Abstract
National registries provide useful information in understanding outcomes of surgeries that have late sequelae, especially for rare operations such as total elbow arthroplasty (TEA).
A systematic search was performed and data were compiled from the registries to compare total elbow arthroplasty outcomes and evaluate trends. We included six registries from Australia, the Netherlands, New Zealand, Norway, the United Kingdom and Sweden.
Inflammatory arthritis was the most common indication for total elbow arthroplasty, followed by acute fracture and osteoarthritis. When comparing 2000–2009 to 2010–2017 data, total elbow arthroplasty for inflammatory arthritis decreased and total elbow arthroplasty for fracture and osteoarthritis increased. There was an increase in the number of revision TEAs over this time period.
The range of indications for total elbow arthroplasty is broadening; total elbow arthroplasty for acute trauma and osteoarthritis is becoming increasingly more common. However, inflammatory arthritis remains the most common indication in recent years. This change is accompanied by an increase in the incidence of revision surgery.
Cite this article: EFORT Open Rev 2020;5:215-220. DOI: 10.1302/2058-5241.5.190036
Keywords: arthritis, national registry, orthopaedic surgery, osteoarthritis, total elbow arthroplasty, trauma
Introduction
Despite technical improvements over the past 40 years, the long-term clinical results after total elbow arthroplasty (TEA) are not comparable to those of hip and knee arthroplasty.1,2 The number of TEAs placed annually is less than that of total hip or total knee arthroplasties (THA, TKA); in the United Kingdom the incidence of TEA was 612 in 2017 compared to 91,698 for THA and 102,177 for TKA.3
In arthroplasty, it is difficult to identify meaningful trends without large cohorts of patients. This is especially true for TEA as the incidence is low. TEA is included in few national registries and has been added more recently compared to THA and TKA. Moreover, disparities exist between cohort studies. For example, two large studies at tertiary academic medical centres in the USA reported implant survival of between 60% and 95%.4,5 National arthroplasty registries are therefore a valuable data source when patient demographics, the number of arthroplasties, indications for arthroplasty and several outcome measures are recorded.
Many articles have been published on the indications and outcomes of TEA, but large reviews, meta-analyses, as well as systematic pooling of data of national registries are sparse.1,6,7 Therefore, we sought to perform a systematic review of the data from available national registries and compare the indications for TEA and revision surgery rates between 2000 and 2017. We tested the null hypothesis that there is no difference in indications for primary TEA and number of TEAs that underwent revision surgery between 2000–2009 and 2010–2017.
Methods
Literature search
A systematic search was performed using internet search engines (Google, Alphabet Inc., Mountain view, California, USA) and PubMed (US national library of medicine, Rockville Pike, Bethesda, Maryland, USA) for all national joint replacement registries that included elbow arthroplasty. The MeSH terms that were searched included elbow, elbow joint, joint prosthesis, arthroplasty, replacement and registries, and additional terms were elbow replacement, elbow arthroplasty, elbow prosthesis, national and national registry. The reference lists of the included articles were manually checked to avoid missing relevant registries.
Inclusion and exclusion criteria
All national registries that reported original data on TEAs were included. Independent databases studies, local registries or registries that included elbow surgery later than 2017, were excluded.
Data extraction
From the included databases, data were extracted from the annual or periodical reports. From the websites of national orthopaedic associations and their annual reports meta-data on the registries was gathered. The indications were divided into five categories: acute fracture, primary osteoarthritis, inflammatory arthritis, post-traumatic sequelae and other. The category acute fracture was defined as all categories specifying acute trauma or acute fracture without other cause. Primary osteoarthritis was defined as degenerative disease without other cause. Inflammatory arthritis was defined as all primary inflammatory causes and almost completely consisted of rheumatoid arthritis. In the category post-traumatic sequelae, we included all secondary-trauma-related reports, including secondary osteoarthritis, late trauma complications and trauma sequalae. All other indications were included in the category other. Neoplasms and necrosis were added to other as occurrences were rare. Data were grouped into the time periods 2000–2009 and 2010–2017 for comparison of indications for TEA and revision surgery rates.
Twelve national joint replacement registries were identified, registries from Canada, Denmark and Iran did not include elbow arthroplasties and The American Joint Replacement Registry (USA) only included elbow arthroplasty starting in 2018. Scotland did not report any specifics on TEA and Finland did not publish reports. We included registries from Australia (AUS), the Netherlands (NL), New Zealand (NZ), Norway (NOR), the United Kingdom (UK) and Sweden (SE) and included patients from 1994–2017 (Table 1).
Table 1.
Included registries.
| Year | Organization | Obligatory | Source | Patient consent | Validation | Completeness | Reference | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| United Kingdom
http://www.njrreports.org.uk |
2012-2017 | NJR | No | Annual report | Yes | Yes | 95% | 8 | Revision, Mortality |
| Australia
https://aoanjrr.sahmri.com |
2004-2017 | AOANJRR | No | Annual report | No | Yes | 94% | 9 | Revision |
| Norway
http://nrlweb.ihelse.net |
1994-2017 | NRL | No | Annual report | Yes | Yes | 97% | 10 | Revision |
| New Zealand
https://nzoa.org.nz |
1999-2017 | NZOA | Yes | Annual report | Yes | Yes | Not reported | 11 | Revision, Oxford Elbow Score |
| Netherlands
www.lroi-rapportage.nl |
2014-2017 | LROI | No | Annual report | Yes | Yes | 91% | 12 | Revision |
| Sweden
http://www.ssas.se |
1999-2017 | SSAS | No | Annual report | No | Yes | > 90% | 13 | Revision, QuickDash |
Note. NJR, National Joint Registry; AOANJRR, Australian Orthopaedic Association National Joint Replacement Registry; NRL, Nasjonalt Register for Leddproteser; NZOA, New Zealand Orthopedic Association; LROI, Landelijke Registratie Orthopedische Implantaten; SSAS, Svenska Skulder- och Armbågssällskapet.
Risk of bias was assessed for each registry. All were large databases without comparison or analysis and the reported data were validated with hospital records to assess completeness. Data on completeness rate was collected from the latest reports and was higher than 90% in all registries that disclosed completeness. Risk of bias was determined to be low.
In the Netherlands, TEA was included starting from 2014. The Australian Orthopaedic Association reported data from 2004 but lacked annual reports. The United Kingdom included data from England, Northern Ireland, Wales and the Isle of Man. Scotland’s national registry included elbow surgery but did not report indications for TEA. The New Zealand registry did not differentiate between acute fracture and secondary-trauma-related diagnoses, the category trauma from this registry was added to acute fracture. All registries published periodical reports at least yearly.
New Zealand, Norway and Sweden included data from 2000, and these three registries were used to make a comparison between the time periods 2000–2009 and 2010–2017. Some data could not be compared, for example due to initial diagnoses being categorized differently or different collection of patient-related outcomes. None of the registries reported any outcome measures per indication for surgery, therefore we were unable to compare surgery outcomes between the categories. Only the registries from Sweden (QuickDash) and New Zealand (Oxford Elbow Score) included specific measures evaluating elbow outcomes.
Four registries (AUS, NL, NOR, UK; n = 9037) included both total elbow arthroplasties and other types of elbow arthroplasties (partial arthroplasties). Of all the elbow arthroplasties 50% (4511) were TEAs. In the UK, TEA made up the biggest portion of all elbow arthroplasties (78%), followed by Norway (76%) and the Netherlands (53%). In Australia partial arthroplasties were more common than TEA (28%) (p < 0.0001). The Swedish and New Zealand registries only included TEAs. Overall, a total of 6544 total elbow arthroplasties from these six registries were included. Analysis was performed including all total elbow arthroplasties.
Statistical analysis
Fisher’s exact test was used to compare indication rates between the time periods 2000–2009 and 2010–2017. Linear regression was used to assess changes in the incidence of revision surgery between 2000–2017. STATA software (StataCorp, College Station, Texas, USA) was used to perform data analysis. A p-value of < 0.05 was considered statistically significant.
Results
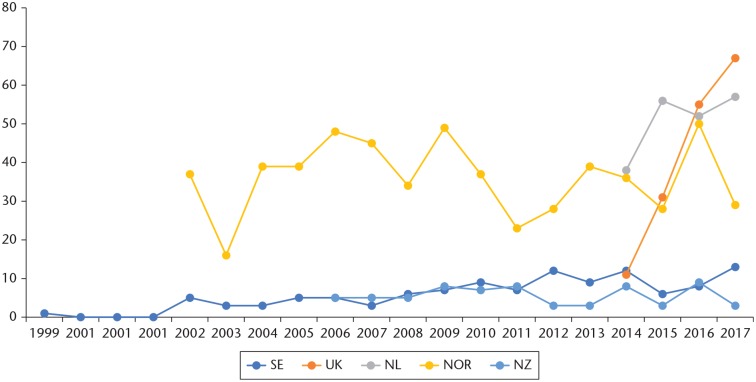
Inflammatory arthritis was the most common indication for TEA (44%) followed by acute fracture (28%), primary osteoarthritis (17%), post-traumatic sequelae (9%) and other (2%) (all registries, Fig. 1).
Fig. 1.
Indications for total elbow arthroplasty (N = 6544).
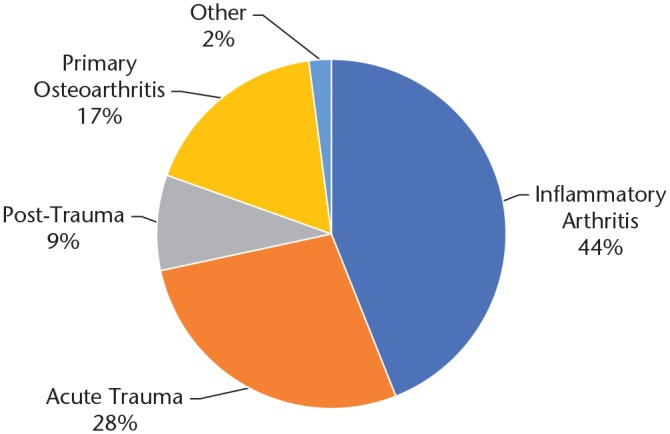
When comparing the time periods 2000–2009 and 2010–2017 there was a smaller proportion of TEAs performed for inflammatory arthritis (61% vs. 46%, p < 0.0001) and a larger proportion of TEAs performed for acute fracture (23% vs. 38%, p < 0.0001) and primary osteoarthritis (5% vs. 8%, p = 0.0004) (Fig. 2).
Fig. 2.
Indications for total elbow arthroplasty (Norway, New Zealand, Sweden).
When comparing geographical regions, the percentage of TEAs for primary osteoarthritis in Scandinavian countries (3%) was lower compared to other countries (27%) (p < 0.0001). Oceanic countries reported few post-traumatic-related indications for TEA (Australia 1%) or did not report post-traumatic sequelae at all (NZ) compared to 12% in the other countries (p < 0.0001).
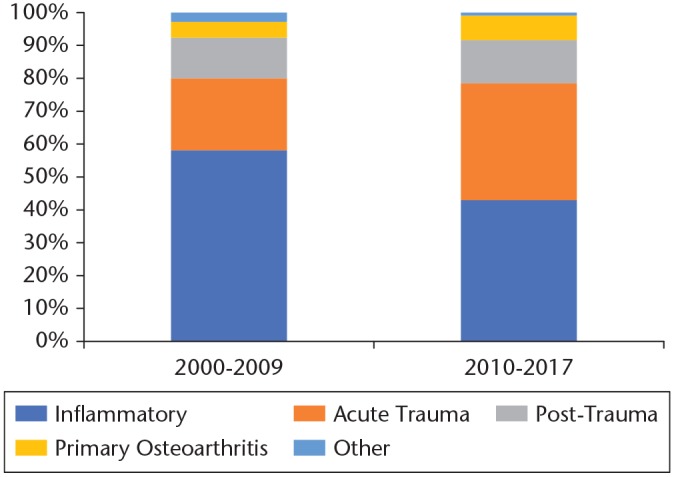
There was an increase in the number of revisions in all five registries that included elbow arthroplasty revision surgery individually (p < 0.05). When compiling data from all five of these countries for 2014–2017, an increase in the total amount of elbow revisions could also be identified from 105 in 2014, 124 in 2015, 174 in 2016 to 169 in 2017 (p = 0.003) (Fig. 3).
Fig. 3.
Revision elbow surgery.
Discussion
The purpose of this study was to assess the changes in indications for TEA over the last decade. We observed that the proportion of TEA cases performed for rheumatoid arthritis was smaller when comparing the time periods 2000–2009 and 2010–2017. This is possibly related to the increase in novel, successful non-surgical treatment options for rheumatoid arthritis, such as biologicals.14,15 The rise in acute fracture as an indication for TEA could be explained because some surgeons have espoused TEA as an option for fractures of the distal humerus due to the possibility of performing the procedure while leaving the extensor mechanism intact, leading to faster and easier rehabilitation when compared with internal fixation.16
We identified several differences between countries. The data suggest that European countries use more TEA than partial arthroplasties, while Australia reports much lower numbers of TEA surgeries compared to partial arthroplasties. A factor that could influence this number is the fact that hemi-arthroplasty is currently not approved by some regulatory offices such as the Food and Drug Administration in the United States, narrowing the options for affected radio-capitellar articulation down to conservative treatment, radial head resection, or TEA.17
We also identified differences in indications for TEA between geographical regions; Scandinavian countries reported notably fewer TEAs for osteoarthritis and Oceanic countries fewer TEA for post-traumatic indications. These differences could be explained by location-dependent factors such as surgeon trends, healthcare and insurance systems, and infrastructure.
Additionally, we identified an increasing trend in the incidence of elbow revision surgery. Considering that the population is staying active for longer and patients are therefore less inclined to adapt their lifestyle to a prosthesis with limitations, it is likely that this increasing trend will continue. This would create a larger demand for surgeons specialized in elbow revision surgery. The revision rate of TEA could not be compared because for most countries incidences were reported separately per year.
Advantages of this study include the large pool of data that was used, gathered from several countries, which diminished the biases a specific country or region might bring – such as insurances, local preferences, high- or low-volume centres – and therefore made the overview more generalizable to elbow surgery worldwide. With this large pool of international data, we were able to create a clear and accurate overview.
This review had several limitations. The collection of data was limited by the available reports from national registries, for example the Australian registry did not separately report data from each year. Registries reported the indication for TEA in different categories which made it difficult to generalize the outcomes, it would be desirable to streamline these categories as a step towards international co-operation, which could provide more and more accurate data. Data collection may differ between registries; therefore, it is difficult to make a comparison between registries. Only the UK and New Zealand used obligatory reporting, for the other registries reporting was not mandatory, which may compromise completeness of the data. However, all registries were validated with hospital records and completeness was assessed. Of the registries that reported completeness, none was below 90%. The only registry that did not report on completeness was from New Zealand, but this registry did have obligatory reporting. New Zealand and Sweden did not include hemi-arthroplasties, which may affect the assessment of indications for all elbow arthroplasties. It could be possible that this is a factor influencing the low rate of TEA for primary osteoarthritis in Scandinavia. However, the percentage of TEA for osteoarthritis was similar in Norway and Sweden (6% and 1%). Many national registries did not include elbow surgery. Though fewer in number compared to hip or knee surgery, data on TEA are essential to improve the outcome for this type of surgery. None of the registries made a distinction of outcomes between indications for surgery. This information could point out for which indications TEA is effective and could therefore contribute to decision making when considering TEA. Many registries included Patient Reported Outcome Measures (PROMs) for hip, knee and shoulder surgery, but only two included such outcome measures for elbow surgery. PROMs can be an effective tool to assess the success of an operation and should therefore be included in national registries where possible. Ideally, a single PROM score would be used in all registries to facilitate comparison between registries and possible contribution to an international registry. The Oxford Elbow Score (OES) or the Mayo Elbow Performance Index (MEPI) are popular PROMs, and the OES is used by the New Zealand registry for elbow outcomes.
Much information can be extracted from national registries. Nonetheless, there is improvement that could be made for comparison between registries. Several national registries are not publicly available, and increasing public accessibility of more registries would facilitate larger combined studies. The inclusion of elbow surgery in all national registries, complete and clear annual reporting, using the same categories for indications, reporting of outcome measures per indication and the inclusion of PROMs in registries could contribute greatly to the available knowledge and development of elbow surgery.
A valuable tool to optimize registry effectiveness and completeness could be the implementation of an electronic follow-up system such as the one used by Viveen et al.18 These improvements could also be the first steps towards an international registry such as the Nordic Arthroplasty Registry Association (NARA). NARA started as a collaboration between registries from Norway, Sweden and Denmark in 2007, Finland joined the association in 2010. A code set was defined for all parameters that the registries had in common, which allowed for the merger of data and comparison between countries. However, because only parameters and data that the registries had in common could be included, the merged registry contained fewer parameters and details.19 Since the foundation of NARA, several studies have been performed using the common database.20–25 Future collaboration between registries could consist of the merger of data to create larger databases. To avoid the problem of decreasing parameters and details when adding more registries other options can be explored. When applying a universal coding system and universal access without compiling data, the integrity of national registries would be preserved while allowing studies to be performed on specific parameters, including only those registries that specify the parameters needed for a particular study. Another option would be to convince as many registries as possible to start adopting universal categories of parameters, thereby increasing the possibility of collaboration without decreasing the total number of parameters. However, questions could be raised about the feasibility of this option as some countries might have to make changes in their diagnostic and reporting systems.
Conclusion
We performed a systematic review of six national registries including a total of 6544 TEAs. We found that the range of indications for TEA is broadening, with TEA for acute trauma and osteoarthritis becoming increasingly more common. However, inflammatory arthritis remains the most common indication for TEA in recent years. When comparing geographical regions, we conclude that Scandinavian countries report fewer TEAs for osteoarthritis and Oceanic countries fewer for post-traumatic sequelae. We also observed an increase in the incidence of revision surgery.
Footnotes
ICMJE Conflict of interest statement: NCC reports consultancy for Miami Device Solutions; fellowship support for OMeGA, Acumed and Skeletal Dynamics; research funding from Acumed, AO International and DePuy Synthes.
DE reports consultancy for Lima corporates, has given paid presentations for A.O. and Stryker and received institutional support from Matthys, Zimmer-Biomet and Stryker.
The other authors declare no conflict of interest relevant to this work.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated.
References
- 1. Prkić A, van Bergen CJ, The B, Eygendaal D. Total elbow arthroplasty is moving forward: review on past, present and future. World J Orthop 2016;7:44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Marsh JP, King GJW. Total Elbow Arthroplasty. Oper Tech Orthop 2013. 10.1053/j.oto.2013.09.002 (date last accessed 9 September 2019). [DOI]
- 3. National Joint Registry for England Wales and Northern Ireland. 13th Annual Report 2016. 2016. 10.1017/CBO9781107415324.004 (date last accessed 9 September 2019). [DOI]
- 4. Sanchez-Sotelo J, Baghdadi YMK, Morrey BF. Primary linked semiconstrained total elbow arthroplasty for rheumatoid arthritis: a single-institution experience with 461 elbows over three decades. J Bone Joint Surg Am 2016;98:1741–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Perretta D, van Leeuwen WF, Dyer G, Ring D, Chen N. Risk factors for reoperation after total elbow arthroplasty. J Shoulder Elbow Surg 2017;26:824–829. [DOI] [PubMed] [Google Scholar]
- 6. Chafik D, Lee T, Gupta R. Total elbow arthroplasty: current indications, factors affecting outcomes, and follow-up results. Am J Orthop (Belle Mead NJ) 2004;33:496–503. [PubMed] [Google Scholar]
- 7. Rasmussen JV, Olsen BS, Fevang BTS, et al. A review of national shoulder and elbow joint replacement registries. J Shoulder Elbow Surg 2012;21:1328–1335. [DOI] [PubMed] [Google Scholar]
- 8. UK National Joint Registry. 14th Annual Report: National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Natl Jt Regist 2016. https://doi.org/http://www.njrreports.org.uk/Portals/0/PDFdownloads/NJR%2014th%20Annual%20Report%202017.pdf (date last accessed 9 September 2019).
- 9. Australian Orthopaedic Association. Australian Orthopaedic Association National Joint Replacement Registry; Hip, Knee & Shoulder Arthroplasty: annual report 2017. Adelaide, South Australia, Australia, Australian Orthopaedic Association, 2017. [Google Scholar]
- 10. Norwegian National Advisory Unit on Arthroplasty and Hip Fractures. Norwegian Arthroplasty Registry: 2018 report. Haukeland: Norwegian National Advisory Unit on Arthroplasty and Hip Fractures, 2018. [Google Scholar]
- 11. New Zealand Orthopaedic Association. New Zealand Orthopaedic Association, annual report 2018. https://nzoa.org.nz/system/files/DH8131_NZOA_AnnualReport2018_v7_7Nov18.pdf (date last accessed 9 September 2019).
- 12. Dutch Arthroplasty Register. Dutch Arthroplasty Register, annual report 2018. http://www.lroi-rapportage.nl/media/pdf/PDFOnline_LROI_annual_report_2018.pdf (date last accessed 9 September 2019).
- 13. Svenska Skulder och Armbagssallskapet. Svenska Skulder och Armbågsregistret, ÅRSRAPPORT 2018. http://ssas.se/files/docs/rapp18.pdf (date last accessed 9 September 2019).
- 14. Prkic A, Welsink C, The B, van den Bekerom MPJ, Eygendaal D. Why does total elbow arthroplasty fail today? A systematic review of recent literature. Arch Orthop Trauma Surg 2017;137:761–769. [DOI] [PubMed] [Google Scholar]
- 15. Burmester GR, Pope JE. Novel treatment strategies in rheumatoid arthritis. Lancet 2017;389:2338–2348. [DOI] [PubMed] [Google Scholar]
- 16. Harmer LS, Sanchez-Sotelo J. Total elbow arthroplasty for distal humerus fractures. Hand Clin 2015;31:605–614. [DOI] [PubMed] [Google Scholar]
- 17. Bachman D, Cil A. Current concepts in elbow arthroplasty. EFORT Open Rev 2017;2:83–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Viveen J, Prkic A, The B, Koenraadt KL, Eygendaal D. Effect of introducing an online system on the follow-up of elbow arthroplasty. World J Orthop 2016;7:826–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Havelin LI, Robertsson O, Fenstad AM, Overgaard S, Garellick G, Furnes O. A Scandinavian experience of register collaboration: the Nordic Arthroplasty Register Association (NARA). J Bone Joint Surg Am 2011;93:13–19. [DOI] [PubMed] [Google Scholar]
- 20. Robertsson O, Bizjajeva S, Fenstad AM, et al. Knee arthroplasty in Denmark, Norway and Sweden: a pilot study from the Nordic Arthroplasty Register Association. Acta Orthop 2010;81:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pedersen AB, Mehnert F, Havelin LI, et al. Association between fixation technique and revision risk in total hip arthroplasty patients younger than 55 years of age: results from the Nordic Arthroplasty Register Association. Osteoarthr Cartil 2014;22:659–667 [DOI] [PubMed] [Google Scholar]
- 22. Springer BD, Cahue S, Etkin CD, Lewallen DG, McGrory BJ. Infection burden in total hip and knee arthroplasties: an international registry-based perspective. Arthroplast Today 2017;3:137–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dale H, Fenstad AM, Hallan G, et al. Increasing risk of prosthetic joint infection after total hip arthroplasty. Acta Orthop 2012;83:449–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Glassou EN, Hansen TB, Mäkelä K, et al. Association between hospital procedure volume and risk of revision after total hip arthroplasty: a population-based study within the Nordic Arthroplasty Register Association database. Osteoarthritis Cartilage 2016;24:419–426. [DOI] [PubMed] [Google Scholar]
- 25. Rasmussen JV, Hole R, Metlie T, et al. Anatomical total shoulder arthroplasty used for glenohumeral osteoarthritis has higher survival rates than hemiarthroplasty: a Nordic registry-based study. Osteoarthritis Cartilage 2018;26:659–665. [DOI] [PubMed] [Google Scholar]