfield et al, 1999; Hammond, 2011; Hobin et al., 2018; Laughery et al., 1993; Pettigrew et al., 2016; Thomas, 2012).
Knowledge that alcohol can cause cancer
To assess knowledge that alcohol can cause cancer, participants were asked, “Based on what you know or believe, can drinking alcohol cause breast cancer/liver disease/the flu/harm to a fetus? Yes/no/don’t know”; only responses to the cancer item are reported here. Responses were dichotomized as 0 = no/don’t know and 1 = yes; 5 (0.6%) participants answered “prefer not to say”/missing and were excluded from these analyses.
Knowledge of standard drinks in preferred beverage type
To assess knowledge of standard drink information, participants were asked to report the number of standard drinks in a container of their preferred beverage type. An image of a container of their preferred drink was shown on-screen, and the container label listed the volume in milliliters and the percentage alcohol by volume. The range of correct responses for the number of standard drinks was between 1.26 and 1.54 for beer, 4 and 6 for wine, 16 and 20 for distilled spirits, and 0.9 and 1.1 for ciders, which is 10% above and below the accurate number of standard drinks for each beverage type. Answers were dichotomized to 0 = incorrect and 1 = correct; 16 (1.9%) participants responded “prefer not to say”/missing and were excluded from these analyses.
Knowledge of sex-specific daily and weekly low-risk drinking guideline limits
To assess knowledge of sex-specific daily and weekly recommended drink limits in Canada’s LRDG, participants were asked, “What is the daily (or weekly) limit of ‘standard drinks’ recommended for males/females (depending on identified sex) in Canada’s Low-Risk Drinking Guidelines?” The number of daily or weekly standard drinks was entered as an open-ended item. The range of correct responses for women was two standard drinks or less (0–2) per day and 10 standard drinks or less (0–10) per week, and for men it was three standard drinks or less (0–3) per day and 15 standard drinks or less (0–15) per week. Responses were dichotomized as 0 = incorrect and 1 = correct; 10 (1.2%) participants responded “prefer not to say”/missing and were excluded from these analyses.
Support for alcohol warning labels with a health message, standard drink information, and low-risk drinking guideline limits
To assess support for AWLs on alcohol containers, participants were asked the degree to which they agree or disagree with the following: “Cans and bottles of alcoholic beverages should be labeled with warnings describing the link between alcohol and diseases, such as cancer”; “Cans and bottles of alcoholic beverages should be labeled with the number of standard drinks per container”; “Cans and bottles of alcoholic beverages should be labeled with low-risk drinking guidelines.” Responses for the three support measures included a 5-point Likert scale, which was dichotomized as 0 = neutral/disagree/strongly disagree/don’t know and 1 = agree/strongly agree. Eight participants (1.0%) for health messages and standard drink information and 10 participants (1.2%) for LRDG responded “prefer not to say”/missing and were excluded from these analyses.
Sociodemographic and alcohol drinking characteristics
Sociodemographic measures included age, sex, ethnicity (White, Aboriginal/other, and unknown), highest level of education attained (completed high school or less, and more than high school, and unknown), and annual household income ($60,000, >$60,000, and unknown). (All amounts are in Canadian dollars.) Health literacy was measured using the Newest Vital Sign assessment tool (≤3, 4–6, and unknown); ≤1–3 correct responses represents limited/possibility of limited literacy, and 4–6 correct responses represents adequate literacy (Weiss et al., 2005). Pattern of alcohol consumption was measured using the quantity/frequency method (Heeb & Gmel, 2005). Participants were asked to indicate how often they drank alcoholic beverages in the past 6 months and how many drinks they usually drank per occasion. Responses were combined to provide a mean number of drinks per week and were categorized using Canada’s LRDG weekly limits (≤10/15 female/male per week, >10/15 female/male per week, and unknown) (Butt et al., 2011).
Statistical analyses
Chi-square analyses (Cody & Smith, 1997) were conducted to assess differences in sociodemographic characteristics by site. To estimate predictors of knowledge that alcohol can cause cancer, of the correct number of standard drinks in a container, and of the correct daily/weekly LRDG limits, four separate multivariable logistic regression models were conducted. To estimate support for AWLs with a health message, standard drink information, and LRDG, three separate multivariable logistic regression models were conducted. Site as well as sociodemographic and alcohol drinking characteristics were entered as independent variables in all models. Adjusted odds ratios (AORs) and corresponding 95% confidence intervals (CIs) were estimated to quantify associations. Sociodemographic and alcohol drinking variables with “don’t know”/“prefer not to say”/missing responses were treated as a separate “unknown” category in the analyses, and AORs and CIs are not presented for this category. As per agreement with the local territorial government partners, ethnicity is included in the sample description and is controlled for in the analyses but is not reported in the results. All analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
In total, 836 participants completed the baseline survey, with 505 (60.4%) in the intervention site and 331 (39.6%) in the comparison site (Table 1). A higher proportion of participants 45 years and older were in the intervention site compared with the comparison site (62.0% vs. 44.4%, p = .0001). There was also a significant difference in ethnicity, with a higher proportion of participants in the intervention than in the comparison site identifying as White (72.9% vs. 65.3%, p = .0005). A higher proportion of participants in the intervention site compared with the comparison site also reported alcohol consumption above the recommended weekly LRDG limits (18.8% vs. 15.4%, p = .0391). There were no other significant differences between the two sites by key sociodemographic characteristics. Overall, 400 (47.9%) participants identified as female, 623 (74.5%) had more than a high school education, 465 (55.6%) reported an annual household income of $60,000 or greater, and 322 (38.5%) participants had adequate health literacy.
Table 1.
Sample characteristics of intervention (Yukon) and comparison (Northwest Territories) sites
| Variable | Total (n = 836) |
Intervention (n = 505) |
Comparison (n = 331) |
||||
| n | % | n | % | n | % | χ2 (p) | |
| Sex | |||||||
| Male | 436 | 52.15 | 255 | 50.50 | 181 | 54.68 | 1.40 |
| Female | 400 | 47.85 | 250 | 49.50 | 150 | 45.32 | (.2359) |
| Age, in years | |||||||
| 19–44 | 376 | 44.98 | 192 | 38.02 | 184 | 55.59 | 24.93 |
| ≥45 | 460 | 55.02 | 313 | 61.98 | 147 | 44.41 | (.0001) |
| Ethnicity | |||||||
| Other | 216 | 25.84 | 109 | 21.58 | 107 | 32.33 | 15.13 |
| White | 584 | 69.86 | 368 | 72.87 | 216 | 65.26 | (.0005) |
| Unknown | 36 | 4.31 | 28 | 5.54 | 8 | 2.42 | |
| Education | |||||||
| ≤Completed high school | 192 | 22.97 | 109 | 21.58 | 83 | 25.08 | 1.37 |
| >Completed high school | 623 | 74.52 | 382 | 75.64 | 241 | 72.81 | (.4447) |
| Unknown | 21 | 2.51 | 14 | 2.77 | 7 | 2.11 | |
| Incomea | |||||||
| <$60,000 | 290 | 34.69 | 187 | 37.03 | 103 | 31.12 | 5.90 |
| ≥$60,000 | 465 | 55.62 | 264 | 52.28 | 201 | 60.73 | (.0522) 54 |
| Unknown | 81 | 9.69 | 54 | 10.69 | 27 | 8.16 | |
| Literacy | |||||||
| ≤3 correct responses | 478 | 57.18 | 280 | 55.45 | 198 | 59.82 | 2.45 |
| 4–6 correct responses | 322 | 38.52 | 205 | 40.59 | 117 | 35.35 | (.2935) |
| Unknown | 36 | 4.31 | 20 | 3.96 | 16 | 4.83 | |
| Alcohol use | |||||||
| ≤10/15 female/male per week | 609 | 72.85 | 371 | 73.47 | 238 | 71.90 | 6.48 |
| >10/15 female/male per week | 146 | 17.46 | 95 | 18.81 | 51 | 15.41 | (.0391) |
| Unknown | 81 | 9.69 | 39 | 7.72 | 42 | 12.69 | |
Notes: Bold indicates p < .05.
In Canadian dollars.
Knowledge that alcohol can cause cancer
Overall, 204 (24.5%) participants knew that drinking alcohol can cause cancer, with no significant differences between intervention and comparison sites (Table 2). Of those that knew alcohol causes cancer, 100 (23.1%) were male and 104 (26.1%) were female; there was no significant difference between men and women for this outcome (AOR = 1.18, 95% CI [0.86, 1.63]). Results of the multivariable logistic regression model indicated no significant differences in cancer knowledge across sociodemographic factors.
Table 2.
Baseline estimates of adjusted odds ratio (AOR) and corresponding 95% confidence interval (CI) of key knowledge outcomes
| A |
B |
C |
D |
|||||
| Know/believe that alcohol causes cancer |
Correctly identify no. of SD per container of preferred drink |
Correctly report daily LRDG limits |
Correctly report weekly LRDG limits |
|||||
| Variables | n (%) | AOR [95% CI]a | n (%) | AOR [95% CI]a | n (%) | AOR [95% CI]a | n (%) | AOR [95% CI]a |
| Site | ||||||||
| Intervention | 128 (25.60) | 1.00 | 161 (32.46) | 1.00 | 262 (52.51) | 1.00 | 244 (48.61) | 1.00 |
| Comparison | 76 (22.96) | 0.89 [0.63, 1.24] | 81 (25.00) | 0.81 [0.56, 1.15] | 147 (44.95) | 0.76 [0.56, 1.04] | 154 (47.53) | 0.91 [0.68, 1.23] |
| Sex | ||||||||
| Male | 100 (23.15) | 1.00 | 78 (18.31) | 1.00 | 219 (50.93) | 1.00 | 206 (47.91) | 1.00 |
| Female | 104 (26.07) | 1.18 [0.86, 1.63] | 164 (41.62) | 3.55 [2.55, 4.99]*** | 190 (47.98) | 0.87 [0.65, 1.17] | 192 (48.48) | 1.02 [0.76, 1.35] |
| Age, in years | ||||||||
| 19–44 | 92 (24.60) | 1.00 | 84 (22.83) | 1.00 | 180 (48.65) | 1.00 | 187 (50.82) | 1.00 |
| ≥45 | 112 (24.51) | 1.00 [0.71, 1.39] | 158 (34.96) | 1.79 [1.26, 2.56]** | 229 (50.22) | 0.86 [0.63, 1.17] | 211 (46.07) | 0.73 [0.54, 0.98]* |
| Education | ||||||||
| ≤Completed high school | 41 (21.47) | 1.00 | 39 (20.86) | 1.00 | 54 (29.35) | 1.00 | 63 (34.05) | 1.00 |
| >Completed high school | 157 (25.20) | 1.19 [0.76, 1.81] | 201 (32.42) | 1.03 [0.66, 1.63] | 353 (56.84) | 2.17 [1.48, 3.19]*** | 332 (53.46) | 1.78[1.23,2.58]** |
| Unknown | 6 (35.29) | 2 (15.38) | 2 (9.52) | 3 (15.00) | ||||
| Incomeb | ||||||||
| <$60,000 | 72 (24.83) | 1.00 | 55 (19.16) | 1.00 | 120 (42.11) | 1.00 | 127 (44.72) | 1.00 |
| ≥$60,000 | 116 (24.95) | 0.98 [0.68, 1.43] | 171 (36.85) | 1.78 [1.19, 2.67]** | 266 (57.20) | 1.27 [0.90, 1.78] | 250 (53.88) | 1.16 [0.83, 1.62] |
| Unknown | 16 (21.05) | 16 (23.19) | 23 (30.26) | 21 (26.92) | ||||
| Health literacy | ||||||||
| ≤3 correct responses | 118 (23.32) | 1.00 | 92 (19.62) | 1.00 | 196 (41.61) | 1.00 | 205 (43.62) | 1.00 |
| 4–6 correct responses | 86 (26.71) | 1.17 [0.83, 1.68] | 140 (43.48) | 2.49 [1.74, 3.57]*** | 205 (63.66) | 1.65 [1.20, 2.28]** | 182 (56.52) | 1.23 [0.90, 1.68] |
| Unknown | 7 (21.21) | 10 (34.48) | 8 (24.24) | 11 (32.35) | ||||
| Alcohol use | ||||||||
| ≤10/15 female/male per week | 148 (24.34) | 1.00 | 203 (33.50) | 1.00 | 335 (55.19) | 1.00 | 321 (52.97) | 1.00 |
| >10/15 female/male per week | 39 (26.71) | 1.18 [0.77, 1.81] | 32 (22.22) | 0.87 [0.55, 1.40] | 61 (42.66) | 0.77 [0.51, 1.14] | 60 (41.38) | 0.71 [0.48, 1.05] |
| Unknown | 17 (21.79) | 7 (10.00) | 13 (17.11) | 17 (22.67) | ||||
Notes: Canada’s Low-Risk Drinking Guidelines recommend no more than 2 standard drinks (SDs) for women/3 for men (daily) and no more than 10 for women/15 for men (weekly). There were 5 participants in Analysis A, 16 in Analysis B, and 10 in Analyses C and D who answered “prefer not to say” or no response and who were excluded from the analyses. The correct SD category ranges were as follows: 1.26–1.54 standard drinks for beers, 4–6 for wine, 16–20 for distilled spirits, and 0.9–1.1 for ciders. Values 10% above and below the accurate number of SDs for wine were used as the “correct” category. Bold indicates statistical significance.
Estimates adjusted for one another;
in Canadian dollars.
p < .05;
p < .01;
p < .001.
Knowledge of standard drinks in preferred beverage type
A total of 242 (29.5%) participants correctly reported the number of standard drinks in a container of their preferred beverage type, with no significant differences between sites (Table 2). Regression results indicate that women (AOR = 3.55, 95% CI [2.55, 4.99]), those 45 years and older (AOR = 1.79, 95% CI [1.26, 2.56]), those with an annual household income of $60,000 or greater (AOR = 1.78, 95% CI [1.19, 2.67]), and those with adequate health literacy (AOR = 2.49, 95% CI [1.74, 3.57]) had greater odds, compared with the referent group, of correctly reporting the number of standard drinks in a container of their preferred beverage type.
Knowledge of sex-specific daily and weekly LRDG limits
Overall, 409 (49.5%) participants were able to correctly report the sex-specific daily LRDG limits, and 398 (48.2%) were able to report the sex-specific weekly LRDG limits (Table 2); there were no significant differences between sites. Regression results indicate that participants who reported having more than a high school education (AOR = 2.17, 95% CI [1.48, 3.19]) and with adequate health literacy (AOR = 1.65, 95% CI [1.20, 2.28]) had greater odds, compared with the referent group, of correctly reporting the daily LRDG limits. Participants 45 years and older (AOR = 0.73, 95% CI [0.54, 0.98]) had lower odds, compared with the referent group, of correctly reporting the weekly LRDG limits, and those with more than a high school education (AOR = 1.78, 95% CI [1.23, 2.58]) had greater odds, compared with the referent group, of correctly reporting the weekly LRDG limits.
Support for alcohol warning labels with health message, standard drink information, and low-risk drinking guideline limits
In total, 463 (55.9%) participants agreed or strongly agreed that alcohol containers should be labeled with AWLs including a health warning, 426 (51.4%) participants agreed or strongly agreed containers should be labeled with standard drink information, and 320 (38.3%) participants agreed or strongly agreed containers should be labeled with LRDG limits; there were no significant differences between intervention and comparison sites. Regression results indicate that participants who identified as female (AOR = 1.45, 95% CI [1.09, 1.92]) and with adequate health literacy (AOR = 1.71, 95% CI [1.25, 2.36]) had greater odds, compared with the referent group, of supporting labeling containers with a health warning (Table 3). Similarly, participants who identified as female (AOR = 1.70, 95% CI [1.27, 2.27]), those with more than a high school education (AOR = 1.44, 95% CI [1.00, 2.03]), and those with adequate health literacy (AOR = 2.02, 95% CI [1.47, 2.78]) had greater odds, compared with the referent group, of supporting labeling containers with standard drink information. Participants who reported consuming above the weekly LRDG limits (AOR = 0.60, 95% CI [0.40, 0.88]) had lower odds, compared with the referent group, of supporting labeling containers with standard drink information (Table 3). Similarly, participants who identified as female (AOR = 1.55, 95% CI [1.15, 2.07]), those 45 years and older (AOR = 1.49, 95% CI [1.09, 2.02]), those with more than a high school education (AOR = 1.75, 95% CI [1.18, 2.58]), and those with adequate health literacy (AOR = 1.55, 95% CI [1.12, 2.14]) had greater odds, compared with the referent group, of supporting labeling containers with LRDG limits. Participants with an annual household income of $60,000 or greater (AOR = 0.64, 95% CI [0.45, 0.90]) and who reported consuming above the weekly LRDG limits (AOR = 0.57, 95% CI [0.38, 0.87]) had lower odds, compared with the referent group, of supporting labeling containers with LRDG limits (Table 3).
Table 3.
Baseline estimates of adjusted odds ratio (AOR) and corresponding 95% confidence interval (CI) of key support outcomes
| A |
B |
C |
|||||
| Agree/strongly agree alcohol containers should be labeled with health warning |
Agree/strongly agree alcohol containers should be labeled with SD information |
Agree/strongly agree alcohol containers should be labeled with LRDG limits |
|||||
| Variables | n (%) | AOR [95% CI]a | n (%) | AOR [95% CI]a | n (%) | AOR [95% CI]a | |
| Site | |||||||
| Intervention | 286 (57.43) | 1.00 | 261 (52.30) | 1.00 | 208 (41.77) | 1.00 | |
| Comparison | 177 (53.64) | 0.93 [0.69, 1.27] | 165 (50.15) | 1.01 [0.75, 1.38] | 112 (34.15) | 0.80 [0.59, 1.09] | |
| Sex | |||||||
| Male | 221 (51.16) | 1.00 | 193 (44.78) | 1.00 | 142 (33.10) | 1.00 | |
| Female | 242 (61.11) | 1.45 [1.09, 1.92]* | 233 (58.69) | 1.70 [1.27, 2.27]*** | 178 (44.84) | 1.55 [1.15, 2.07]** | |
| Age, in years | |||||||
| 19–44 | 195 (52.42) | 1.00 | 182 (49.06) | 1.00 | 127 (34.42) | 1.00 | |
| ≥45 | 268 (58.77) | 1.34 [0.99, 1.79] | 244 (53.39) | 1.21 [0.90, 1.64] | 193 (42.23) | 1.49 [1.09, 2.02]* | |
| Education | |||||||
| ≤Completed high school | 104 (54.17) | 1.00 | 78 (40.84) | 1.00 | 57 (30.00) | 1.00 | |
| >Completed high school | 356 (57.33) | 0.96 [0.67, 1.38] | 346 (55.63) | 1.44 [1.00, 2.03]* | 260 (41.80) | 1.75 [1.18, 2.58]** | |
| Unknown | 3 (20.00) | 2 (13.33) | 3 (21.43) | ||||
| Incomeb | |||||||
| <$60,000 | 154 (53.29) | 1.00 | 139 (48.26) | 1.00 | 116 (40.28) | 1.00 | |
| ≥$60,000 | 270 (58.06) | 0.96 [0.69, 1.34] | 257 (55.27) | 0.89 [0.63, 1.24] | 176 (37.93) | 0.64 [0.45, 0.90]* | |
| Unknown | 39 (52.70) | 30 (40.00) | 28 (37.84) | ||||
| Health literacy | |||||||
| ≤3 correct responses | 240 (50.31) | 1.00 | 205 (42.89) | 1.00 | 164 (34.45) | 1.00 | |
| 4–6 correct responses | 208 (64.60) | 1.71 [1.25, 2.36]*** | 207 (64.29) | 2.02 [1.47, 2.78]*** | 146 (45.34) | 1.55 [1.12, 2.14]** | |
| Unknown | 15 (51.72) | 14 (50.00) | 10 (35.71) | ||||
| Alcohol use | |||||||
| ≤10/15 female/male per week | 352 (58.09) | 1.00 | 344 (56.77) | 1.00 | 254 (41.91) | 1.00 | |
| >10/15 female/male per week | 77 (52.74) | 0.91 [0.62, 1.33] | 59 (40.41) | 0.60 [0.40, 0.88]** | 43 (29.66) | 0.57 [0.38, 0.87]** | |
| Unknown | 34 (44.74) | 23 (30.26) | 23 (30.67) | ||||
Notes: There were 8 participants in Analysis A, 10 in Analysis B, and 8 in Analysis C who answered “prefer not to say” or no response and who were excluded from the analyses. Bold indicates statistical significance.
Estimates adjusted for one another;
in Canadian dollars.
p < .05;
p < .01;
p < .001.
Discussion
This study assessed baseline knowledge of alcohol-related health information and support for AWLs as well as the associations between these outcomes and key sociodemographic characteristics among liquor store patrons in two northern Canadian territories. Overall, there were no significant differences in the main outcomes between participants in Whitehorse and Yellowknife at baseline, indicating that the cities were suitably matched as intervention and comparison sites. Further, this population had relatively low levels of alcohol-related knowledge, which provides justification for the broader study testing the impact of labels with messages related to alcohol and cancer risk, national drinking guidelines, and standard drink information across jurisdictions.
Roughly a quarter of the sample knew that alcohol can cause cancer, which is comparable to the relatively low awareness levels found in previous national and international studies (Buykx et al., 2016; Canadian Cancer Society, 2015; Rundle-Thiele et al., 2013; Scheideler & Klein, 2018; Wiseman & Klein, 2019) and which is anticipated given ongoing alcohol industry efforts to keep this information from the public (Petticrew et al., 2018a, 2018b; Vallance et al., 2020a, 2020b). There were no sociodemographic factors associated with knowing that alcohol is a carcinogen, suggesting that, regardless of age, sex, socioeconomic status, or pattern of alcohol consumption, awareness of this serious alcohol-related health risk remains consistently unknown. Considering the large proportion of Canadians who have indicated that knowledge of alcohol-cancer risk would decrease their consumption (Canadian Cancer Society, 2015), this information is important for consumers to make more informed choices and could potentially contribute to a shift in drinking patterns.
Similar to the findings of previous Canadian studies (McNally et al., 2019; Osiowy et al., 2015; Hobin et al., 2018), less than a third of the overall sample was able to correctly estimate the number of standard drinks in a container of their preferred alcoholic beverage when only volume and percentage alcohol-by-volume information were presented on the label. Women and older participants, as well as those with higher income and health literacy levels, were better able to calculate standard drinks using this limited label information. This outcome further highlights that presenting only percentage alcohol-by-volume information on alcohol labels may unduly disempower more vulnerable and higher consuming groups from accurately tracking their consumption and preventing or reducing harms.
Also consistent with previous research (McNally et al., 2019; Osiowy et al., 2015; Hobin et al., 2018), a comparably low proportion of participants—less than half overall—accurately reported the sex-specific daily and weekly limits recommended in Canada’s LRDG. Knowledge of both sets of drink limits was greater among those with higher education levels, and for the daily limits it was greater among those also with higher health literacy—again suggesting that there is a need for more consistent and accessible exposure to national guidelines. Taken together, these results support previous recommendations (Osiowy et al., 2015; Hobin et al., 2018; Wettlaufer, 2018) to provide both standard drink and sex-specific drink limit information on alcohol container labels to improve all consumers’ ability to estimate not only their total consumption but also their consumption in relation to national drinking guidelines. Providing this combination in an accessible format on alcohol containers would expose a broader range of alcohol consumers—including high-volume drinkers (Greenfield, 1997)—to this information.
Broad support for labeling alcohol containers with a health warning such as cancer risk and standard drink and LRDG information was moderate among this population, with more than half of drinkers supporting labels with a health warning and standard drink information. These findings are in line with Canadian and international research showing that the public supports providing this type of label information—and especially cancer warnings—on alcohol containers (Bates et al., 2018; Buykx et al., 2015; Hobin et al., 2018; Miller et al., 2016; Osiowy et al., 2015; Pettigrew et al., 2014; Thomson et al., 2012; Vallance et al., 2018). Overall support for labeling alcohol containers with the three different types of messages was highest among women and those with higher health literacy levels, which are similar characteristics noted in support for most alcohol policies (Bates et al., 2018; Buykx et al., 2016; Li et al., 2017; Moskalewicz et al., 2013; Pechey et al., 2014; Rundle-Thiele, 2013). Despite the consistent acceptability of labels among this sample and across different jurisdictions and population groups, implementation of evidence-informed labels remains low internationally. This discrepancy points to other barriers to their introduction—including commercial vested interests of keeping consumers in the dark about alcohol-related harms such as cancer risk and lobbying by powerful alcohol industry groups—rather than a lack of public support (Bhattacharya et al., 2018; Casswell et al., 2016; Connor, 2017; Vallance et al., 2020b).
Reporting alcohol consumption levels above the recommended weekly LRDG limits was associated with lower levels of support for both standard drink and LRDG labels, which is consistent with previous research finding that those with higher consumption levels are less supportive of alcohol policies (Bates et al., 2018; Li et al., 2017; Macdonald et al., 2011; Moskalewicz et al., 2013; Pechey et al., 2014; Wilkinson et al., 2009). Interestingly, higher alcohol consumption was not associated with a lower likelihood of supporting labels with a health warning such as cancer risk—which may suggest that consumers would not object to these types of labels regardless of their alcohol consumption patterns. Although displaying LRDG information on labels received less support in this sample and elsewhere (Li et al., 2017), the potentially synergistic effect on consumers’ ability to more accurately monitor their consumption when combined with standard drink measurements warrants their inclusion (Bates et al., 2018).
Limitations
Study limitations include a low response rate common to this type of intercept recruitment technique (Hobin et al., 2017; Schneider, 2013; Wiggers et al., 2018) and participant recruitment from liquor stores in the city centers using nonprobability methods. The sample was therefore not representative of site populations, which limits generalizability. However, the distributions of age, sex, and ethnicity are similar to those in the sample of drinkers in the 2014 Canadian Community Health Survey and can thus be considered broadly representative of people who drink alcohol in Yukon and Northwest Territories. The use of self-report surveys may also be subject to response bias. In addition, only one prompted measure specific to breast cancer was used to test knowledge of alcohol’s carcinogenicity. Future research could include both prompted and unprompted measures assessing knowledge of risk for multiple cancer types.
Conclusion
This study identified low baseline levels of knowledge of alcohol-related harm, such as cancer risk, limited ability to calculate number of standard drinks in containers using currently mandated labeling information, and low knowledge of Canada’s LRDG limits. There was support for AWLs that included a health message such as cancer risk, standard drink information, and national low-risk drinking guidelines. Implementation of evidence-based AWLs is warranted and is likely to receive public support as a tool to increase awareness of alcohol related-risks and to support Canadian consumers in the North and elsewhere to make more informed and safer alcohol choices.
Acknowledgments
The authors acknowledge all of our RAs who helped with data collections, as well as the liquor control boards, health and social services, and especially the community partners in Yukon and Northwest Territories for their commitment and support in developing and executing this research. Special thanks also go to Mark Petticrew and Melanie Wakefield for their expertise and guidance.
Footnotes
This research was funded by Health Canada–Substance Use and Addictions Program #1718-HQ-000003. The views expressed herein do not necessarily represent the views of Health Canada. Thomas K. Greenfield was supported by National Institute on Alcohol Abuse and Alcohol Grant No. P50 AA005595. International Registered Report Identifier (IRRID): RR2-10.2196/16320.
References
- American Association for Public Opinion Research. Standard definitions: Final dispositions of case codes and outcome rates for surveys (7th ed.) 2011. Retrieved from https://www.esomar.org/uploads/public/knowledge-and-standards/codes-and-guidelines/ESOMAR_Standard-Definitions-Final-Dispositions-of-Case-Codes-and-Outcome-Rates-for-Surveys.pdf. [Google Scholar]
- Bates S., Holmes J., Gavens L., de Matos E. G., Li J., Ward B., Buykx P. Awareness of alcohol as a risk factor for cancer is associated with public support for alcohol policies. BMC Public Health. 2018;18:688. doi: 10.1186/s12889-018-5581-8. doi:10.1186/s12889-018-5581-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharya A., Angus C., Pryce R., Holmes J., Brennan A., Meier P. S. How dependent is the alcohol industry on heavy drinking in England? Addiction. 2018;113:2225–2232. doi: 10.1111/add.14386. doi:10.1111/add.14386. [DOI] [PubMed] [Google Scholar]
- Blackwell A. K. M., Drax K., Attwood A. S., Munafo M. R., Maynard O. M. Informing drinkers: Can current UK alcohol labels be improved? Drug and Alcohol Dependence. 2018;192:163–170. doi: 10.1016/j.drugalcdep.2018.07.032. doi:10.1016/j.drugalcdep.2018.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden J. A., Delfabbro P., Room R., Miller C. L., Wilson C. Alcohol consumption and NHMRC guidelines: Has the message got out, are people conforming and are they aware that alcohol causes cancer? Australian and New Zealand Journal of Public Health. 2014;38:66–72. doi: 10.1111/1753-6405.12159. doi:10.1111/1753-6405.12159. [DOI] [PubMed] [Google Scholar]
- Bowring A. L., Gold J., Dietze P., Gouillou M., Van Gemert C., Hellard M. E. Know your limits: Awareness of the 2009 Australian alcohol guidelines among young people. Drug and Alcohol Review. 2012;31:213–223. doi: 10.1111/j.1465-3362.2011.00409.x. doi:10.1111/j.1465-3362.2011.00409.x. [DOI] [PubMed] [Google Scholar]
- Butt P., Beirness D., Stockwell T., Gliksman L., Paradis C. Alcohol and health in Canada: A summary of evidence and guidelines for low-risk drinking. Ottawa, Ontario: Canadian Centre on Substance Abuse; 2011. Retrieved from http://www.ccsa.ca/Resource%20Library/2011-Summary-of-Evidence-and-Guidelines-for-Low-Risk%20Drinking-en.pdf. [Google Scholar]
- Buykx P., Gilligan C., Ward B., Kippen R., Chapman K. Public support for alcohol policies associated with knowledge of cancer risk. International Journal on Drug Policy. 2015;26:371–379. doi: 10.1016/j.drugpo.2014.08.006. doi:10.1016/j.drugpo.2014.08.006. [DOI] [PubMed] [Google Scholar]
- Buykx P., Li J., Gavens L., Hooper L., Lovatt M., Gomes de Matos E., Holmes J. Public awareness of the link between alcohol and cancer in England in 2015: A population-based survey. BMC Public Health. 2016;16:1194. doi: 10.1186/s12889-016-3855-6. doi:10.1186/s12889-016-3855-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Cancer Society. Toronto, ON, Canada: Cancer Care Ontario; 2015. Drinking habits and perceived impact of alcohol consumption [Survey conducted by Leger] [Google Scholar]
- Canadian Institute for Health Information. Alcohol harm in Canada: Examining hospitalizations entirely caused by alcohol and strategies to reduce alcohol harm. Ottawa, ON: Author; 2017. Retrieved from https://www.cihi.ca/sites/default/files/document/report-alcohol-hospitalizationsen-web.pdf. [Google Scholar]
- Canadian Substance Use Costs and Harms Scientific Working Group. Canadian substance use costs and harms: 2007–2014. 2018. (Prepared by the Canadian Institute for Substance Use Research and the Canadian Centre on Substance Use and Addiction.) Ottawa, Ont.: Canadian Centre on Substance Use and Addiction. Retrieved from https://www.ccsa.ca/canadian-substance-use-costs-and-harms-2007-2014-report. [Google Scholar]
- Casswell S., Callinan S., Chaiyasong S., Cuong P. V., Kazantseva E., Bayandorj T., Wall M. How the alcohol industry relies on harmful use of alcohol and works to protect its profits. Drug and Alcohol Review. 2016;35:661–664. doi: 10.1111/dar.12460. doi:10.1111/dar.12460. [DOI] [PubMed] [Google Scholar]
- Cody R. P., Smith J. K. Applied statistics and the SAS programming language. New York, NY: North-Holland; 1997. [Google Scholar]
- Connor J. Alcohol consumption as a cause of cancer. Addiction. 2017;112:222–228. doi: 10.1111/add.13477. doi:10.1111/add.13477. [DOI] [PubMed] [Google Scholar]
- De Visser R. O., Birch J. D. My cup runneth over: Young people’s lack of knowledge of low-risk drinking guidelines. Drug and Alcohol Review. 2012;31:206–212. doi: 10.1111/j.1465-3362.2011.00371.x. doi:10.1111/j.1465-3362.2011.00371.x. [DOI] [PubMed] [Google Scholar]
- Ferrence R., Hammond D., Fong G. Warning labels and packaging. In: Bonnie R. J., Stratton K., Wallace R. B., editors. Ending the tobacco problem: Blueprint for the nation. 2007. Committee on Reducing Tobacco Use: Strategies, barriers, and consequences. Washington, DC: National Academy Press. [Google Scholar]
- Fong G. T. A review of the research on tobacco warning labels, with particular emphasis on the new Canadian warning labels. Waterloo, Ontario: Department of Psychology, University of Waterloo; 2001. [Google Scholar]
- Global Burden of Disease 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: A systematic analysis for the global burden of disease study 2016. The Lancet. 2018;392:1015–1035. doi: 10.1016/S0140-6736(18)31310-2. doi:10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield T. Warning labels: Evidence of harm reduction from long-term American surveys. In: Plant M., Single E., Stockwell T., editors. Alcohol: Minimizing the harm (pp. 105–125) London, England: Free Association Books; 1997. [Google Scholar]
- Greenfield T. K., Kaskutas L. A. Five years’ exposure to alcohol warning label messages and their impacts: Evidence from diffusion analysis. Applied Behavioral Science Review. 1998;6:39–68. doi:10.1016/S1068-8595(99)80004-X. [Google Scholar]
- Greenfield T. K., Graves K. L., Kaskutas L. A. Long-term effects of alcohol warning labels: Findings from a comparison of the United States and Ontario, Canada. Psychology and Marketing. 1999;16:261–282. doi:10.1002/(SICI)1520-6793(199905)16:3<261::AID-MAR5>3.0.CO;2-Z. [Google Scholar]
- Hammond D. Health warning messages on tobacco products: A review. Tobacco Control. 2011;20:327–337. doi: 10.1136/tc.2010.037630. doi:10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- Heeb J. L., Gmel G. Measuring alcohol consumption: A comparison of graduated frequency, quantity frequency, and weekly recall diary methods in a general population survey. Addictive Behaviors. 2005;30:403–413. doi: 10.1016/j.addbeh.2004.04.022. doi:10.1016/j.addbeh.2004.04.022. [DOI] [PubMed] [Google Scholar]
- Hobin E., Bollinger B., Sacco J., Liebman E., Vanderlee L., Zuo F., Hammond D. Consumers’ response to an on-shelf nutrition labelling system in supermarkets: Evidence to inform policy and practice. The Milbank Quarterly. 2017;95:494–534. doi: 10.1111/1468-0009.12277. doi:10.1111/1468-0009.12277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobin E., Vallance K., Zuo F., Stockwell T., Rosella L., Simniceanu A., Hammond D. Testing the efficacy of alcohol labels with standard drink information and national drinking guidelines on consumers’ ability to estimate alcohol consumption. Alcohol and Alcoholism. 2018;53:3–11. doi: 10.1093/alcalc/agx052. doi:10.1093/alcalc/agx052. [DOI] [PubMed] [Google Scholar]
- Hobin E., Weerasinghe A., Vallance K., Hammond D., McGavock J., Greenfield T. K., Stockwell T. Testing alcohol labels as a tool to communicate cancer risk to drinkers: A real-world quasi-experimental study. Journal of Studies on Alcohol and Drugs. 2020;81:249–261. doi: 10.15288/jsad.2020.81.249. doi:10.15288/jsad.2020.81.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalinowski A., Humphreys K. Governmental standard drink definitions and low-risk alcohol consumption guidelines in 37 countries. Addiction. 2016;111:1293–1298. doi: 10.1111/add.13341. doi:10.1111/add.13341. [DOI] [PubMed] [Google Scholar]
- Laughery K. R., Young S. L., Vaubel K. P., Brelsford J. W., Jr. The noticeability of warnings on alcoholic beverage containers. Journal of Public Policy & Marketing. 1993;12:38–56. doi:10.1177/074391569501200105. [Google Scholar]
- Li J., Lovatt M., Eadie D., Dobbie F., Meier P., Holmes J., MacKintosh A. M. Public attitudes towards alcohol control policies in Scotland and England: Results from a mixed-methods study. Social Science & Medicine. 2017;177:177–189. doi: 10.1016/j.socscimed.2017.01.037. doi:10.1016/j.socscimed.2017.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston M. Perceptions of low-risk drinking levels among Australians during a period of change in the official drinking guidelines. Drug and Alcohol Review. 2012;31:224–230. doi: 10.1111/j.1465-3362.2011.00414.x. doi:10.1111/j.1465-3362.2011.00414.x. [DOI] [PubMed] [Google Scholar]
- McNally K., Noonan L. L., Cameron M., Phillips K., Baidoobonso S., Sabapathy D. Public awareness of low-risk alcohol use guidelines. Health Promotion Practice. 2019;20:905–913. doi: 10.1177/1524839918781527. doi:10.1177/1524839918781527. [DOI] [PubMed] [Google Scholar]
- Macdonald S., Stockwell T., Luo J. The relationship between alcohol problems, perceived risks and attitudes toward alcohol policy in Canada. Drug and Alcohol Review. 2011;30:652–658. doi: 10.1111/j.1465-3362.2010.00259.x. doi:10.1111/j.1465-3362.2010.00259.x. [DOI] [PubMed] [Google Scholar]
- Manthey J., Shield K. D., Rylett M., Hasan O. S. M., Probst C., Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. Lancet. 2019;393:2493–2502. doi: 10.1016/S0140-6736(18)32744-2. doi:10.1016/S0140-6736(18)32744-2. [DOI] [PubMed] [Google Scholar]
- Miller E. R., Ramsey I. J., Baratiny G. Y., Olver I. N. Message on a bottle: Are alcohol warning labels about cancer appropriate? BMC Public Health. 2016;16:139. doi: 10.1186/s12889-016-2812-8. doi:10.1186/s12889-016-2812-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskalewicz J., Wieczorek Ł., Karlsson T., Österberg E. Social support for alcohol policy: Literature review. Drugs: Education, Prevention and Policy. 2013;20:361–374. doi:10.3109/09687637.2012.687794. [Google Scholar]
- Osiowy M., Stockwell T., Zhao J., Thompson K., Moore S. How much did you actually drink last night? An evaluation of standard drink labels as an aid to monitoring personal consumption. Addiction Research and Theory. 2015;23:163–169. doi:10.3109/16066359.2014.955480. [Google Scholar]
- Pechey R., Burge P., Mentzakis E., Suhrcke M., Marteau T. M. Public acceptability of population-level interventions to reduce alcohol consumption: A discrete choice experiment. Social Science & Medicine. 2014;113:104–109. doi: 10.1016/j.socscimed.2014.05.010. doi:10.1016/j.socscimed.2014.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petticrew M., Maani Hessari N., Knai C., Weiderpass E. How alcohol industry organisations mislead the public about alcohol and cancer. Drug and Alcohol Review. 2018a;37:293–303. doi: 10.1111/dar.12596. doi:10.1111/dar.12596. [DOI] [PubMed] [Google Scholar]
- Petticrew M., Maani Hessari N., Knai C., Weiderpass E. The strategies of alcohol industry SAPROs: Inaccurate information, misleading language and the use of confounders to downplay and misrepresent the risk of cancer. Drug and Alcohol Review. 2018b;37:313–315. doi: 10.1111/dar.12677. doi:10.1111/dar.12677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew S., Jongenelis M., Chikritzhs T., Slevin T., Pratt I. S., Glance D., Liang W. Developing cancer warning statements for alcoholic beverages. BMC Public Health. 2014;14:786. doi: 10.1186/1471-2458-14-786. doi:10.1186/1471-2458-14-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew S., Jongenelis M. I., Glance D., Chikritzhs T., Pratt I. S., Slevin T., Wakefield M. The effect of cancer warning statements on alcohol consumption intentions. Health Education Research. 2016;31:60–69. doi: 10.1093/her/cyv067. doi:10.1093/her/cyv067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Lachenmeier D. W., Room R. Why does society accept a higher risk for alcohol than for other voluntary or involuntary risks? BMC Medicine. 2014;12:189. doi: 10.1186/s12916-014-0189-z. doi:10.1186/s12916-014-0189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robb K., Stubbings S., Ramirez A., Macleod U., Austoker J., Waller J., Wardle J. Public awareness of cancer in Britain: A population-based survey of adults. British Journal of Cancer, 101, Supplement 2. 2009:S18–S23. doi: 10.1038/sj.bjc.6605386. doi:10.1038/sj.bjc.6605386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg G., Bauld L., Hooper L., Buykx P., Holmes J., Vohra J. New national alcohol guidelines in the UK: Public awareness, understanding and behavioural intentions. Journal of Public Health. 2018;40:549–556. doi: 10.1093/pubmed/fdx126. doi:10.1093/pubmed.fdx126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rundle-Thiele S., Siemieniako D., Kubacki K., Deshpande S. Benchmarking alcohol literacy: A multi-country study. Modern Management Review. 2013;18:99–111. Retrieved from http://doi.prz.edu.pl/pl/pdf/zim/45. [Google Scholar]
- Scheideler J. K., Klein W. M. P. Awareness of the link between alcohol consumption and cancer across the world: A review. Cancer Epidemiology, Biomarkers & Prevention. 2018;27:429–437. doi: 10.1158/1055-9965.EPI-17-0645. doi:10.1158/1055-9965.EPI-17-0645. [DOI] [PubMed] [Google Scholar]
- Schneider R. J. Measuring transportation at a human scale: An intercept survey approach to capture pedestrian activity. Journal of Transport and Land Use. 2013;6:43–59. doi:10.5198/jtlu.v6i3.311. [Google Scholar]
- Schoueri-Mychasiw N., Weerasinghe A., Vallance K., Stockwell T., Zhao J., Hammond D., Hobin E. Examining the impact of alcohol labels on awareness and knowledge of national drinking guidelines: A real-world study in Yukon, Canada. Journal of Studies on Alcohol and Drugs. 2020;81:262–272. doi: 10.15288/jsad.2020.81.262. doi:10.15288/jsad.2020.81.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shield K. D., Soerjomataram I., Rehm J. Alcohol use and breast cancer: A critical review. Alcoholism: Clinical and Experimental Research. 2016;40:1166–1181. doi: 10.1111/acer.13071. doi:10.1111/acer.13071. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. Custom tables on alcohol use from 2003 to 2009-10. Canadian community health survey (database) Ottawa, Ontario: Author; 2011a. Retrieved from https://www150.statcan.gc.ca/n1/pub/82625-x/2010002/article/11261-eng.htm. [Google Scholar]
- Statistics Canada. Canadian Census, 2011. Ottawa, Ontario: Author; 2011b. Retrieved from http://www12.statcan.gc.ca/census-recensement/2011/dp-pd/prof/index.cfm?Lang=E. [Google Scholar]
- Statistics Canada. Canadian Alcohol and Drug Use Monitoring Survey. Ottawa, Ontario: Author; 2012. Retrieved from https://www.canada.ca/en/health-canada/services/health-concerns/drug-prevention-treatment/drug-alcohol-use-statistics/canadian-alcohol-drug-use-monitoringsurvey-summary-results-2012.html. [Google Scholar]
- Statistics Canada. Canadian Community Health Survey (CCHS) 2014. Ottawa, Ontario: Author; 2014. Retrieved from https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&Item_Id=214314. [Google Scholar]
- Statistics Canada. Table: 10-10-0010-01. Sales of alcoholic beverages types by liquor authorities and other retail outlets, by value, volume, and absolute volume. 2018. Retrieved from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1010001001. [Google Scholar]
- Thomas G. Levels and patterns of alcohol use in Canada (Alcohol Price Policy Series) Ottawa, Ontario: Canadian Centre on Substance Abuse and Addiction; 2012. Retrieved from http://www.ccsa.ca/Resource%20Library/CCSA-Patterns-Alcohol-Use-Policy-Canada-2012-en.pdf. [Google Scholar]
- Thomson L. M., Vandenberg B., Fitzgerald J. L. An exploratory study of drinkers views of health information and warning labels on alcohol containers. Drug and Alcohol Review. 2012;31:240–247. doi: 10.1111/j.1465-3362.2011.00343.x. doi:10.1111/j.1465-3362.2011.00343.x. [DOI] [PubMed] [Google Scholar]
- Vallance K., Romanovska I., Stockwell T., Hammond D., Rosella L., Hobin E. “We have a right to know”: Exploring consumer opinions on content, design and acceptability of enhanced alcohol labels. Alcohol and Alcoholism. 2018;53:20–25. doi: 10.1093/alcalc/agx068. doi:10.1093/alcalc/agx068. [DOI] [PubMed] [Google Scholar]
- Vallance K., Stockwell T., Hammond D., Shokar S., Schoueri-Mychasiw N., Greenfield T., Hobin E. Testing the effectiveness of enhanced alcohol warning labels and modifications resulting from alcohol industry interference in Yukon, Canada: Protocol for a quasi-experimental study. JMIR Research Protocols. 2020a;9(1):e16320. doi: 10.2196/16320. doi:10.2196/16320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallance K., Vincent A., Schoueri-Mychasiw N., Stockwell T., Hammond D., Greenfield T. K., Hobin E. News media and the influence of the alcohol industry: An analysis of media coverage of alcohol warning labels with a cancer message in Canada and Ireland. Journal of Studies on Alcohol and Drugs. 2020b;81:273–283. doi: 10.15288/jsad.2020.81.273. doi:10.15288/jsad.2020.81.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weerasinghe A., Schoueri-Mychasiw N., Vallance K., Stockwell T., Hammond D., McGavock J., Hobin E. Improving knowledge that alcohol can cause cancer is associated with consumer support for alcohol policies: Findings from a real-world alcohol labelling study. International Journal of Environmental Research and Public Health. 2020;17:398. doi: 10.3390/ijerph17020398. doi:10.3390/ijerph17020398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss B. D., Mays M. Z., Martz W., Castro K. M., DeWalt D. A., Pignone M. P., Hale F. A. Quick assessment of literacy in primary care: The newest vital sign. Annals of Family Medicine. 2005;3:514–522. doi: 10.1370/afm.405. doi:10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wettlaufer A. Can a label help me drink in moderation? A review of the evidence on standard drink labelling. Substance Use & Misuse. 2018;53:585–595. doi: 10.1080/10826084.2017.1349798. doi:10.1080/10826084.2017.1349798. [DOI] [PubMed] [Google Scholar]
- Wiggers D., Vanderlee L., White C. M., Reid J. L., Minaker L., Hammond D. Food sources among young people in five major Canadian cities. Canadian Journal of Public Health. 2018;109:506–515. doi: 10.17269/s41997-018-0083-0. doi:10.17269/s41997-018-0083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson C., Room R., Livingston M. Mapping Australian public opinion on alcohol policies in the new millennium. Drug and Alcohol Review. 2009;28:263–274. doi: 10.1111/j.1465-3362.2009.00027.x. doi:10.1111/j.1465-3362.2009.00027.x. [DOI] [PubMed] [Google Scholar]
- Wiseman K. P., Klein W. M. P. Evaluating correlates of awareness of the association between drinking too much and cancer risk in the United States. Cancer Epidemiology, Biomarkers & Prevention. 2019;28:1195–1201. doi: 10.1158/1055-9965.EPI-18-1010. doi:10.1158/1055-9965.EPI-18-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global status report on alcohol and health 2018. Geneva, Switzerland: Author; 2018. Retrieved from https://www.who.int/substance_abuse/publications/global_alcohol_report/gsr_2018/en/ [Google Scholar]
- Zhao J., Stockwell T., Thomas G. An adaptation of the Yesterday Method to correct for under-reporting of alcohol consumption and estimate compliance with Canadian low-risk drinking guidelines. Canadian Journal of Public Health. 2015;106:e204–e209. doi: 10.17269/cjph.106.4753. doi:10.17269/cjph.106.4753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Stockwell T., Vallance K., Hobin E. The effects of alcohol warning labels on population alcohol consumption: An interrupted time-series analysis of alcohol sales in Yukon, Canada. Journal of Studies on Alcohol and Drugs. 2020;81:225–237. doi:10.15288/jsad.2020.81.225. [PubMed] [Google Scholar]