Abstract
The coronavirus disease 2019 pandemic has led to widespread change as public health strategies for containment have emphasized social distancing and remaining at home. These policies have led to downscaled clinic volumes, cancellation of elective procedures, enhanced personal protective strategies in the clinic, and adoption of telemedicine encounters. We describe the evidence-based practical approach taken in our ophthalmology department to continue delivering eye care during the pandemic by rescheduling visits, enhancing clinic safety, and adopting virtual video encounters.
Keywords: Coronavirus, Coronavirus disease 2019, COVID-19, Patient triage, Practical approach, Prevention, Safety, Teleophthalmology, Video visits, Web-based vision testing
Key Summary Points
| This article covers the following topics relating to ophthalmology practice during the coronavirus disease 2019 pandemic. |
| Brief background on COVID-19 and ophthalmic manifestations. |
| Triage and rescheduling clinic appointments and OR procedures. |
| Telemedicine, its role and implementation in the current pandemic. |
| Early teleophthalmology experience from UPMC. |
Introduction
In December 2019, the novel coronavirus SARS-CoV-2 emerged in China as the cause of coronavirus disease 2019 (COVID-19). COVID-19 is a contagious and potentially lethal respiratory infection that has resulted in a global pandemic [1]. Countries have worked to stem the spread of infection using social distancing and stay-at-home orders. As a result, routine outpatient visits and elective procedures have been postponed.
In March 2020, the American Academy of Ophthalmology (AAO) recommended limiting office visits to emergencies and canceling elective surgery [2]. Outpatient ophthalmology clinics have adapted rapidly. In this paper, we provide a practical approach to ophthalmic practice in the setting of the pandemic. We describe the development of our department’s policies regarding careful triaging of patients, adoption of safety measures for in-person visits, and introduction of video-visit encounters.
This article does not contain any studies with human participants or animals performed by any of the authors.
Risks of COVID-19 Transmission in Outpatient Eye Clinics
Transmission of COVID-19 occurs by respiratory droplets, contact, and fomites. The ocular surface is thought to play a role in transmission as well. While uncommon, conjunctivitis can be an early manifestation of the disease and can precede pneumonia by several days [3–5]. A retrospective study of 1099 COVID-19 cases across 30 Chinese hospitals identified nine patients (0.8%) with documented conjunctival congestion [6]. However, ocular signs could be more prevalent than noted in retrospective reports. In COVID-19 patients who underwent dedicated ophthalmic examination, 12 of 38 (31.6%) had conjunctival hyperemia, chemosis, or epiphora [5]. Patients with conjunctivitis have had SARS-CoV-2 detected in tears, suggesting infectivity [7]. It is unclear whether viral shedding occurs in the tears of positive cases without ocular signs [8].
Regardless of the likelihood of viral transmission from tears, the close physical contact required for slit-lamp examination and ophthalmoscopy puts eye care providers at high risk for respiratory droplet transmission [9]. Dr. Li Wenliang, an ophthalmologist in Wuhan, China, has been widely recognized for alerting the public of the emerging disease. He is thought to have contracted the virus from an asymptomatic patient and to be the first documented patient-to-ophthalmologist fatality [10]. In Norway, an eye clinic was the epicenter of a local COVID-19 outbreak [11].
Strategies to Mitigate Exposure Risk in Ophthalmology Clinics
The University of Pittsburgh Medical Center (UPMC) Eye Center is an academic health center-based ophthalmology practice in Pittsburgh, Pennsylvania. To protect our providers, our patients, and the community, our practice implemented policies and procedures that addressed patient triage, environmental and personal protective strategies in the clinic, and adoption of video visits.
Patient Triage and Rescheduling
Eye clinic schedules were downsized to prevent crowds of vulnerable patients in our waiting rooms. Our physicians were tasked with triaging scheduled patients into three groups: patients who could be safely rescheduled for 3–6 months in the future, those whose care might be addressed by a video visit, and those who required in-person care to avoid imminent, permanent loss of vision. Similarly, physicians were tasked with triaging surgeries and procedures, delaying all but those aiming to prevent imminent, permanent loss of vision. Triage strategies were in line with recommendations from the AAO and larger ophthalmology community [2, 12, 13].
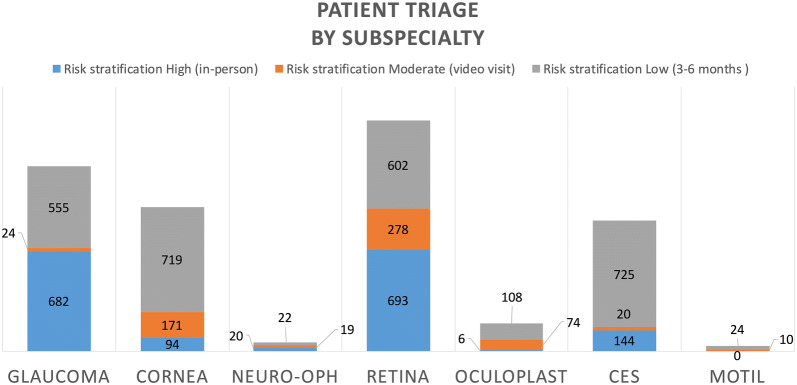
Triage results are presented in Fig. 1. The distribution into three categories varied across subspecialties. Oculoplastic specialty encounters were more likely to be triaged to video visits. Glaucoma specialty encounters, perhaps due to a reliance on tonometry, visual fields, and imaging, were more likely to be either postponed or scheduled for in-person care. Across specialties, preoperative visits and office procedures were generally deferred, while 10–13% of new and established patients were triaged to video visits (Fig. 2).
Fig. 1.
Rescheduling triage results by subspecialty for patients with appointments from March 19 through April 30, 2020. Patients determined to be at high risk of eye disease progression maintained their original appointments as scheduled (“in-person”). Those at moderate risk were offered a video visit for virtual check-in, and low-risk patients had appointments canceled, with plans for rescheduling in 3–6 months. Patient risk stratification was determined by each individual provider. CES, comprehensive eye service; motil, adult strabismus and motility service; neuro-oph, neuro-ophthalmology service; oculoplast, oculoplastic surgery service
Fig. 2.
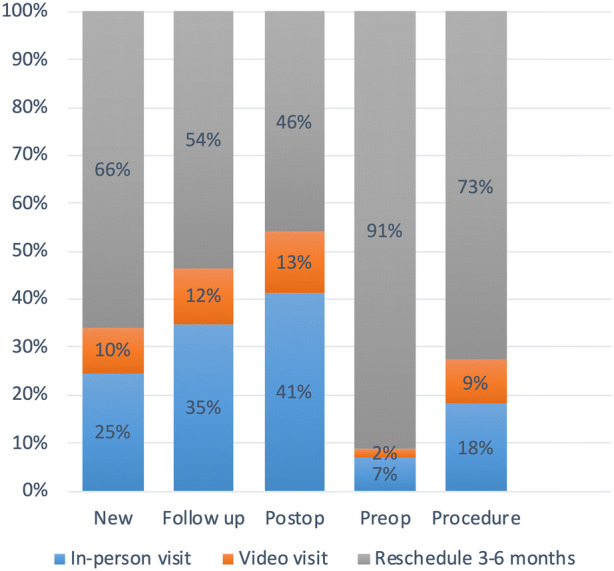
Rescheduling triage results by visit type for patients with appointments from March 19 through April 30, 2020. Results reflect visits from the retina and glaucoma services. New, new patient to the practice; Follow up, established patient seeking a medical visit; Postop, visit within the 90-day postoperative period; Preop, patient visit to plan for surgery, Procedure, patient scheduled for a procedure-only visit with a provider
Clinic Safety
Patients who could not be safely rescheduled and those with new urgent issues were seen for in-person encounters. Procedures were implemented to protect patients and providers.
In response to the severe respiratory distress syndrome (SARS) outbreak in the early 2000s, eye care providers implemented measures to decrease spread of infection. Chan et al. report categorization of ophthalmic patients as “general,” “suspect,” or “probable” infection [14]. General cases were treated with universal precautions: disposable cap, eye protection, surgical mask, gown, and hand washing. For suspect or probable cases, precautions were expanded to include use of a face shield, an N95 mask, and disposable gloves.
Similar protective measures have been described for the current pandemic. Lai et al. report implementation of measures including a questionnaire for travel and contact history and for temperature measurement on clinic entry [15]. A positive screen resulted in deferral of eye care and referral for medical evaluation. Febrile patients requiring urgent eye care were seen in the emergency department. Personal protective equipment was utilized as described by Chan et al. [14]. Air ventilation was enhanced in waiting areas. Exam equipment and high-touch surfaces were disinfected. Protective shields were installed at slit lamps. Similar measures have been undertaken by ophthalmology departments worldwide [16].
Across our department, any patient scheduled for an in-person visit is screened by telephone for symptoms of fever, cough, dyspnea, or contact with sick persons. Temperature is measured upon entry to the building. Positive screens or fever prompt deferral of all but the most urgent care until infection risk is further assessed.
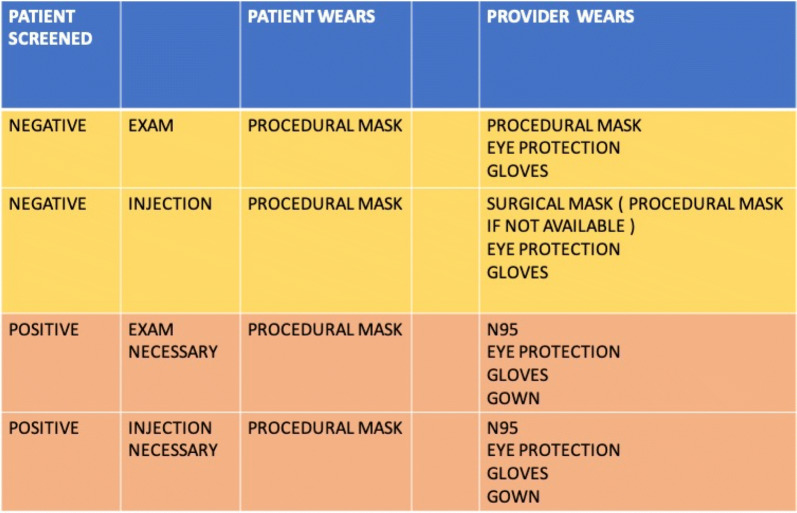
All patients and all clinic staff are required to wear masks during all patient encounters. Providers are required to use N95 masks for encounters with patients who have confirmed disease or a positive symptom screen (Fig. 3). Waiting room chairs are arranged approximately 6 feet apart to promote social distancing. Appointment desk check-in lines are labeled with floor markers to indicate 6 feet of separation. Equipment is disinfected after each use. Hand hygiene on entry and exit of the exam room is required as always. Ophthalmic testing is reserved for cases for which it is needed to guide management in preventing imminent, permanent loss of vision. UPMC continues to perform contact tracing on any positive patients, and thus far there have been no reported cases of spread or outbreak attributed to our department.
Fig. 3.
Personal protective equipment recommendations by patient screen status. The left column indicates whether the patient has screened positive or negative for exposure to a known contact with COVID-19 or report of fever, cough, or dyspnea
Ophthalmology Resident Safety
In addition to minimizing patient visits, our department also reduced in-person educational meetings. Instead, resident lectures and grand rounds presentations are given remotely by interactive online video conference (Zoom, San Jose, CA, USA). Due to a decrease in clinic volumes, ophthalmology resident schedules were reorganized into three teams. One team covers the hospital and clinic setting for a given week, followed by 2 weeks at home in quarantine from the other groups to mitigate any cross-contamination. Inpatient ophthalmology consultations are offered remotely by telephone, photograph, or video with primary teams when deemed appropriate.
Video Visits
Patients not triaged to in-person encounters or rescheduling were offered video visits (Figs. 1, 2). Store-and-forward fundus photography has been used for diabetic retinopathy screening [17], and real-time interactions via phone and video have been described between eye care providers in rural areas and remote consultant ophthalmologists [18].
Video visits have been reported in other surgical subspecialties [19–21]. However, real-time video interactions for ophthalmic visits have not previously been described, and video visits had not previously been offered by our department.
Perhaps more than in other specialties, decision-making in ophthalmology requires examination techniques—refraction, slit-lamp examination, ophthalmoscopy, visual field assessment, and imaging—that cannot feasibly be accomplished remotely. The pandemic allowed our physicians to consider ways that video visits could be used for our patients’ benefit, such as checking on symptoms, refining triage, ensuring adherence to therapy, answering questions, and providing reassurance. We are also exploring tools to maximize the potential of an eye exam by video encounter.
Remote Examination
Visual Function
Platforms for measuring visual acuity have been developed for computers and tablets, with modest evidence for their accuracy. Hundreds of applications (“apps”) have become commercially available for eye-related self-assessment [22], but agreement between app-based measurements and office-measured Snellen visual acuity has been modest [23–26]. Notably, app-based platforms face limitations in usability, availability only on certain devices, cost, and initial setup requirements.
Due to usability limitations of commercial visual acuity assessment platforms, we designed and deployed an online eye chart available from a simple, static webpage. The finished product is available at https://farsight.care and includes a Rosenbaum-style near card, an Amsler grid, and a red dot for color desaturation assessment (Fig. 4). Setup is limited to adjustment of browser magnification settings such that a reference line is matched to the height of a credit card.
Fig. 4.
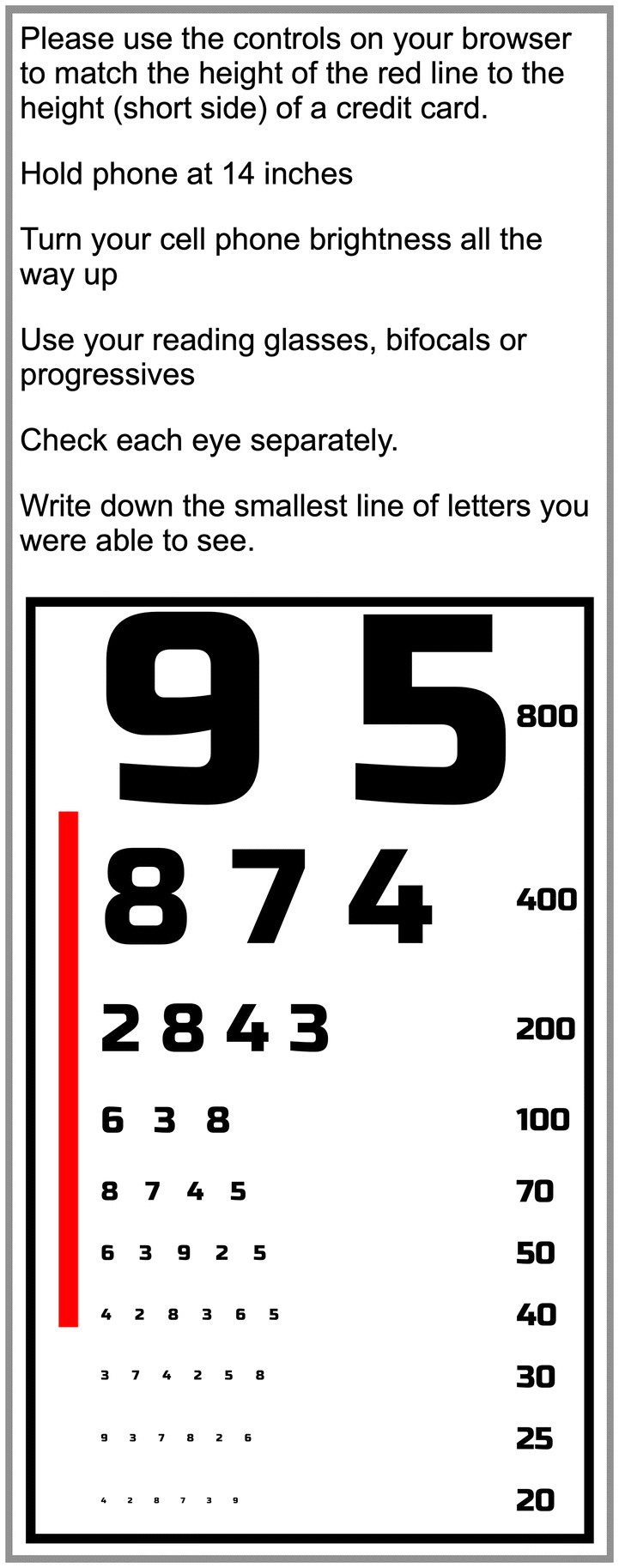
Webpage to assess near visual acuity for video visits, available at https://farsight.care
While the accuracy of the chart requires validation, its ease of accessibility has allowed its use for video visit intake. Prior to a video visit with a provider, the patient is contacted by a department member who works with them to ensure that they are able to use the video platform (Epic, Verona, WI, USA). During that phone call, the patient is directed to https://farsight.care for visual acuity measurement. Amsler grid assessment and desaturation testing are done on a case-by-case basis. At the time of the video visit, the provider has a summary of the chief complaint and the near visual acuity. In several cases in our practice, an afferent pupillary defect was predicted from the desaturation test. Over a 2-week period, approximately 61.4% (108/176) of teleophthalmology patients were able to complete a visual acuity assessment with the Farsight platform. Barriers to completion included patient unavailability for phone call, lack of access to the webpage during prescreen calls, and inadequate time interval between appointment scheduling and execution.
At our Children’s Hospital, parents are provided with instructional video on measuring age-appropriate visual acuity using existing apps (https://youtu.be/Clp_axzAfeQ). Future directions in remote assessment of visual function could include incorporation of validated programs, such as Odysight medical modules, for remote monitoring of visual acuity or metamorphopsia [27].
Anterior Segment and Ocular Adnexa
Video visits allow for at least gross examination of the ocular adnexa and anterior segment. Video visit encounters have been reported for initial patient consultation for cosmetic facial or eyelid surgery [28], and remote assessment of ptosis by photographs has good agreement with subsequent office evaluation [29].
The absence of a slit beam and magnification limit a detailed anterior segment examination, but remote assessment may still provide valuable diagnostic information. For example, video visits can be useful in triaging of anterior segment trauma. Remote assessment of ocular injury in animal models can accurately identify referable conditions, such as eyelid laceration and globe rupture [30]. Additionally, when provided with patient history, corneal photography in telemedicine has demonstrated modest diagnostic specificity compared with in-person slit-lamp examination [31, 32], suggesting some diagnostic utility in virtual examination.
In our practices, video visits for patients with subconjunctival hemorrhages and conjunctivitis resulted in an encounter that did not require follow-up. In other cases, video visits were used to establish a clear need for an in-person visit for patients with pain, redness, or orbital signs. Hundreds of our previously scheduled patients have been identified for video visit encounters, and these visits are ongoing.
Patient Perspectives
Patients interviewed about video visits from a general medicine practice have reported favorable access to providers and decreased travel and wait times [33]. Patients also note limitations, however, and have expressed concerns about the diagnostic accuracy and loss of patient–provider contact. Tools to mitigate some of these concerns have been promoted as a “webside manner:” Providers should engage the patient in a video encounter as they would in an in-person visit, maintaining eye contact, proper posture, and patient-centered communication [33].
Limitations
Video visits are new and clearly have limitations. Providers have expressed concern for the medical and medicolegal ramifications of diagnostic error in the absence of a traditional exam. One can imagine that a first episode of iritis presenting as a red, painful eye could be misinterpreted as a corneal abrasion or viral conjunctivitis, and remote eye exams are currently unvalidated. Research in this realm is ongoing at UPMC regarding patient satisfaction, diagnostic error rates, and clinical outcomes.
Although trainees can join or initiate video visits within Epic to participate in patient care, the volume, quality, and overall impact of video visits on their training and education remains uncertain. In the meantime, we have found that the video visits provide benefit to our patients as a triage tool and as a means to continue management of low-risk cases, and we expect to continue offering video visit encounters post-pandemic.
Patient confidentiality and security must be ensured. We will continue using an encrypted platform and giving providers private spaces for videos with the same privacy levels of in-person visits. Lessons learned from the growing implementation of video visits will inform future best practices.
Considerations for Practices Outside of Academic Medicine
New federal regulations allow for physician discretion while caring for patients during the pandemic [34, 35]. Providers are permitted to conduct telehealth in private settings with reasonable safeguards to limit disclosure of protected health information. With new guidelines, practices without video visit infrastructure in their electronic medical record system may practice teleophthalmology visits using “non-public-facing” remote communication products such as Zoom, Apple, or Google platforms. When patient access to these devices is limited, telephone encounters can be implemented and billed based on time for 10-, 20-, and 30-min intervals [17, 36, 37].
Conclusions
The COVID-19 pandemic has presented challenges to ophthalmic practice. We have discussed ways in which our department has worked to promote safe practice through triage, enhancement and standardization of safety measures and personal protective equipment, and by introducing video visits to allow patient access to ophthalmic care without healthcare exposure.
Looking towards the future, our providers are simultaneously examining which operative cases and clinical visits should be prioritized post-pandemic. We are also evaluating expanded clinic hours and adjusted clinic safety measures to accommodate the influx upon reopening. As we look forward to the end of this pandemic, we will continue to apply the lessons learned to ensure patient safety and ready access to eye care.
Acknowledgements
The authors would like to acknowledge Dr. Tadhg Schempf and Siobahn Gallagher for their assistance with data acquisition, and Dr. Scott Drexler and the division of optometry for their efforts to assess vision using the Farsight platform during the COVID-19 pandemic.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Andrew M. Williams, Gagan Kalra, José-Alain Sahel, Evan L. Waxman, Roxana Fu, Patrick W. Commiskey, Eve M. R. Bowers, Vishal Jhanji, Mary Pitcher, Ken K. Nischal, and Brian R. Rudolph declare no potential conflicts of interest in relation to this work. Kunal K. Dansingani reports a consulting agreement with Biogen.
Compliance with Ethical Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no data sets were generated or analyzed during the current study.
Footnotes
This study has two Co-Principal Investigators: Evan L. Waxman, MD PhD, and Roxana Fu, MD.
Digital Features
To view digital features for this article go to 10.6084/m9.figshare.12179295.
Contributor Information
Evan L. Waxman, Email: waxmane@upmc.edu
Roxana Fu, Email: fur3@upmc.edu.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Ophthalmology. New recommendations for urgent and nonurgent patient care. 2020. https://www.aao.org/headline/new-recommendations-urgent-nonurgent-patient-care. Accessed 8 Apr 2020.
- 3.Cheema M, Aghazadeh H, Nazarali S, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19). Can J Ophthalmol. 2020. 10.1016/j.jcjo.2020.03.003. [DOI] [PMC free article] [PubMed]
- 4.Lu C-w, Liu X-f, Jia Z-f. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020. 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed]
- 6.Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2019;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020 doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seah IYJ, Anderson DE, Kang AEZ, et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. 2019 doi: 10.1016/j.ophtha.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seitzman GD, Doan T. No time for tears. Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parrish RK, Stewart MW, Duncan Powers SL. Ophthalmologists are more than eye doctors—in Memoriam Li Wenliang. Am J Ophthalmol. 2020 [Google Scholar]
- 11.Jørstad ØK, Moe MC, Eriksen K, Petrovski G, Bragadóttir R. Coronavirus disease 2019 (COVID-19) outbreak at the Department of Ophthalmology, Oslo University Hospital. Norway. Acta Ophthalmol. 2020;98(3):e388–e389. doi: 10.1111/aos.14426. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Ophthalmology EyeWiki. Coronavirus (COVID-19). https://eyewiki.org/Coronavirus_(COVID-19). Accessed 14 Apr 2020.
- 13.Romano MR, Montericcio A, Montalbano C, et al. Facing COVID-19 in Ophthalmology department. Curr Eye Res. 2020 doi: 10.1080/02713683.2020.1752737. [DOI] [PubMed] [Google Scholar]
- 14.Chan W, Liu D, Chan P, et al. Precautions in ophthalmic practice in a hospital with a major acute SARS outbreak: an experience from Hong Kong. Eye. 2006;20(3):283–289. doi: 10.1038/sj.eye.6701885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefe's Arch Clin Exp Ophthalmol. 2020;258(5):1049–55. doi: 10.1007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olivia Li J-P, Shantha J, Wong TY, et al. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology. 2020;127(5):569–72. doi: 10.1016/j.ophtha.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS. The current state of teleophthalmology in the United States. Ophthalmology. 2017;124(12):1729–1734. doi: 10.1016/j.ophtha.2017.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Host BK, Turner AW, Muir J. Real-time teleophthalmology video consultation: an analysis of patient satisfaction in rural Western Australia. Clin Exp Optometry. 2018;101(1):129–134. doi: 10.1111/cxo.12535. [DOI] [PubMed] [Google Scholar]
- 19.Rimmer RA, Christopher V, Falck A, et al. Telemedicine in otolaryngology outpatient setting—single Center Head and Neck Surgery experience. Laryngoscope. 2018;128(9):2072–2075. doi: 10.1002/lary.27123. [DOI] [PubMed] [Google Scholar]
- 20.Thelen-Perry S, Ved R, Ellimoottil C. Evaluating the patient experience with urological video visits at an academic medical center. mHealth. 2018;4:54. doi: 10.21037/mhealth.2018.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Viers BR, Lightner DJ, Rivera ME, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68(4):729–735. doi: 10.1016/j.eururo.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Karthikeyan SK, Thangarajan R, Theruvedhi N, Srinivasan K. Android mobile applications in eye care. Oman J Ophthalmol. 2019;12(2):73. doi: 10.4103/ojo.OJO_226_2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perera C, Chakrabarti R, Islam F, Crowston J. The Eye Phone Study: reliability and accuracy of assessing Snellen visual acuity using smartphone technology. Eye. 2015;29(7):888–894. doi: 10.1038/eye.2015.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phung L, Gregori NZ, Ortiz A, Shi W, Schiffman JC. Reproducibility and comparison of visual acuity obtained with SightBook mobile application to near card and Snellen chart. Retina. 2016;36(5):1009–1020. doi: 10.1097/IAE.0000000000000818. [DOI] [PubMed] [Google Scholar]
- 25.Tofigh S, Shortridge E, Elkeeb A, Godley B. Effectiveness of a smartphone application for testing near visual acuity. Eye. 2015;29(11):1464–1468. doi: 10.1038/eye.2015.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsui I, Drexler A, Stanton AL, Kageyama J, Ngo E, Straatsma BR. Pilot study using mobile health to coordinate the diabetic patient, diabetologist, and ophthalmologist. J Diabetes Sci Technol. 2014;8(4):845–849. doi: 10.1177/1932296814529637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brucker J, Bhatia V, Sahel J-A, Girmens J-F, Mohand-Saïd S. Odysight: a mobile medical application designed for remote monitoring—a prospective study comparison with standard clinical eye tests. Ophthalmol Ther. 2019;8(3):461–476. doi: 10.1007/s40123-019-0203-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hwang CJ, Eftekhari K, Schwarcz RM, Massry GG. The aesthetic oculoplastic surgery video teleconference consult. Aesthetic Surg J. 2019;39(7):714–718. doi: 10.1093/asj/sjz058. [DOI] [PubMed] [Google Scholar]
- 29.Rayner S, Beaconsfield M, Kennedy C, Collin R, Taylor P, Murdoch I. Subspecialty adnexal ophthalmological examination using telemedicine. J Telemed Telecare. 2001;7(1_suppl):29–31. doi: 10.1177/1357633X010070S112. [DOI] [PubMed] [Google Scholar]
- 30.Simon DP, Thach AB, Bower KS. Teleophthalmology in the evaluation of ocular trauma. Mil Med. 2003;168(3):205–211. [PubMed] [Google Scholar]
- 31.Woodward MA, Bavinger JC, Amin S, et al. Telemedicine for ophthalmic consultation services: use of a portable device and layering information for graders. J Telemed Telecare. 2017;23(2):365–370. doi: 10.1177/1357633X16634544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woodward MA, Musch DC, Hood CT, et al. Tele-ophthalmic approach for detection of corneal diseases: accuracy and reliability. Cornea. 2017;36(10):1159. doi: 10.1097/ICO.0000000000001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordon HS, Solanki P, Bokhour BG, Gopal RK. “I’m Not Feeling Like I’m Part of the Conversation” patients’ perspectives on communicating in clinical video telehealth visits. J General Internal Med. 2020 doi: 10.1007/s11606-020-05673-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.United States Department of Health and Human Services. COVID-19 and HIPAA: Disclosures to law enforcement, paramedics, other first responders and public health authorities. https://www.hhs.gov/sites/default/files/covid-19-hipaa-and-first-responders-508.pdf. Accessed 9 Apr 2020.
- 35.United States Department of Health and Human Services. FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. https://www.hhs.gov/sites/default/files/telehealth-faqs-508.pdf. Accessed 9 Apr 2020.
- 36.Zimmer-Galler IE, Zeimer R. Telemedicine in diabetic retinopathy screening. Int Ophthalmol Clin. 2009;49(2):75–86. doi: 10.1097/IIO.0b013e31819fd60f. [DOI] [PubMed] [Google Scholar]
- 37.Andino JJ, Castaneda PR, Shah PK, Ellimoottil C. The impact of video visits on measures of clinical efficiency and reimbursement. Urol Practice. 2020 doi: 10.1097/upj.0000000000000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no data sets were generated or analyzed during the current study.