Abstract
AIM
To evaluate clinical outcomes of unilateral implantation of a diffractive multifocal intraocular lens (IOL) in patients with contralateral monofocal IOL.
METHODS
Twenty-two patients who already had implantation of a monofocal IOL in unilateral eye underwent implantation of a diffractive multifocal IOL in contralateral eye were enrolled. After 1, 6, and 12mo, uncorrected and distant corrected distant visual acuity (UCDVA and DCDVA), uncorrected and distant corrected intermediate-visual acuity (UCIVA and DCIVA), uncorrected and distant corrected near visual acuity (UCNVA and DCNVA), and contrast sensitivity were obtained. Halo/glare symptoms, spectacle dependence, and patient satisfaction were also evaluated.
RESULTS
The mean age was 67.86±7.25y and the average interval between two IOL implantations was 645.82±878.44d. At 1mo, binocular UCDVA was lower than 0.20 logMAR in 76% of patients (mean 0.12±0.13 logMAR), which increased to 90% by 6 and 12mo. The binocular UCDVA was significantly better than the monocular results (P<0.05) at 1, 6, and 12mo. Additionally, UCNVA was lower than 0.40 logMAR in 82% of patients, increasing to 90% by 6 and 12mo. Mean UCNVA in the multifocal IOL implanted eye was statistically significantly better than that in the monofocal IOL implanted eye (P<0.05) at 1, 6, and 12mo. About 5% of patients at 1 and 6mo, reported “severe glare or halo”. Patient satisfaction rates were 95% and 91% at 6 and 12mo, respectively.
CONCLUSION
Unilateral implantation of multifocal IOL in patients with a contralateral, monofocal IOL implantation results in high patient satisfaction rate, with low severe glare or halo rate during follow-up. It can represent a good option for patients who have previously had a monofocal IOL implantation regardless of two year interval duration between two IOL implantations.
Keywords: diffractive multifocal intraocular lens, unilateral implantation, near vision, cataract surgery
INTRODUCTION
The bifocal or multifocal intraocular lens (IOL), accommodative IOL, and pseudophakic monovision were designed to overcome loss of accommodation after cataract surgery[1]–[7]. Recently, implantation of a multifocal IOL has been used more frequently than other types of lens to correct near vision in cataract patients[2].
Bilateral implantation of multifocal IOLs has been reported to provide good binocular function[8]–[9], although there is a well-known disadvantage including reduced contrast sensitivity at low frequency contrast levels[1],[8]–[10]. Based on these studies, bilateral multifocal IOL implantation after cataract surgery might have better results than unilateral implantation[9]. In reality, large number of patients has already underwent monofocal IOL implantation in their one eye. It was reported that unilateral multifocal IOL implantation with contralateral virgin phakic eye was as effective for visual function as bilateral multifocal IOL implantation, in spite of slightly higher level of halo and glare in the unilateral multifocal IOL implantation group[11]–[12].
In our present study, we attempted to evaluate binocular visual function and quality in multifocal IOL implantation in the contralateral eye of patients who had already undergone monofocal IOL implantation in one eye averagely two years ago by measuring both distant, intermediate and near visual acuity and satisfaction rate using a questionnaire.
SUBJECTS AND METHODS
Ethical Approval
All patients provided informed consent, and the study adhered to the principles of the Declaration of Helsinki.
This study was a retrospective case series, including 22 patients who had underwent unilateral cataract surgery with a monofocal IOL implantation and then done contralateral cataract surgery with a multifocal IOL (Tecnis ZMB00, Abbott Medical Optics, Inc., Abbot Park, IL, USA) implantation at the Department of Ophthalmology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, South Korea. Exclusion criteria included an age younger than 45y or older than 80y, an axial length (AL) greater than 26.0 mm or less than 21.5 mm, corneal astigmatism greater than 1.50 diopters (D), intraoperative complications, and ocular disease other than cataract, such as a clinically significant retinal pathology, glaucoma, optic neuropathy, optic disc anomalies, or other disease that could affect visual performance.
Surgical Procedures
IOL power was calculated based on each patient's corneal curvature and AL using an IOLMaster optical biometer (Carl Zeiss Meditec AG, Jena, Germany). After considering each patient's corneal curvature, AL, and anterior chamber depth (ACD), the IOL power was selected to provide emmetropia in the eye to be operated (0.00 to -0.50 D) using the SRK/II[13], SRK/T[14], Haigis[15], or Hoffer Q[16] formula. All operations were performed by the same surgeon (Tchah H). After the application of topical anesthesia [propacaine hydrochloride 0.5% (Alcaine; Alcon Laboratories, Inc., Fort Worth, TX, USA)], a continuous curvilinear capsulorrhexis (CCC) marker with a 6.0 mm diameter was used as a reference to the corneal plane. A 2.2 mm limbal incision was made at a steep axis to reduce corneal astigmatism. CCC and hydrodissection were then performed. Ultrasonic phacoemulsification was carried out. A diffractive multifocal IOL (Tecnis ZMB00, Abbott Medical Optics, Inc., USA) was implanted using an injector. Stromal hydration of the incision site was performed using a balanced salt solution (Alcon Laboratories, Inc.), and the surgery was completed without sutures. Postoperative 0.5% gatifloxacin (Gatiflo; Handok Pharm., Seoul, Republic of Korea) and 1.0% rimexolone (Vexol; Alcon Laboratories, Inc.) eyedrops were administered four times per day for 4wk.
Postoperative Follow-up
All postoperative examinations, including visual acuities at near and far distance, contrast sensitivity, and completion of the questionnaire, were carried out at 1, 6, and 12mo postoperatively. Uncorrected and distant corrected distant visual acuity (UCDVA and DCDVA) were measured at a distance of 5.0 m using a Landolt ‘C’ vision tester. Uncorrected and distant corrected intermediated visual acuity (UCIVA and DCIVA) were measured at a distance of 70 cm using near vision Landolt ‘C’#729111 (Good-Lite Co., Elgin, IL, USA), and uncorrected and distant corrected near-visual acuity (UCNVA and DCNVA) were measured at a distance of 40 cm using near vision illiterate ‘E’ #728000 (Good-Lite Co.). To measure the DCIVA or DCNVA, the intermediate or near visual acuity was checked when the refraction was optimally corrected with spectacles for distance. The mean visual acuity was expressed as the logMAR scale.
Contrast sensitivity was measured in each eye at 5 points [1.5, 3.0, 6.0, 12.0, and 18.0 cycles per degree (CPD)] using the Vision Contrast Test System (Vistech Consultants., Chicago, IL, USA). Contrast sensitivity was measured in both dim (25 lx) and bright (480 lx) light conditions and the test distance was 3 m. Binocular uncorrected reading ability was measured under bright light conditions using the near vision chart (JV institute, Seoul, Republic of Korea). A patient read the chart aloud beginning with the largest characters and continued to read the sentence at each character size. The distance at which the patient considered optimal for reading and could read the words in a specific time interval (1min) was noted.
Patient were asked 6 questions about their satisfaction at 1, 6, and 12mo postoperatively, including questions about their need for near glasses and discomfort from glare under mesopic or photopic conditions. The subjective degree of satisfaction was evaluated with the procedure on a 3-level scale (not satisfied, moderately satisfied, and very satisfied)[11]. The patient's need for near glasses was checked using a 3-level scale (never, sometimes, and always)[11]. Moreover, patients were asked to evaluate how frequently they felt glare and halo using a 3-level scale (severe, moderate, and none to minimal)[11].
Statistical Analysis
Data were presented as mean±standard deviation. Statistics were analyzed using SPSS software (version 18.0, SPSS, Inc., Chicago, IL, USA). Binocular and monocular visual acuities were compared using the Wilcoxon signed-rank test. A paired t-test and Wilcoxon signed rank test were used for comparisons between monofocal IOL-implanted eyes (monofocal group) and multifocal IOL implanted eyes (multifocal group). Two-tailed P-values <0.05 were considered to denote statistically significant differences.
RESULTS
This study included 22 patients who underwent multifocal IOL implantation in the contralateral eye of patients who had already undergone monofocal IOL implantation in one eye (Table 1). The mean patient age was 67.86±7.25y (range, 46 to 76y), and the mean powers of the implanted IOLs were 20.76±2.02 D in monofocal IOL-implanted eyes and 21.57±2.19 D in multifocal IOL-implanted eyes. The mean AL was 23.52±0.97 mm in monofocal IOL-implanted eyes and 23.52±0.90 mm in multifocal IOL-implanted eyes, and the mean preoperative UCDVA (logMAR) was 0.12±0.11 (range, 0 to 0.50) in monofocal IOL-implanted eyes and 0.34±0.18 (range, 0.1 to 0.6) in contralateral multifocal IOL-implanted eyes. The interval between cataract surgeries in each eye was 645.82±878.44d (range, 30 to 2884d), and the monofocal IOLs in previously operated eyes were Tecnis ZCB00 (Abbott Medical Optics, Inc.) for 11 patients, Tecnis ZA9003 (Abbott Medical Optics, Inc.) for 3 patients, and Hoya iMics NY-60 (Hoya Surgical Optics, Tokyo, Japan) in 2 patients, ACRI-SMART 46S (Acri.Tec, Orange City, FL, USA), Acrysof toric SN60T4 (Alcon Laboratories, Inc.), MA60BA (Alcon Laboratories, Inc.), SA60AT (Alcon Laboratories, Inc.), or AR40e (Abbott Medical Optics, Inc.) in one patient each. A previous monofocal IOL type could not be specified in 1 patient. No patients developed complications, but one patient experienced a femtosecond laser-assisted arcuate keratotomy at 1.5mo postoperatively because of astigmatism in the multifocal eye, which decreased from +1.25 D to +0.75 D.
Table 1. Preoperative characteristics of subjects.
| Parameters | n=22 |
| Age (y) | 67.86±7.25 (46-76) |
| Male:female | 9:13 |
| Interval between surgeries (d) | 645.82±878.44 (30-2884) |
| AL (mm) | |
| Monofocal eye | 23.52±0.97 |
| Multifocal eye | 23.52±0.90 |
| IOL power (D) | |
| Monofocal eye | 20.76±2.02 |
| Multifocal eye | 21.57±2.19 |
| UCDVA (logMAR) | |
| Monofocal eye | 0.12±0.11 |
| Multifocal eye | 0.34±0.18 |
| DCDVA (logMAR) | |
| Monofocal eye | 0.08±0.11 |
| Multifocal eye | 0.18±0.16 |
| MR SE (logMAR) | |
| Monofocal eye | 0.00±0.40 (-0.38-0.75) |
| Multifocal eye | -0.03±1.04 (-2.50-2.25) |
AL: Axial length; IOL: Intraocular lens; UCDVA: Uncorrected distant visual acuity; logMAR: Logarithm of minimum angle of resolution; MR SE: Spherical equivalent of manifest refraction; DCDVA: Distant corrected distant visual acuity.
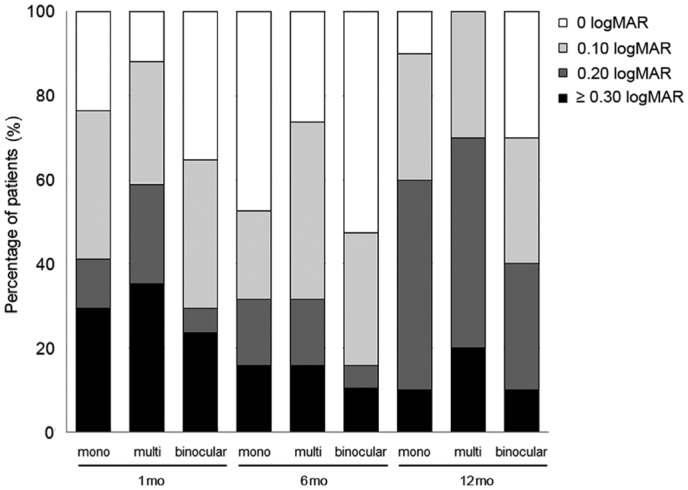
Table 2 shows the postoperative monocular and binocular UCDVA results over time. The mean binocular UCDVA at all follow-up periods was better than 0.12 logMAR (mean 0.12±0.13, 0.07±0.11, and 0.12±0.10 at 1, 6, and 12mo, respectively). The binocular UCDVA was significantly better than the monocular results (P=0.008, 0.008, and 0.03 at 1, 6, and 12mo, respectively).
Table 2. Spherical equivalent and near, intermediate, and distant acuity at 1, 6, and 12mo postoperatively.
| Parameters | 1mo | 6mo | 12mo |
| MR SE | |||
| Monofocal | 0.04±0.39 | 0.12±0.49 | 0.08±0.54 |
| Multifocal | -0.18±0.31 | -0.08±0.34 | 0.04±0.40 |
| UCDVA | |||
| Monofocal | 0.15±0.13a | 0.10±0.13a | 0.17±0.11b |
| Multifocal | 0.20±0.13a | 0.12 ±0.10a | 0.19±0.07b |
| Binocular | 0.12±0.13a | 0.07±0.11a | 0.12±0.10b |
| UCIVA | |||
| Monofocal | 0.45±0.12 | 0.47±0.13 | 0.42±0.08 |
| Multifocal | 0.49±0.12 | 0.40±0.15 | 0.37±0.13 |
| Binocular | 0.41±0.11 | 0.38±0.15 | 0.32±0.10 |
| UCNVA | |||
| Monofocal | 0.52±0.20c | 0.53±0.16c | 0.55±0.16c |
| Multifocal | 0.36±0.13c | 0.29±0.12c | 0.33±0.13c |
| Binocular | 0.37±0.14 | 0.30±0.12 | 0.30±0.17 |
| DCDVA | |||
| Monofocal | 0.05±0.07 | 0.04±0.11 | 0.03±0.17 |
| Multifocal | 0.08±0.12 | 0.05±0.11 | 0.03±0.07 |
| Binocular | 0.04±0.07 | 0.02±0.12 | 0.02±0.05 |
| DCIVA | |||
| Monofocal | 0.41±0.10 | 0.42±0.12 | 0.37±0.10 |
| Multifocal | 0.41±0.12 | 0.37±0.11 | 0.34±0.15 |
| Binocular | 0.35±0.08 | 0.35±0.11 | 0.29±0.14 |
| DCNVA | |||
| Monofocal | 0.40±0.23 | 0.46±0.15 | 0.43±0.15 |
| Multifocal | 0.31±0.15 | 0.26±0.11 | 0.24±0.12 |
| Binocular | 0.30±0.18 | 0.25±0.10 | 0.23±0.12 |
logMAR: Logarithm of minimum angle of resolution; MR SE: Spherical equivalent of manifest refraction; UCDVA and DCDVA: Uncorrected and distant corrected distant visual acuity; UCIVA and DCIVA; Uncorrected and distant corrected intermediate visual acuity; UCNVA and DCNVA: Uncorrected and distant corrected near visual acuity. aP<0.01, bP<0.05: Significant between binocular UCDVA and that of monofocal or multifocal IOL-implanted eye (Wilcoxon signed-rank test); cP<0.01: Significant between UCNVAs of monofocal and multifocal IOL-implanted eyes (Wilcoxon signed-rank test).
The monofocal IOL implanted eye seems to have better UCDVA than the multifocal eye throughout the follow-up period, but this difference was not significant (P=0.16, 0.39, and 0.48 at 1, 6, and 12mo, respectively).
The percentages of patients with a monocular UCDVA lower than 0.20 logMAR were similar in both monofocal and multifocal IOL implanted eyes (70.6% and 64.7% at 1mo, 84.2% and 84.2% at 6mo, and 90% and 80% at 12mo in monofocal and multifocal IOL implanted eyes, respectively) and more than half of the subjects had a visual acuity lower than 0.20 logMAR monocularly. Binocular UCDVA was also lower than 0.10 logMAR in 70.6% patients at 1mo and the percentage increased at 6mo (89.5% at 6mo and 60.0% at 12mo; Figure 1).
Figure 1. Monocular and binocular uncorrected distance visual acuity over time.
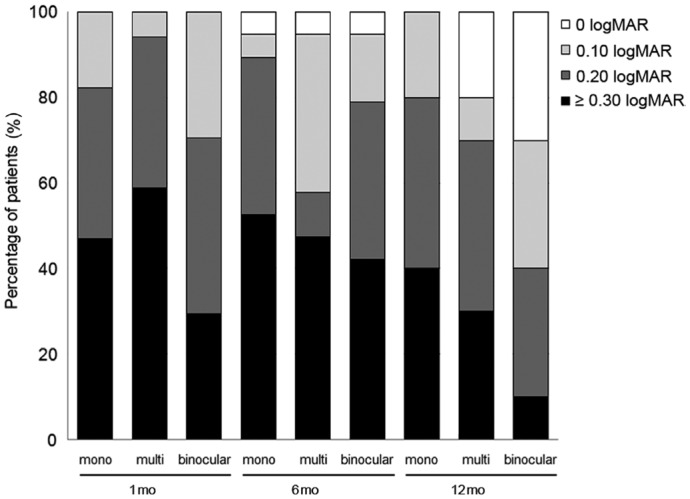
The mean binocular UCNVA at all periods was lower than 0.40 logMAR (mean 0.37±0.14, 0.30±0.12, and 0.30±0.17 at 1, 6, and 12mo, respectively; Figure 2). Mean UCNVA in the multifocal IOL implanted eye was statistically significantly better than that in the monofocal IOL implanted eye (P=0.006, P<0.001, and P=0.007 at 1, 6, and 12mo, respectively; Table 2) and binocular UCNVA was almost equal to that in the multifocal IOL implanted eye (P=0.89, 0.61, and 0.18 at 1, 6, and 12mo, respectively; Table 2 and Figure 2).
Figure 2. Monocular and binocular uncorrected near visual acuity over time.
Mean binocular UCIVA at all periods was equal or lower than 0.40 logMAR (mean 0.41±0.11, 0.38±0.15, and 0.32±0.10 at 1, 6, and 12mo, respectively; Table 2). Mean UCIVA in the multifocal IOL implanted eye was comparable with monofocal IOL implanted eye at 1mo (P=0.20), but statistically significant difference was found in 6mo (0.40±0.15 logMAR in multifocal eyes and 0.47±0.13 in monofocal eyes, P=0.04). At 12mo, 60% of patients had UCIVA over 20/40 (Figure 3).
Figure 3. Monocular and binocular uncorrected intermediate visual acuity over time.
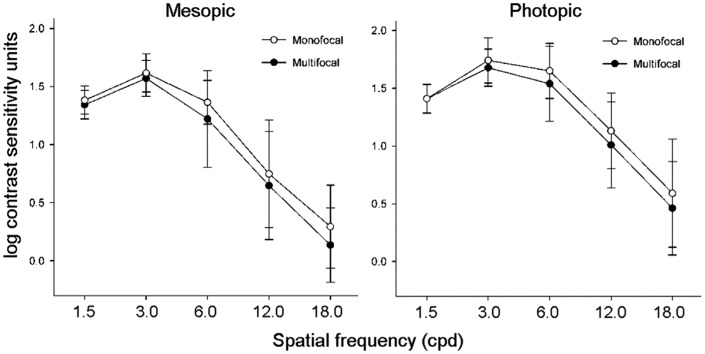
Figure 4 shows the 1-month postoperative contrast sensitivity in each eye. Contrast sensitivity in both mesopic and photopic conditions was not significantly different in multifocal and monofocal IOL implanted eyes even in low CPD photopic conditions (P=0.35 in 3.0 CPD and P=0.48 in 6.0 CPD, by the Mann-Whitney test).
Figure 4. Contrast sensitivity in mesopic and photopic conditions at 1mo postoperatively.
A total of 60.0% of patients responded that they initially only experienced a minimal halo at 1mo postoperatively, and this increased to 79.0% at 6mo. Finally, by 12mo postoperatively, only 1 patient (4.8%) responded that they experienced a severe halo (Figure 5A). Additionally, 65.0% of patients responded that they experienced only a minimal glare at 1mon postoperatively, which increased to 79.0% at 6mo. The number of patients who experienced severe glare was only 1 (4.8%) at 12mo postoperatively (Figure 5B).
Figure 5. Degree of halo and glare over time.
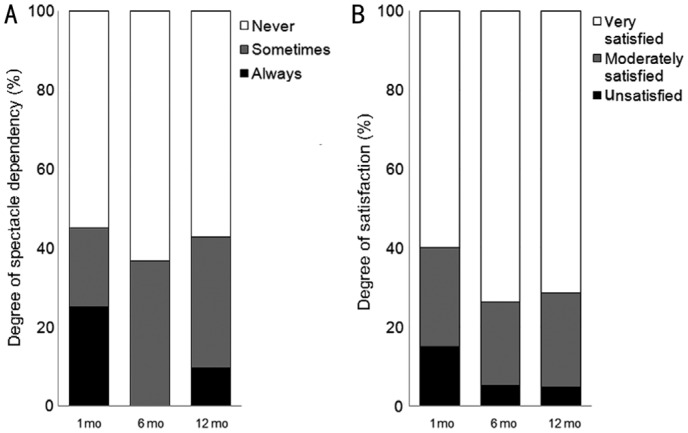
Totally 55.0% of patients responded that they did not use spectacles most of the time, and this frequency increased to 63.2% at 6mo and 57.1% at 12mo. Only 2 patients responded that they had used spectacles most of the time (Figure 6A). Furthermore, a total of 60.0% of patients were satisfied with their visual results at 1mo, which increased to 73.7% at 6mo and 71.4% at 12mo (Figure 6B).
Figure 6. Degree of use of reading glasses and satisfaction over time.
DISCUSSION
Currently, various methods, including cataract extraction with multifocal IOLs, are available for presbyopia correction after cataract surgery[11]–[12],[17]. However, there is a paucity of report regarding clinical outcomes of unilateral implantation of a multifocal IOL in patients with contralateral monofocal IOL. Hybrid monovision, which means pseudophakic monovision using monofocal IOL and multifocal IOL in each eye, was introduced by Iida et al[18]. They reported that monofocal IOL implantation in the dominant eye and a diffractive multifocal IOL in the non-dominant contralateral eye could be effective for managing loss of accommodation after cataract surgery[18]. However, only a few studies have reported outcomes and no study has been performed about multifocal IOL implantation in patients who previously underwent cataract surgery using monofocal IOL long time ago. In our present study, we attempted to evaluate binocular visual acuity after contralateral cataract surgery using multifocal IOL in patients who had previously undergone unilateral monocular cataract surgery in only one eye using monofocal IOL. We also used a questionnaire to measure the degree of patient satisfaction.
The mean binocular UCDVAs were 0.12, 0.07, and 0.12 logMAR in the 1, 6, and 12mo postoperative period, respectively. These values were comparable with the pseudophakic monovision that has been reported as -0.02, -0.04, and -0.03 logMAR of UCDVA in the 1, 6, and 12mo postoperative periods[4], respectively, and as -0.03±0.09 in the 3mo postoperative period[19]. But these differences are not clinically important, because patients were satisfied with visual acuity over certain point. Bilateral multifocal IOL implantation (the same IOL used in present study) has been reported to be -0.11 and -0.10 logMAR of UCDVA in the 3 and 6mo postoperative periods[20], and 0.10±0.18 logMAR in 12mo postoperative period[11], respectively, and hybrid monovision has been reported to be -0.14 in the 3mo postoperative period[18]. In the 1, 6, and 12mo postoperative periods, 71%, 84%, and 60% of patients had a binocular UCDVA of 0.1 logMAR or better, respectively. Slight differences of UCDVA values between this and other studies were not clinically significant.
The mean binocular UCNVA values were 0.37, 0.30, and 0.30 logMAR in the 1, 6, and 12mo postoperative periods, respectively, and were slightly lower than the pseudophakic monovision values reported as 0.09, 0.09, and 0.08 logMAR of UCNVA in the 1, 6, and 12mo postoperative periods[4], and was -0.1±0.11 logMAR in the 3mo postoperative period[19]. The values for bilateral multifocal IOL implantation (the same IOL used in this present study) have been reported to be 0.06 and -0.02 logMAR of UCNVA in the 3 and 6mo postoperative periods, respectively[20], and hybrid monovision has been reported to be 0.02 logMAR in the 3mo postoperative period[18]. Considering these previous data, our present findings were relatively satisfactory, as 47%, 66%, and 60% had a binocular UNDVA of 0.3 logMAR or better in each of the postoperative periods.
Visual acuity at intermediate distance is considered being important because it allows patients to use computer and watch television. Many studies were performed about conventional pseudophakic monovision, but limited results were reported about visual acuity in intermediate distance. In this study, relatively high percentage of patients showed clinically satisfactory binocular UCIVA, which was lower than 0.40 logMAR (70.6%, 57.9%, and 90% in 1, 6, and 12mo, respectively). Also, mean binocular UCIVA in 12mo was similar as that of binocular multifocal IOL implantation study performed in the same hospital as this study (0.32±0.10 in this study and 0.25±0.18)[11].
It was noteworthy that binocular UCDVA results were better than each monocular result at all distances and during every postoperative period due to binocular summation in present study. Moreover, the monofocal IOL-implanted eye seems to have better UCDVA than the multifocal eye throughout the follow-up period, but this difference was not significant in present study. In a comparison of monocular visual acuity, eyes with multifocal IOL showed significantly better results at near distances. Contrast sensitivity is an important factor in multifocal IOL and has been reported to be significantly better in the monofocal than in the multifocal group, irrespective of glare[21]. In our present study, contrast sensitivity was better in the monofocal group at all distances, but the differences were not statistically significant.
Not only objective tests, but also subjective satisfaction are important for cataract surgery. At 1mo postoperatively, only 15% of our current patients were unsatisfied with the surgery, and the 25% of patients required spectacles; these percentages decreased to 5%, 0 and 5%, 10% at 6 and 12mo postoperatively, respectively, probably as a result of binocular summation and adaptation. These percentages of patient satisfaction were relatively higher than those reported for pseudophakic monovision (77.8%, 77.8%, and 83.3% satisfaction rates during the 1, 6, and 12mo postoperative periods, respectively)[4], and similar to the results of a previous hybrid monovision study (93.7% satisfaction rate at 3mo)[18].
Less than 10% of our patients were uncomfortable with halo or glare throughout the postoperative periods. Yoon et al[11] reported that 10% of patients experienced a severe halo in the bilateral multifocal IOL implantation group, while 14% of patients experienced severe halo and 10% of patients experienced severe glare in unilateral multifocal IOL implantation group at 1y postoperatively. Furthermore, Cionni et al[12] found that 58% and 69% of patients reported a halo or glare, respectively, in unilateral multifocal IOL implantation and 77% and 39% of patients reported halo or glare, respectively, in bilateral multifocal IOL implantation at 6mo postoperatively. Overall, the findings of our present study were similar or better than the results of previous unilateral or bilateral multifocal IOL implantation studies.
There were several limitations in present study. First, we could not get information regarding the ocular dominance preoperatively, nor could we address the effects of ocular dominance. Second, the intervals between cataract surgeries in each eye broadly ranged (range, 30 to 2884d). Finally, no test for stereopsis or binocular function was performed to compare unilateral implantation of multifocal IOL to bilateral implantation in present study, although bilateral implantation of multifocal IOLs provided good binocular function[8]–[9].
In conclusion, monocular use of a multifocal IOL could represent an effective approach for the improvement of distant and near vision in patients who have already undergone cataract surgery in only one eye with a monofocal IOL. Notably, it may be a good option for younger patients who have already undergone cataract surgery for any reason.
Acknowledgments
Foundations: Supported by the Student Research Grant of University of Ulsan College of Medicine, Seoul, Korea (No.17-18); Grant from the Asan Institute for Life Sciences, Seoul, Korea (No.2014-464).
Conflicts of Interest: Kim JY, None; Lee Y, None; Won HJ, None; Jeong H, None; Park JH, None; Kim MJ, None; Tchah H, None.
REFERENCES
- 1.Kim M, Kim JH, Lim TH, Cho BJ. Comparison of reading speed after bilateral bifocal and trifocal intraocular lens implantation. Korean J Ophthalmol. 2018;32(2):77–82. doi: 10.3341/kjo.2017.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kretz FT, Choi CY, Müller M, Gerl M, Gerl RH, Auffarth GU. Visual outcomes, patient satisfaction and spectacle independence with a trifocal diffractive intraocular lens. Korean J Ophthalmol. 2016;30(3):180–191. doi: 10.3341/kjo.2016.30.3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marques EF, Castanheira-Dinis A. Clinical performance of a new aspheric dual-optic accommodating intraocular lens. Clin Ophthalmol. 2014;8:2289–2295. doi: 10.2147/OPTH.S72804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pallikaris IG, Portaliou DM, Kymionis GD, Panagopoulou SI, Kounis GA. Outcomes after accommodative bioanalogic intraocular lens implantation. J Refract Surg. 2014;30(6):402–406. doi: 10.3928/1081597X-20140520-01. [DOI] [PubMed] [Google Scholar]
- 5.Ahn JH, Kim DH, Shyn KH. Investigation of the changes in refractive surgery trends in Korea. Korean J Ophthalmol. 2018;32(1):8–15. doi: 10.3341/kjo.2017.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenbaum S. Monovision pseudophakia. J Cataract Refract Surg. 2002;28(8):1439–1443. doi: 10.1016/s0886-3350(02)01218-x. [DOI] [PubMed] [Google Scholar]
- 7.Ito M, Shimizu K, Niida T, Amano R, Ishikawa H. Binocular function in patients with pseudophakic monovision. J Cataract Refract Surg. 2014;40(8):1349–1354. doi: 10.1016/j.jcrs.2013.11.038. [DOI] [PubMed] [Google Scholar]
- 8.Kretz FT, Khoramnia R, Attia MS, Koss MJ, Linz K, Auffarth GU. Clinical evaluation of functional vision of +1.5 diopters near addition, aspheric, rotational asymmetric multifocal intraocular lens. Korean J Ophthalmol. 2016;30(5):382–389. doi: 10.3341/kjo.2016.30.5.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinert RF, Post CT, Jr, Brint SF, et al. A prospective, randomized, double-masked comparison of a zonal-progressive multifocal intraocular lens and a monofocal intraocular lens. Ophthalmology. 1992;99(6):853–860. discussion 860–861. doi: 10.1016/s0161-6420(92)31864-0. [DOI] [PubMed] [Google Scholar]
- 10.Steinert RF, Aker BL, Trentacost DJ, Smith PJ, Tarantino N. A prospective comparative study of the AMO ARRAY zonal-progressive multifocal silicone intraocular lens and a monofocal intraocular lens. Ophthalmology. 1999;106(7):1243–1255. doi: 10.1016/S0161-6420(99)00704-6. [DOI] [PubMed] [Google Scholar]
- 11.Yoon SY, Song IS, Kim JY, Kim MJ, Tchah H. Bilateral mix-and-match versus unilateral multifocal intraocular lens implantation: long-term comparison. J Cataract Refract Surg. 2013;39(11):1682–1690. doi: 10.1016/j.jcrs.2013.04.043. [DOI] [PubMed] [Google Scholar]
- 12.Cionni RJ, Osher RH, Snyder ME, Nordlund ML. Visual outcome comparison of unilateral versus bilateral implantation of apodized diffractive multifocal intraocular lenses after cataract extraction: prospective 6-month study. J Cataract Refract Surg. 2009;35(6):1033–1039. doi: 10.1016/j.jcrs.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 13.Ha A, Wee WR, Kim MK. Comparative efficacy of the new optical biometer on intraocular lens power calculation (AL-scan versus IOLMaster) Korean J Ophthalmol. 2018;32(3):241–248. doi: 10.3341/kjo.2017.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cho K, Lim DH, Yang CM, Chung ES, Chung TY. Comparison of intraocular lens power calculation methods following myopic laser refractive surgery: new options using a rotating scheimpflug camera. Korean J Ophthalmol. 2018;32(6):497–505. doi: 10.3341/kjo.2018.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shammas HJ. Intraocular lens power calculations. Thorofare, NJ: SLACK; 2004. pp. 180–220. [Google Scholar]
- 16.Kang BS, Han JM, Oh JY, Kim MK, Wee WR. Intraocular lens power calculation after refractive surgery: a comparative analysis of accuracy and predictability. Korean J Ophthalmol. 2017;31(6):479–488. doi: 10.3341/kjo.2016.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charman WN. Developments in the correction of presbyopia II: surgical approaches. Ophthalmic Physiol Opt. 2014;34(4):397–426. doi: 10.1111/opo.12129. [DOI] [PubMed] [Google Scholar]
- 18.Iida Y, Shimizu K, Ito M. Pseudophakic monovision using monofocal and multifocal intraocular lenses: hybrid monovision. J Cataract Refract Surg. 2011;37(11):2001–2005. doi: 10.1016/j.jcrs.2011.05.032. [DOI] [PubMed] [Google Scholar]
- 19.Lubiński W, Cholewa M, Podboraczyńska-Jodko K. Conventional pseudophakic monovision-visual function, patient satisfaction and complications. Klin Oczna. 2013;115(3):189–193. [PubMed] [Google Scholar]
- 20.Lubiński W, Gronkowska-Serafin J, Podborączyńska-Jodko K. Clinical outcomes after cataract surgery with implantation of the Tecnis ZMB00 multifocal intraocular lens. Med Sci Monit. 2014;20:1220–1226. doi: 10.12659/MSM.890585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamauchi T, Tabuchi H, Takase K, Ohsugi H, Ohara Z, Kiuchi Y. Comparison of visual performance of multifocal intraocular lenses with same material monofocal intraocular lenses. PLoS One. 2013;8(6):e68236. doi: 10.1371/journal.pone.0068236. [DOI] [PMC free article] [PubMed] [Google Scholar]