Abstract
The unprecedented and rapidly spreading Coronavirus Disease-19 (COVID-19) pandemic has challenged public health care systems globally. Based on worldwide experience, India has initiated a nationwide lockdown to prevent the exponential surge of cases. During COVID-19, management of cardiovascular emergencies like acute Myocardial Infarction (MI) may be compromised. Cardiological Society of India (CSI) has ventured in this moment of crisis to evolve a consensus document for care of acute MI. However, this care should be individualized, based on local expertise and governmental advisories.
Keywords: Corona virus, ST-Elevation MI, Acute coronary syndrome, Coronary thrombosis
1. Introduction
The global Coronavirus Disease-19 (COVID-19) pandemic is an unprecedented, rapidly spreading public health emergency with over 2.5 million cases reported worldwide and about two lakh deaths across 213 countries as on 27th April 2020.1 To reduce person to person transmission, government of India initiated a nationwide lockdown on 25th March 2020. Learning from worldwide experience, the Indian health care system needs to be prepared for a surge in COVID-19 patients. Reperfusion for acute myocardial infarction (AMI) by primary percutaneous coronary intervention (PPCI) or Thrombolysis, is evidence-based, time-critical, life-saving intervention that should not be neglected in the COVID-19 era. Although rare, COVID-19, like influenza, may trigger an AMI by multiple pathways.2 Hence this document is intended to provide strategies for triage and management of patients with AMI in the time of COVID-19.
Given the paucity of adequate data, the guidance provided in this statement is based mainly on expert opinion and the best currently available published information. This guidance may change as more data and experience in managing the epidemic and non-COVID-19 patients become available in this rapidly evolving pandemic.
Based on international experience and various national advisories, social distancing, personal hygiene, using appropriate personal protection equipment (PPE), and isolating the highest risk population (age > 60 years, those with underlying cardiovascular disease or its risk factors such as hypertension and diabetes mellitus, those with medical comorbidities and the immunocompromised patients) are most important in containing and mitigating COVID-19.
2. About COVID-19 infection
-
1.
It is caused by SARS-CoV-2, a single-stranded RNA enveloped virus that binds to ACE2 receptors on lung alveolar cells.3 These receptors are also present in the heart, vascular endothelium, kidney and the intestines.
-
2.
The SARS-CoV-2 virus is spread via respiratory droplets although there are now reports that the virus can be detected in air under experimental condition for a period up to 3 h. Fomites also play a role in transmission with the virus remaining viable in cardboard for 24 h, on plastic and steel for 3 days. The virus can be detected in faeces and blood although this does not seem to be an important mechanism for spread of the virus.4, 5, 6
-
3.
The infectivity of COVID-19 is greater than that of the usual influenza virus, with an estimated R0 value (the basic reproduction number, representing viral infectivity) of 2.2.7 Overall mortality ranges from 0.25% to as high as 3.0%.8
3. Cardiovascular manifestations of COVID-19
-
1.
Although the virus predominantly affects the respiratory system producing a typical influenza like illness, it also shows affinity for the cardiovascular system. COVID-19 patients with pre-existing cardiovascular disease (CVD) have an increased risk of severe disease and death (case fatality rates of 6% among hypertensives, 7.3% among diabetics and 10.5% with CVD).9 Depending upon population studied prevalence of cardiovascular disease ranges from 5 to 15%.9, 10, 11, 12
-
2.
Majority of cardiovascular events in patients with COVID -19 infection are the result of severe inflammatory and hemodynamic changes in patients with extensive respiratory involvement. This produces supply-demand mismatch myocardial ischemia due to hypoxia/hemodynamic instability. These are generally seen in the second week of the illness and may manifest with ECG changes and troponin elevation.9, 10, 11, 12, 13
-
3.
Some patients can present as myocarditis including a severe fulminant myocarditis due to cytokine storm with regional ST elevation, marked troponin release and ventricular dysfunction.14
-
4.
Type I myocardial infarction due to atherosclerotic plaque instability resulting from direct vascular infection is uncommon.
-
5.
Many patients can present with chest pain, shortness of breath and palpitations secondary to pulmonary involvement.
-
6.Thus, the range of cardiovascular manifestations of COVID-19 include
-
a.Acute cardiac injury (defined as “Troponin elevations”) is common. Type I acute coronary syndrome (ACS) is uncommon.
-
b.Myocarditis and cardiomyopathy including a severe fulminant form due to cytokine storm syndrome with elevations in NT-pro-BNP, troponin and IL-6 levels
-
c.Arrhythmia occurred in 16.7% of patients in a case series from China12
- d.
-
a.
4. New challenges in managing MI patients during COVID-19
-
1.
Patient Delay: Due to existing situation prevailing in the country, one can expect delays in patient presentation due to lack of transportation, lack of routine medical services at first medical contact or patient's fear of contracting an infection from the healthcare system. At the height of the epidemic treatment delays may also be expected due to limited emergency medical services on account of sick staff or system overload. Mass public education efforts using media will be needed to assure patients that healthcare services remain operational and safe for use16, 17, 18
-
2.
Current non-availability of a rapid nucleic acid test for SARS-CoV-2 infection does not permit rapid discrimination of patients COVID–19 status (Covid-19 positive or negative). Even when available this testing will also cause some delay in providing reperfusion.19
-
3.
Presently there are limited number of centers for testing for SARS-CoV-2 and test results are available only after 24–72 h.
-
4.
Abnormal troponin values are common among those with COVID-19 infection particularly when testing with a high sensitivity cardiac troponin (hs-cTn) assay. This scenario is more commonly due to direct (“non-coronary”) myocardial injury (myocarditis) or due to Type 2 myocardial infarction (MI) due to supply-demand imbalance in patients with severe pulmonary disease. Type 1 acute myocardial infarction due to plaque rupture triggered by the infection is uncommon. Therefore Troponins should be measured only if diagnosis of MI is being considered on clinical grounds and disregard casually ordered abnormal troponin value.20,21
-
5.
With the anticipated surge, there may be a shortage of appropriate PPE across the country, something already experienced globally.22 To overcome this scarcity, the US FDA recently granted an Emergency Use Authorization (EUA) for the reuse of the single-use-disposable N-95 respirator, using a vaporized hydrogen peroxide decontamination method.23 Use of Ethylene Oxide re-sterilization is currently awaiting FDA clearance24
-
6.
There may be a constant need to reassess the risk-benefit ratio of optimal management strategies for STEMI, weighing in the effect of different stages of the pandemic on hospital preparedness.
5. Recommendations regarding reperfusion strategy for AMI
-
1.
At the present stage in COVID-19 epidemic, it is imperative to screen every patient for history of (h/o) international travel or contact with a COVID-19 patient and fever with respiratory symptoms, on presentation at the first medical contact.
-
2.
The respiratory status of the patient should be assessed and classified. For instance, the risk-benefit ratio of primary PCI may be limited in patients with severe pneumonia.
-
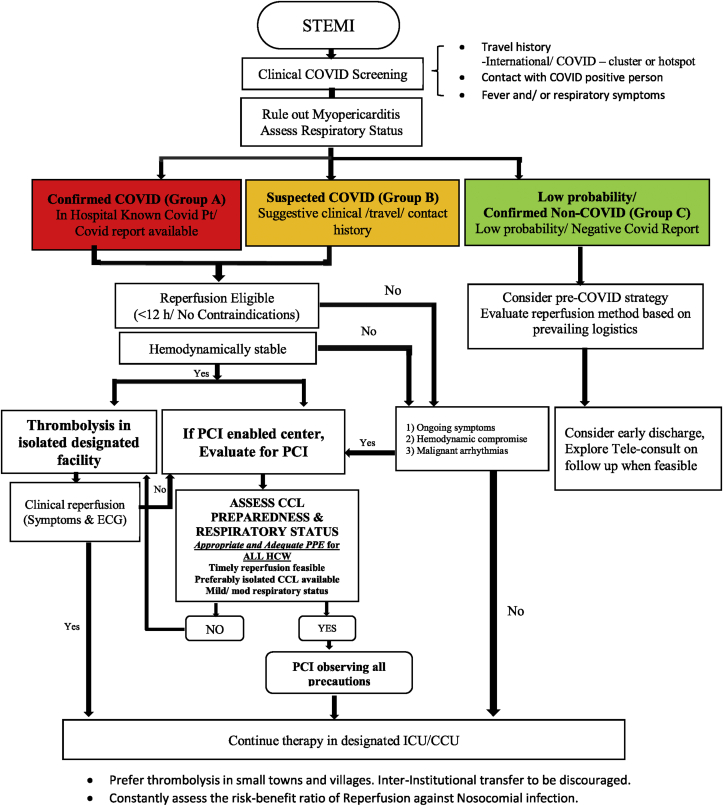
3.Patients presenting with Acute MI could be classified into 3 groups (Fig. 1)
-
a.Confirmed COVID-19 patient (Group A): This would include patients with a positive COVID 19 test result. Currently, such patients are rare in the community in India, but their numbers may grow with increased testing and community spread.
-
b.Suspected COVID-19 patient (Group B): At the present stage in the epidemic this would include patients who have a h/o international travel or are close contacts of a definite COVID-19 patient and has symptoms of fever and/or some respiratory symptoms. However, when the epidemic is in the community stage, many patients will belong to this group even if they have no respiratory symptoms. Rapid testing will permit quick classification of these patients.
-
c.Patient with Low clinical probability of being a COVID-19 patient/Confirmed non-COVID-19 patient (Group C): This would include a patient with no symptoms suggestive of influenza and no history of travel/contact with a COVID-19 patient or a patient whose COVID 19 test is negative.
-
a.
-
4.
Due to non-availability of rapid testing, for decisions regarding management of AMI, it would be best to club Groups A and B together.
-
5.
For the confirmed or suspected COVID-19 patient with ST elevation myocardial infarction (STEMI) presenting within 12 h, primary PCI should be preferred if performed with the necessary precautions and preparedness (see below). Thrombolysis is the prudent option as PCI may not be feasible due to the prevailing logistic problems in performing timely PCI, especially if the patient is hemodynamically stable.18,19 Clinical judgement is important in diagnosing myocardial infarction as myocarditis may masquerade as myocardial infarction. If the patient is hemodynamically unstable, primary PCI would be an ideal option, especially if the COVID-19 pneumonia (respiratory status) is assessed as mild to moderate. However, if primary PCI may not be feasible due to the prevailing logistic problems, thrombolysis should still be tried even if patient is unstable with a plan for rescue PCI.19
-
6.
PCI would also be a desirable option for failed thrombolysis (Rescue PCI) or for a delayed presentation beyond 12 h, especially if pneumonia is mild to moderate and appropriate PPE is available.
-
7.
Primary PCI should be preferably performed in an isolated catheterization laboratory with minimum trained personnel to reduce nosocomial spread. It should not be performed if adequate PPE are not available.
-
8.
For the Group C patients of STEMI, since personnel protection is not in jeopardy, one could resort to the pre-COVID 19 strategy as per previous CSI position statement.25 However, the reperfusion strategy should be based not only on prevailing logistics and hospital preparedness but also on strategies to reduce nosocomial infection.
-
9.
For the stable NSTEMI patient, coronary angiography and or PCI should be preferably deferred until a COVID-19 negative test has been obtained.
-
10.
For the confirmed or suspected COVID-19 patient, thrombolysis should be given in an isolation room/area within the designated ICCU as per institutional protocol.
-
11.
In small towns and villages and at the spokes in a hub and spoke model of STEMI care, thrombolysis should be the preferred reperfusion strategy. Inter-institutional transfers should be discouraged, and the index facility should be encouraged to stabilize the patient using teleconsultation (see Fig. 1).
Fig. 1.
Flow Chart for Reperfusion Strategy for Acute MI during COVID-19 pandemic.
6. Preparedness of the cardiovascular care team
-
1.
PROTECT YOURSELF FIRST not only to avoid getting infected, but also to importantly prevent nosocomial infections (other patients and coworkers) as well as community spread of the infection which could ruin the strategy of containing and mitigating the disease. It is reported that 41.3% of the COVID-19 transmission is presumably hospital-related in Wuhan, China.12
-
2.
While treating a confirmed or suspected COVID-19 patient, appropriate PPE is paramount as per national/international advisories. This should include caps, surgical masks, N-95 respirator masks, face shields, eye protection goggles, gowns, gloves and shoe covers. The entire team should review and practise donning and doffing of PPE. Assistance of infection-control trainers should be taken.
-
3.
It is preferable to intubate patients with borderline respiratory status before wheeling these patients into the cardiac catheterization laboratory (CCL).
-
4.
Echocardiogram should be ordered only if it contributes to decision-making.
-
5.
All personal equipment including stethoscopes and cellphones have to be decontaminated.
-
6.
There should be minimal equipment in the CCL during PCI procedure as these will require decontamination after the procedure in a COVID-19 positive patient.
-
7.
As most CCLs are not negative-pressurized rooms, they will need cleaning after procedures on a patient with suspected or confirmed COVID-19 which may prolong turnaround time of the CCL. When there are multiple CCLs in the hospital it would be useful to use a dedicated isolated CCL for such procedures. It will be useful to employ pragmatic approaches that limit both time of exposure as well as the number of health care personnel involved in the care of COVID-19 patients. This may include prescribing once daily medications where feasible, limiting physical examination to essential components only, and providing teleconsultation on follow up.26
-
8.
The cardiovascular care team professionals maybe called to be on the front line of the COVID-19 response and therefore should design teams for care of these patients. Health care workers over age 60 years should preferably not be in the front line.
-
9.
Collaborate with others: administrators, intensivists, emergency medicine and infectious disease specialists
7. Cardiac medications
The medical management of STEMI remains largely unchanged including antiplatelets, beta blockers, angiotensin converting enzyme inhibitors/angiotensin receptor blockers, nitrates and statins as indicated. There have been previous reports of lower incidence of COPD and influenza deaths in patients on moderate dose statins, but this remains contentious.27,28 Statins should be used as per usual clinical indications. Some of the possible concerns include.
-
1.
ACE inhibitors/angiotensin receptor blockers can be safely continued in patients with COVID-19.29,30
-
2.
Possible interaction of Amiodarone (if prescribed) with Hydroxychloroquine/Chloroquine as well as the anti-retroviral (ARV) drugs Lopinavir/Ritonavir. Regular monitoring of QT interval is required to minimize risk of torsades de pointes.
-
3.
Being a potent liver enzyme CYP3A4 inhibitor, Lopinavir/Ritonavir also has potential drug interaction with antiplatelets, anticoagulants and statins.26
8. Conclusion
The present COVID-19 pandemic is a medical emergency of an unprecedented scale in recent human history. It has called into question, on a global scale, not only the medical preparedness to handle this contagious disease but has also changed the paradigm for management of everyday procedures. As we continue to handle the onslaught of this pandemic, strategies may continue to evolve.18,26,31 Clinical assessment will be necessary to determine whether a patient with ACS is experiencing a primary coronary event or whether it represents a COVID-19 infection with secondary cardiac involvement. Whenever there is a high suspicion of asymptomatic COVID-19 positive patients in the community, the risk to benefit ratio of primary PCI vs lytic therapy to both the patient as well as hospital personnel will have to be assessed. If hospitals are overwhelmed with COVID -19 patients, the feasibility of timely primary PCI will be a challenge and situation should be dealt in accordance with available resources. CCL preparedness with adequate PPEs will be mandatory for care of COVID-19 patients. Protection of health care workers is paramount so that workforce is not depleted and is available as the pandemic evolves.
Conflict of interest
There is no conflict of interest with either the corresponding author or any of the authors/co-authors.
Footnotes
The Cardiological Society of India (CSI) acknowledges the sincere efforts of all the various bodies (viz. your institute or hospital, local and state health authorities, Ministry of Health and Family Welfare and the ICMR) in devising response plans to contain, mitigate and suppress this pandemic. The purpose of this guidance statement is to supplement, not to override, valuable guidance from these bodies.
References
- 1.WHO coronavirus disease (COVID-19) situation dashboard. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 2.Kwong J.C., Schwartz K.L., Campitelli M.A. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378:345–353. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 3.Zhou P., Yang X.L., Wang Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 Mar 17 doi: 10.1056/NEJMc2004973. Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang A., Tong Z.D., Wang H.L. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis. 2020 June 17;26(6) doi: 10.3201/eid2606.200301. Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson N., Kvalsvig A., Barnard L.T., Baker M.G. Case-fatality Risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg Infect Dis. 2020 Mar 13;26(6) doi: 10.3201/eid2606.200320. Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.2648. Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 Feb 15;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;6736:30566–30573. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. J Am Med Assoc. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clerkin K.J., Fried J.A., Raikhelkar J. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020 Mar 21 doi: 10.1161/CIRCULATIONAHA.120.046941. Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Hu H., Ma F., Wei X., Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. March 16 2020 doi: 10.1093/eurheartj/ehaa190. Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020 Mar 18;S0735–1097(20):34637–34644. doi: 10.1016/j.jacc.2020.03.031. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tam C.C.F., Cheung K.S., Lam S. Impact of coronavirus disease 2019(COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ardati A.K., Mena Lora A.J. Circ Cardiovasc Qual Outcomes; 2020 Mar 17. Be prepared. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Welt F.G.P., Shah P.B., Aronow H.D. American college of cardiology's (ACC) interventional council and the society of cardiovascular angiography and intervention (SCAI). Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC's interventional council and SCAI. J Am Coll Cardiol. 2020 Mar 16;S0735–1097(20) doi: 10.1016/j.jacc.2020.03.021. 34566-6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zeng J., Huang J., Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05993-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lippi G., Lavie C.J., Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020 Mar 10;S0033–0620(20):30055–30064. doi: 10.1016/j.pcad.2020.03.001. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Januzzi J.L. 18 Mar 2020. Troponin and BNP Use in COVID-19.https://www.acc.org/latest-in-cardiology/articles/2020/03/18/15/25/troponin-and-bnp-use-in-covid19 [Google Scholar]
- 22.Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources. N Engl J Med. 2020 Mar 23 doi: 10.1056/NEJMsb2005114. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.https://www.fiercebiotech.com/medtech/battelle-deploys-decontamination-system-for-reusing-n95-masks
- 24.https://www.chicagobusiness.com/health-care/medline-resumes-ethylene-oxide-operations-plans-resterilize-used-n95-masks
- 25.Guha S., Sethi R., Ray S. Cardiological society of India: position statement for the management of ST-elevation myocardial infarction in India. Indian Heart J. 2017;69(Suppl 1):S63–S97. doi: 10.1016/j.ihj.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guidance from the CCS COVID-19 Rapid Response Team COVID-19 and Cardiovascular Disease: what the cardiac health care provider should know. www.ccs.ca March 22.
- 27.Frost F.J., Petersen H., Tollestrup K., Skipper B. Influenza and COPD mortality protection as pleiotropic, dose-dependent effects of statins. Chest. 2007;131:1006–1012. doi: 10.1378/chest.06-1997. [DOI] [PubMed] [Google Scholar]
- 28.Is There a Role for Statin Therapy in Acute Viral Infections? March 18 2020. https://www.acc.org/latest-in-cardiology/articles/2020/03/18/15/09/is-there-a-role-for-statin-therapy-in-acute-viral-infections-covid-19 [Google Scholar]
- 29.HFSA/ACC/AHA statement addresses concerns Re: using RAAS antagonists in COVID-19. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19 [DOI] [PMC free article] [PubMed]
- 30.Position statement of the ESC council on hypertension on ACE-inhibitors and angiotensin receptor blockers. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang
- 31.Han Y., Zeng H., Jiang H. CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID-19 epidemic. Circulation. 2020 Mar 27 doi: 10.1161/CIRCgULATIONAHA.120.047011. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]