Abstract
End-stage osteoarthritis is commonly treated with joint replacement. Despite high clinical success rates, up to 28% of patients are dissatisfied with the outcome.
This best-evidence synthesis aimed to review studies with different forms of study design and methodology that examined the relationship between (fulfilment of) outcome expectations of hip and knee patients and satisfaction with outcome.
A literature search was performed in PubMed, Web of Science, PsycInfo, Cochrane, and Google Scholar to identify studies conducted up to November 2017. The methodological quality of studies was assessed using the Newcastle-Ottawa Scale.
In this best-evidence synthesis systematic review, the following main results could be seen. In only half of all studies were preoperative expectations associated with level of satisfaction, while in almost all studies (93%), fulfilment of expectations was related to satisfaction. The effect of met expectations did not differ between hip and knee patients or study design.
Fulfilment of expectations seems to be consistently associated with patient satisfaction with outcome. Emphasis in future research must be placed on the operationalization and measurement of expectations and satisfaction to determine the (strength of the) influence of these different forms of assessment on the (existence of the) relationship.
Cite this article: EFORT Open Rev 2020;5:226-240. DOI: 10.1302/2058-5241.5.190015
Keywords: expectations, fulfilment, PROMS, satisfaction, THA, TKA
Introduction
Osteoarthritis (OA) is the most common chronic joint disease, leading to limitations in activities of daily living (ADL).1–3 Joint replacement is a commonly used treatment in orthopaedics for end-stage OA.4–9 The risk of complications with joint replacement is usually low and clinical success rates are high.6,7,9 Up to 90% of patients improve in function after the replacement of the affected joint.5 However, up to 30% of all patients report some degree of dissatisfaction with the results of the replacement of the knee (i.e. total knee arthroplasty; TKA) or hip (i.e. total hip arthroplasty; THA).4,10–14
Dissatisfaction with the results of surgery could concern, for example, dissatisfaction with improvement in pain or function resulting from medical interventions.15 Dissatisfaction with these outcomes has been found to result in nonadherence with medication and advice and delayed or insufficient physical improvement.16,17 This type of dissatisfaction is commonly examined with the reliable and validated self-administered Patient Satisfaction Scale,18 and thereby refers to overall satisfaction with surgery, with pain relief, and with the ability to perform work and recreational activities.19–22 Some studies have indicated that low satisfaction with outcomes of treatment might be related to high preoperative expectations,23,24 as it is found that patients commonly have very optimistic expectations about the results of surgery.23–26 Nonetheless, other studies reported no relationship between preoperative expectations and patient satisfaction,21,24,27 and some found that fulfilment of these expectations, rather than expectations themselves, could lead to satisfaction.13,22,25,26 In fact, fulfilment of expectations was the most important factor linked with post-surgery satisfaction in several studies.22,25,28
Patients’ outcome expectations particularly concern a belief or anticipation that certain actions (i.e. surgery) will achieve particular outcomes.29–31 Postoperative fulfilled expectations, however, concern a consideration of whether surgery did achieve particular outcomes, that is, whether expectations have been met.32 Although these concepts are clearly defined, assessment of these outcome expectations could focus on all different kinds of outcomes, such as, for example, general improvement,10,33–35 or more specific pain level,36–38 or functioning.26,36,38 The Hospital for Special Surgery Hip (Fulfilment) Replacement Expectations Survey (HSS-H(F)RES)33 or the Hospital for Special Surgery Knee (Fulfilment) Replacement Expectations Survey (HSS-K(F)RES)39 are questionnaires commonly used to assess (fulfilled) expectations in THA and TKA patients, as they examine a broad range of possible outcomes on a continuous scale (i.e. the level of satisfaction) rather than a binary scale (i.e. expectations yes/no).20,25,32,40,41
Based on the literature, it is still not clear whether preoperative expectations or the level of fulfilled expectations are related to patient satisfaction with outcome after surgery. This may be due to differences in methodology. For instance, studies varied in the operationalization (i.e. the precise description of a concept to make it measurable, using, for example, questionnaires) of patients’ outcome expectations and satisfaction with outcome. In addition, conflicted findings could have resulted from differences in study design. Specifically, while multiple studies found no relationship between preoperative expectations and satisfaction,36,38,42 when examining it prospectively, one known study reported a relationship between expectations and satisfaction when examining preoperative expectations retrospectively.33 Differences in study design might explain the relationship between postoperative expectations and satisfaction, as patients’ recall of expectations might have changed due to the surgery and recovery process.43,44 Moreover, emphasis in research is predominantly placed on TKA patients instead of THA patients.11,22,26,44 Yet, satisfaction in THA patients could be low and determined by (fulfilment of) expectations as well.4,8 Furthermore, few studies have examined (differences in) satisfaction and effects of expectations between TKA and THA patients, although there might be a variation in short-term and long-term satisfaction between these patient groups. For example, THA patients are often more satisfied and usually recover faster and to a larger extent than TKA patients,4,8,45 even though function seems to return to the same level for both patient groups after six months.4
Several previously published systematic reviews have examined the relationship between preoperative expectations and satisfaction in orthopaedic patients.31,44,46–49 Nonetheless, most of the systematic reviews did not include all relevant studies,31,46,49 and they rarely focused on fulfilment of these expectations,44,47,48 or only on the relationship in TKA patients and not in THA patients.31,47 Moreover, only one single systematic review examined the influence of differences in methodology.49 This study therefore aims to systematically review all studies that have been performed on the relationship between (fulfilment of) expectations and satisfaction with outcome in TKA and THA patients, in order to determine what connection (fulfilled) expectations and satisfaction with outcome have in these patient groups. A best-evidence synthesis will be used and recommendations for future research and implications for clinical practice will be made.
Materials and methods
In accordance with the PRISMA guidelines, this systematic review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 10 February 2017 (registration number: CRD42017052851).
Search strategy
An electronic literature search was performed in PubMed, Web of Science, PsycInfo, Cochrane, and Google Scholar to identify eligible studies published in English or Dutch up to the end of October 2017. Search terms were developed using MeSH terms and consisted of text words related to (1) knee arthroplasty and/or hip arthroplasty, (2) expectations or expectancies, and (3) satisfaction (Table 1). The terms ‘expectations’ and ‘expectancies’ are both used in the literature to indicate that someone is ‘expecting something for the future’. As Haanstra et al stated, expectancies could be defined as ‘the act or state of expecting’ and expectations as ‘cognitions regarding probable future events’.31 Although different concepts, the existing literature was followed and no distinction was made between these two terms.
Table 1.
Search strategy for each database.
| Database | Search terms | Date of search | 2nd date of search | 3rd date of search |
|---|---|---|---|---|
| PubMed | ((((((((((((((“tka") OR "tha") OR "total knee arthroplasty") OR "total hip arthroplasty") OR "hip replacement") OR "knee replacement") OR "tkr") OR "thr") OR "joint replacement") OR "joint prosthesis") OR "knee prosthesis") OR "hip prosthesis")) AND ((("pre operative expectations") OR "post operative expectations") OR "expectations")) AND (("satisfaction") OR "satisfied") | 3-10-2016 | 10-4-2017 | 30-10-2017 |
| Cochrane library | #1 "TKA":ti,ab,kw or "THA":ti,ab,kw or "total knee arthroplasty":ti,ab,kw or "total hip arthroplasty":ti,ab,kw #2 joint prosthesis:ti,ab,kw or knee prosthesis:ti,ab,kw or hip prosthesis:ti,ab,kw #3 hip replacement:ti,ab,kw or knee replacement:ti,ab,kw or joint replacement:ti,ab,kw #4 expectations:ti,ab,kw or expectancies:ti,ab,kw #5 satisfaction:ti,ab,kw or satisfied:ti,ab,kw #6: #1 or #2 or #3 and #4 and #5 |
3-10-2016 | 10-4-2017 | 30-10-2017 |
| Google Scholar | expectations AND satisfaction THA OR TKA OR "Total knee arthroplasty" OR "total hip arthroplasty" OR "joint prosthesis" OR "knee prosthesis" OR "hip prosthesis" OR "hip replacement" OR "knee replacement" OR "joint replacement" | 3-10-2016 | 10-4-2017 | 30-10-2017 |
| Web of Science | #1: TS=(tka) OR TS=(tha) OR TS=(total knee arthroplasty) OR TS=(total hip arthroplasty) OR TS=(hip replacement) OR TS=(knee replacement) OR TS=(tkr) OR TS=(thr) OR TS=(joint replacement) OR TS=(joint prosthesis) OR TS=(knee prosthesis) OR TS=(hip prosthesis) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan=All years #2: TS=(pre operative expectations) OR TS=(post operative expectations) OR TS=(expectations) OR TS=(expectancies) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan=All years #3: TS=(satisfaction) OR TS=(satisfied) OR TS=(dissatisfaction) OR TS=(dissatisfied) OR TS=(satisfy*) OR TS=(dissatisfy*) #4: #1 AND #2 AND #3 |
3-10-2016 | 10-4-2017 | 30-10-2017 |
| PsycInfo | AB ( tka OR tha OR total knee arthroplasty OR total hip arthroplasty OR hip replacement OR knee replacement OR tkr OR thr OR joint replacement OR joint prosthesis OR knee prosthesis OR hip prosthesis ) AND AB ( pre operative expectations OR post operative expectations OR expectations OR expectancies ) AND AB ( satisfaction OR satisfied OR dissatisfaction OR dissatisfied OR satisf* OR dissatisf* | 3-10-2016 | 10-4-2017 | 30-10-2017 |
Eligibility criteria
The search results of all separate databases were combined, after which duplicates were removed (see Fig. 1). Titles and abstracts of the remaining articles were screened against the inclusion criteria. Full-text articles were assessed when, based on the abstract, they either appeared to meet the inclusion criteria, or it was unclear whether they met the criteria. Studies were found eligible and were included when meeting the following criteria: (1) the study included TKA and/or THA patients, (2) preoperative outcome expectations and/or postoperative fulfilled outcome expectations were measured, (3) satisfaction with outcome of treatment was measured, (4) the primary or secondary objective of the study was to evaluate the relationship between expectations and satisfaction with outcome of treatment, and (5) data on the relationship between expectations and satisfaction with outcome of treatment in TKA and/or THA patients were available in the study. OA is the most common indication for a total knee or hip replacement. However, studies including other conditions (e.g. avascular necrosis or rheumatoid arthritis) leading to TKA or THA were also included, as we were interested in the effects of TKA and THA and not of the underlying disease. Studies examining patients with revision TKA or THA were also included, as the aim of the study was not to examine levels of expectations (which could have been different in revision surgery), but to examine the relationship between expectations and satisfaction.
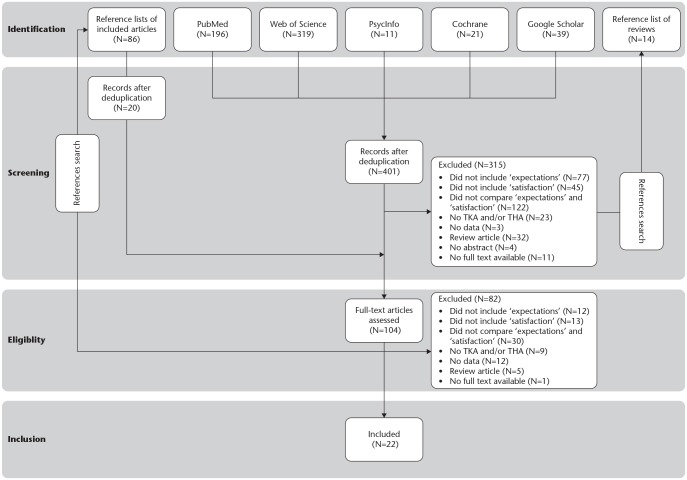
Fig. 1.
Flowchart of study selection.
Note. TKA, total knee arthroplasty; THA, total hip arthroplasty.
If a study examined TKA and/or THA patients in combination with other patient groups, yet did not report data on the different patient groups, the study was excluded, as we would otherwise be unable to make a distinction between the differences in patient groups. In line with the aims of our study, we chose to examine only studies that assessed satisfaction with outcome, and therefore excluded studies examining, for example, satisfaction with care, satisfaction with received information, and satisfaction with treatment choice. In addition, we chose to only examine studies which assessed outcome expectations, and not, for example, self-efficacy beliefs, or expectations about the process of treatment.29,31 Even though outcome expectations and satisfaction with outcome could be operationalized in different ways, we chose to include all studies that examined these concepts, regardless of the operationalization of these concepts.
Data extraction
Data were extracted from the included studies using a standardized extraction form (Table 2). If multiple articles had been written on the same dataset, only the most recent study was included. When a study included both TKA and THA patients, a comparison was made between these different patient groups. If no data on the different groups were available, authors were contacted to ask whether they had data on the different subgroups and, if so, to forward it. In addition, comparisons were also made between studies examining preoperative expectations with a retrospective and with a prospective design.
Table 2.
Characteristics of included studies.
| Author, year | TKA/THA | N | Follow-up | Age | Operationalization of expectations | Study design/ measurement level | % fulfilled | % patients with fulfilled expectations | Operationalization of satisfaction | Measurement level | % satisfied patients |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Anakwe et al, 201112 | TKA | 850 | 1 yr | 68 | One question about fulfilment of expectations, n.s. | 4-point Likert scale | n/a | n/a | One question concerning satisfaction with the results of surgery. Additionally: a rating of the pain relief that is achieved, a rating of the success of operation in performance on heavy lifting, the likelihood of recommendation of the operation to a friend, willingness to have operation again, rating of the hospital. |
4–5-point Likert scale | 93.0% |
| Arden et al, 201136 | THA | 639 | 2 yrs | 68 | Preoperative questionnaire with questions about: expectations for postoperative pain and limitations in usual activities | Prospective 3–4-point Likert scale |
One question about level of satisfaction with the result of the hip replacement. | Binary (satisfied vs. dissatisfied) | 92.8% | ||
| Bourne et al, 201011 | TKA | 1708 | 1 yr | 69 |
Fulfilment of expectations, n.s. Additionally: willingness to have surgery again |
n.s. | n/a | n/a | Three questions concerning: satisfaction with the results of the knee replacement, satisfaction with pain reduction, and satisfaction with the ability to perform five functions (going up stairs, getting in/out of a car/bus, rising from bed, lying in bed, performing light domestic duties). | 5-point Likert scale | 81.0% |
| Clement et al, 201540 | TKA | 322 | 1 yr | 71 | Fulfilment of HSS-KFRES39 | 5-point Likert scale | n/a | 56% | One question about level of satisfaction with the operated knee. | 4-point Likert scale | 86.0% |
| Eisler et al, 200237 | THA | 98 | 1 yr | 70 | Two questions about fulfilment of expectations with future pain, and walking ability | 4-point Likert scale | n/a | 55–69% | A grading of overall satisfaction. | 6-point Likert scale | 63.0% |
| Gandhi et al, 200942 | TKA THA |
1799 | 1 yr | 69–74 | Three questions regarding preoperative expectations about: time to fully recover, level of postoperative pain, and ability to perform usual activities | Prospective Responses collapsed into 3-point Likert scale |
One question about level of satisfaction the results of the surgery. | Binary (satisfied vs. dissatisfied) | 93.0–95.0% | ||
| Hamilton et al, 201310 | TKA THA |
4709 | 1 yr | 70 70 |
One questions about fulfilment of expectations, n.s. | 6-point Likert scale | n/a | n/a | One question with a rating of overall satisfaction with operated hip or knee. |
4–6-point Likert scale | 86.6% |
| Additionally, questions about: pain relieve after surgery, improvement in ability to perform regular activities, performance of heavy work or sport activities, rating of overall hospital experience, willingness to have operation again, the likelihood of recommendation of the operation to a friend. | |||||||||||
| Jain et al, 201719 | THA | 207 | 6 mo | 65 | Preoperative expectations: HSS-HRES33 | Prospective 5-point Likert scale |
The Self-Administered Patient Satisfaction Scale.32 | 4-point Likert scale | 94.5% | ||
| Jain et al, 201720 | TKA | 83 | 1 yr | 70 | Fulfilment of HSS-KFRES39 | 5-point Likert scale | 76.7% | n/a | The Self-Administered Patient Satisfaction Scale.32 | 4-point Likert scale | 92.3% |
| Kiran et al, 201538 | TKA | 365 | 2 yr | 72 | Two preoperative questions about expectations with: limitations in usual activities, pain after recovery | Prospective 4-point Likert scale |
One question concerning satisfaction with the result of the knee replacement. Additionally, three questions regarding: improvement in overall function, reduction of pain, reduction of pain medication. |
Binary (satisfied vs. dissatisfied) | 83.8% | ||
| Lim et al, 201534 | TKA THA |
3488 | > 2 yr | 67 61 |
One question regarding: fulfilment of patient’s expectations, n.s. | 7-point Likert scale | n/a n/a |
95.6% 94.9% |
Rating of overall results of surgery. | 6-point Likert scale | 90.5% 91.9% |
| Lingard et al, 200621 | TKA | 525 | 1 yr | 69 | Four preoperative questions about expectations for: pain level, walking distance, limitation of recreational activity, and use of a walking aid | Prospective 5-point Likert scale |
The Self-Administered Patient Satisfaction Scale.32
Additionally, two questions about performance after surgery and willingness to have the same surgery again. |
4-point Likert scale | n/a | ||
| Mancuso et al, 199733 | THA | 180 | 2–3 yr | 65 | Two preoperative questions about: expectations of surgery and hopes | Retrospective Open-ended questions |
Three questions concerning: willingness to have operation again, meeting expectations, overall satisfaction with the results of hip arthroplasty. | Open-ended | 89.0% | ||
| Mancuso et al, 200941 | THA | 405 | 6 yr | 66 | Fulfilment of HSS-HFRES33 | 5-point Likert scale | 87% | 75% | One question: ‘If you were to spend the rest of your life with your hip symptoms just the way they have been in the last 24 hours, how would you feel?’ | 7-point Likert scale | 94.0% |
| Mannion et al, 200924 | TKA | 112 | 2 yr | 67 | Questions concerning fulfilment of expectations about: time to full recovery, pain after recovery, and limitations in everyday activities after recovery | Open-ended, Likert scale | n/a | 30% / 47% | One question about satisfaction with surgery, n.s. | 4-point Likert scale | 90.1% |
| Noble et al, 200626 | TKA | 253 | 1 yr | 68 | One question about fulfilment of expectation concerning level of activity | Binary (fulfilled vs. not fulfilled) | n/a | n/a | One question about satisfaction with knee replacement. | Binary (satisfied vs. dissatisfied) | 75.0% |
| Palazzo et al, 201425 | THA | 132 | > 1 yr | 64 | Fulfilment of HSS-HFRES33 | 5-point Likert scale | 73.1% | n/a | One question: ‘If you were to spend the rest of your life with your hip symptoms just the way they have been in the last 24 hours, how would you feel?’ | 7-point Likert scale | 91.9% |
| Scott et al, 201022 | TKA | 1141 | 1 yr | 70 | One question about fulfilment of expectations, n.s. | 6-point Likert scale | n/a | n/a | The Self-Administered Patient Satisfaction Scale.32 | 4–6-point Likert scale | 81.4% |
| Scott et al, 201232 | TKA THA |
669 | 1 yr | 69 71 |
Fulfilment of HFSS-KRES39
Fulfilment of HFSS-HRES33 |
5-point Likert scale | 59% 72% |
10% 21% |
One question about satisfaction with the operated hip/knee. | 4-point Likert scale | 78.0% 88.0% |
| Gonzalez Saenz de Tejada et al, 201454 | TKA THA | 892 | 1 yr | 69 | Adapted version of HSS-KRES39/HSS-HRES33 (preoperative expectations) | Prospective 5-point Likert scale |
One question: ‘If you were to spend the rest of your life with your hip symptoms just the way they have been in the last 24 hours, how would you feel?’ | 4-point Likert scale | n/a | ||
| Thambiah et al, 201528 | TKA | 103 | > 1 yr | 64 | Questionnaire assessing preoperative expectations about: improved mobility, reduced pain and better overall quality of life | Prospective n.s. |
One question examining overall patient satisfaction. In addition, two questions about recommendations to others and willingness to undergo surgery again. |
5-point Likert scale | 92.8% | ||
| Vissers et al, 201035 | TKA | 44 | 6 mo | 64 | Four questions about fulfilment of expectations regarding: pain after surgery, limitations of activities of daily living after surgery, the overall success of the operation and likeliness of having complications | 4-point Likert scale | n/a | n/a | One question about satisfaction with results of surgery. | 5-point Likert scale | 72.7% |
Note. TKA, total knee arthroplasty; THA, total hip arthroplasty; HSS-K(F)RES, Hospital for Special Surgery Knee (Fulfilment) Replacement Expectations Survey; HSS-H(F)RES, Hospital for Special Surgery Hip (Fulfilment) Replacement Expectations Survey.
Quality assessment
The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses was used to assess the methodological quality of studies.50 The NOS assesses studies on three different constructs (selection, comparability and exposure/outcome), with eight questions on which studies could score a maximum of nine points in total (i.e., four points for selection, two points for comparability and three points for exposure/outcome) . Studies with a score of six or more points on the NOS were regarded as qualitatively good.51 In order to assure objective assessment, the quality assessment was independently conducted by two researchers. In case of disagreement between reviewers, points of disagreement were discussed in order to reach consensus.
Statistical analysis
A comparison was made between TKA and THA patients in terms of fulfilled expectations and satisfaction. All studies were compared based on average percentages of fulfilled expectations or as percentages of patients who were satisfied, or had all their expectations fulfilled, calculated as a weighted average across all studies examining respectively TKA or THA patients. The number of participants in studies with no separated data on TKA and THA patients were equally split between TKA and THA patients.
Data synthesis
Due to study heterogeneity, it was impossible to synthesize the data in a meta-analysis. An alternative to meta-analysis is the best-evidence synthesis, in which studies are classified based on level of internal and external validity.51 Studies were identified as ‘strong/high quality’ when receiving 6 to 9 points on the NOS. Studies were identified as moderate quality or weak quality when receiving respectively 4 or 5, or 1 to 3 points.51
Studies were classified as either reporting a significant relationship between (fulfilment of) expectations and satisfaction or as reporting no significant relationship between these concepts based on their own findings and conclusions. Statistical values were, when reported, included in our systematic review. The levels of evidence regarding the significance or non-significance of a relationship among studies were ranked according to the following statements: (1) strong evidence: consistent findings (> 75% of the studies reported consistent findings) in multiple high-quality studies; (2) moderate evidence: consistent findings (> 75% of the studies reported consistent findings) in one high-quality study and two or more moderate-quality studies, or in three or more weak-quality studies, (3) limited evidence: generally consistent findings (> 75% of the studies reported consistent findings) in a high-quality study or in two or fewer moderate-quality studies, (4) no evidence: no studies could be found, (5) conflicting evidence: conflicting findings.52
Results
Study selection process
The search resulted in 586 records. After the removal of 185 duplicates, 401 unique studies were screened (see Fig. 1). Based on abstract and title, 315 articles were excluded. The reference lists of included articles and existing relevant reviews were scanned for additional articles. Another 82 articles were excluded after full-text assessment, leaving a remaining 22 included articles.
Study characteristics
Twenty (90.9%) cohort studies and two cross-sectional studies26,33 (9.1%) were included in this review (Table 2). One of the cohort studies was labelled as a cross-sectional study,11 yet this study included multiple follow-up periods with multiple assessments within the same patients, so we considered it a prospective cohort study. Only one study examined revision surgery, instead of primary TKA or THA.37
Expectations
The operationalization of expectation and satisfaction was quite diverse across studies (see Table 2). However, the majority used the HSS-K(F)RES or HSS-H(F)RES 39,53 or an adaptation of these scales (seven studies) or assessed fulfilment of expectations with one single question (six studies) (Table 2). Others focused on hopes or expectations regarding, for instance, limitations in daily living, pain and walking ability. Some studies examined the number of expectations patients have,24,33 while others assessed the level of patients’ expectations,21,38,42 or a combination, in relationship with satisfaction.19,20,25,32,40,41,54 For example, scores on the HSS-H(F)RES or HSS-K(F)RES represent the combined amount of (fulfilled) expectations the patient has and the level of these (fulfilled) expectations.39,53
Studies examining fulfilment of expectations either asked patients how many expectations were fulfilled,20,25,32 or simply examined whether their expectations were fulfilled (yes/no).24,32,34,37,40,41 Even though in the majority of studies examining fulfilment of expectations patients were also asked about their preoperative expectations prospectively (9/14), 13 of the 14 fulfilment studies (93%) did not compare preoperative expectations with postoperative fulfilment. In only one study patients were told what expectations they had cited before and asked how they were now fulfilled.34
Satisfaction
Satisfaction with outcome was mostly examined with one question assessing overall satisfaction or satisfaction with the results of surgery (11 studies). Four studies asked questions about satisfaction with results of surgery, pain relief, and success of operation in increasing home/yard and recreational activities (i.e. the Patient Satisfaction Scale).18 Others focused on, for example, likelihood of recommendation of surgery, the willingness to have surgery again and a rating of the hospital as a measure of satisfaction with outcome. Four studies assessed satisfaction with: a rating of the results of surgery34 or asked patients the question ‘If you were to spend the rest of your life with your hip symptoms just the way they have been in the last twenty-four hours, how would you feel?’.25,41,54 Percentages are reported for the dichotomized proportion of patients that is classified as being satisfied with the results of surgery as compared to the proportion of patients that is classified as being dissatisfied with the results of surgery (Table 2).
Methodical quality
Initially, scores on 12 items (6%) differed between the two reviewers. Disagreement was dissolved by consensus. The mean quality score was 6 out of 9 (range 4–9) (Table 3). A common methodological flaw was the lack of control for important demographic or clinical factors, or other important correlates of satisfaction. Other methodological shortcomings were the lack of description of number of patients who were lost to follow-up, or too large a number of patients (i.e. > 20%) lost to follow-up, and the absence of a description or operationalization of satisfaction.
Table 3.
Quality assessment with Newcastle-Ottawa Scale.
| Author, year | Selection | Comparability | Outcome | Total | Quality |
|---|---|---|---|---|---|
| Anakwe et al, 201112 | • • | • • | • • • | 7 / 9 | High |
| Arden et al, 201136 | • • | • • | • • • | 7 / 9 | High |
| Bourne et al, 201011 | • • | • • | • • • | 7 / 9 | High |
| Clement et al, 201540 | • • | • | • • • | 6 / 9 | High |
| Eisler et al, 200237 | • • | • | • • • | 6 / 9 | High |
| Gandhi et al, 200942 | • • | • • | 4 / 9 | Moderate | |
| Hamilton et al, 201310 | • • | • • | • • | 6 / 9 | High |
| Jain et al, 201720 | • • • | • • | • • • | 8 / 9 | High |
| Jain et al, 201719 | • • | • • | • • • | 7 / 9 | High |
| Kiran et al, 201538 | • • | • • | • • | 6 / 9 | High |
| Lim et al, 201534 | • • | • • | • • | 6 / 9 | High |
| Lingard et al, 200621 | • • | • • | • • • | 7 / 9 | High |
| Mancuso et al, 199733 | • • | • • | • • | 6 / 9 | High |
| Mancuso et al, 200941 | • • | • | • | 4 / 9 | Moderate |
| Mannion et al, 200924 | • • | • • | • • | 6 / 9 | High |
| Noble et al, 200626 | • • | • • | • • | 6 / 9 | High |
| Palazzo et al, 201425 | • • | • • | • • | 6 / 9 | High |
| Scott et al, 201022 | • • | • • | • • • | 7 / 9 | High |
| Scott et al, 201232 | • • | • • • | 5 / 9 | Moderate | |
| Gonzalez Saenz de Tejada et al, 201454 | • • | • • | • • | 6 / 9 | High |
| Thambiah et al, 201528 | • • | • • | • • | 6 / 9 | High |
| Vissers et al, 201035 | • • | • • | • • • | 7 / 9 | High |
Note. Each study could score a maximum of nine points in total (i.e. four points for selection, two points for comparability and three points for exposure/outcome). Studies with a score of six or more points were regarded as qualitatively good.
Expectations and satisfaction
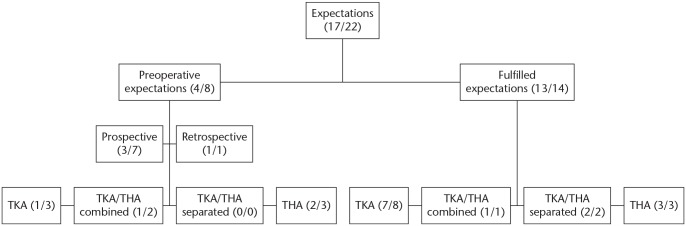
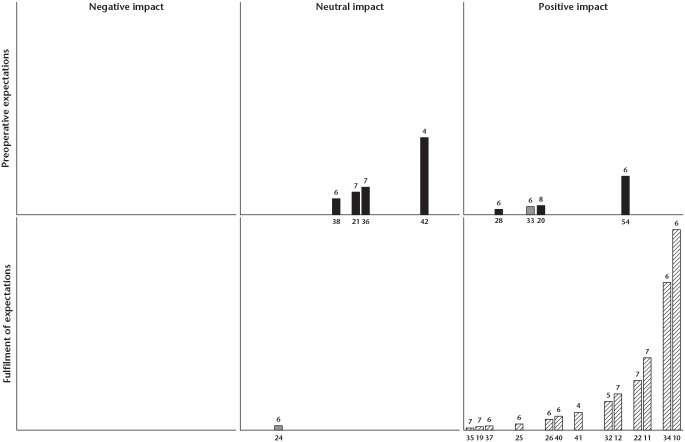
Overall, 17 out of 22 (77%) studies found a significant positive relationship between preoperative expectations or fulfilment of expectations and satisfaction (Table 4, Fig. 2, Fig. 3). Moreover, 13 out of the 14 studies assessing fulfilment of expectations reported a significant association with satisfaction (93%) (Fig. 2, Fig. 3). As such, according to our best-evidence synthesis, strong evidence was found that fulfilled expectations were positively related to satisfaction after surgery. Only four out of eight studies examining preoperative expectations reported a significant association with satisfaction (50%) (Fig. 2, Fig. 3). Therefore, according to the guidelines, conflicting evidence was found for a positive link between preoperative expectations and satisfaction.
Table 4.
Conclusions about relationship between expectations and satisfaction of included studies.
| Author, year | Sig. | Conclusions | Statistics |
|---|---|---|---|
| Anakwe et al, 201112 | Yes | A significant positive correlation between fulfilment of expectations and overall satisfaction | r = .65, p ≤ .001 |
| Arden et al, 201136 | No | Preoperative expectations did not influence level of satisfaction at 12 months or 24 months post surgery | p = .17 p = .96 |
| Bourne et al, 201011 | Yes | Univariate statistical analysis showed that a significant difference existed between patients with met and unmet expectations in terms of satisfaction | OR = 10.7, p ≤ .001 |
| Clement et al, 201540 | Yes | 16 of 17 met expectations were significantly associated with higher satisfaction | OR ≥ 7.9, p ≤ .08 |
| Eisler et al, 200237 | Yes | Fulfilled expectations about pain and walking ability were moderately positively correlated with satisfaction |
r = .47 r = .46 |
| Gandhi et al, 200942 | No | No differences in satisfaction were found between patients with high, moderate or low expectations | p = .92 p = .62 p = .28 |
| Hamilton et al, 201310 | Yes | Meeting patient expectations was significantly positively correlated with higher satisfaction | r = .74, p ≤ .001 |
| Jain et al, 201720 | Yes | Preoperative expectations were positively associated with higher satisfaction at six months | b = .17, p ≤.001 |
| Jain et al, 201719 | Yes | More fulfilment of expectations is related to higher satisfaction | r2 = .29, p ≤ .001 |
| Kiran et al, 201538 | No | Preoperative expectations did not correlate with satisfaction | n/a |
| Lim et al, 201534 | Yes | At two-year follow-up, met expectations were significantly associated with satisfaction | OR = 105.3, p ≤ .001 |
| Lingard et al, 200621 | No | Satisfaction was not associated with level of preoperative expectations | n/a |
| Mancuso et al, 199733 | Yes | A strong positive correlation was found between preoperative expectations and satisfaction | n/a |
| Mancuso et al, 200941 | Yes | Patients who had a favourable response had a greater proportion of expectations fulfilled (90%) in comparison with those who did not have a favourable response (39%) | p ≤ .001 |
| Mannion et al, 200924 | No | Expectations or met expectations did not contribute to the explained variance in satisfaction | n/a |
| Noble et al, 200626 | Yes | Met expectations was, among five other variables, a significant contributor to satisfaction | OR = 6.01, p ≤ .001 |
| Palazzo et al, 201425 | Yes | Fulfilment of expectations was associated with satisfaction | OR = 1.08, p ≤ .001 |
| Scott et al, 201022 | Yes | Satisfaction correlated significantly with met expectation | r = .77 |
| Scott et al, 201232 | Yes | A significant difference was found between met expectations in terms of satisfaction in THA patients and TKA patients | p = .003 p ≤ .001 |
| Gonzalez Saenz de Tejada et al, 201454 | Yes | High and very high expectations of daily activities were associated with a higher level of satisfaction | p = .012 p ≤ .001 |
| Thambiah et al, 201528 | Yes | Preoperative expectations were significantly associated with higher satisfaction | p = .033 |
| Vissers et al, 201035 | Yes | Fulfilled expectations regarding limitations and overall success of treatment were significantly related to satisfaction (p ≤ .001) | OR = 13.6, p ≤ .001 OR = 34.0, p ≤ .001 |
Fig. 2.
Schematic representation of methodological characteristics of included studies and number of studies reporting a significant correlation between (fulfilment of) preoperative expectations and satisfaction.
Note. TKA, total knee arthroplasty; THA, total hip arthroplasty.
Fig. 3.
Harvest plot: evidence for relationship between (fulfilment of) preoperative expectations and satisfaction, stratified by study design.
Note. Columns represent studies included in this systematic review with their reference number below. The height of columns corresponds to the number of patients examined within that study. Numbers above columns indicate the quality of study according to the Newcastle-Ottawa Scale. Grey shades were used for retrospective studies, black shades for prospective studies. Fulfilment studies are dashed, as they are not classified as either retrospective or prospective. The plot is split between studies examining preoperative expectations and studies examining fulfilment of expectations.
Difference between TKA and THA patients
Of the 22 included studies, 11 (50%) studies focused on TKA patients, six (27%) on THA patients and five (23%) studies included both TKA and THA patients. Only two of these five studies reported separate data for TKA and THA patients (Fig. 2).22,34 For both TKA and THA patients a similar significant positive link between fulfilled expectations and satisfaction existed.34
Of the 14 fulfilment studies, eight (57%) reported values regarding fulfilment of expectations. Almost all hip (81%) and knee (77%) patients had all their expectations fulfilled at least six months post-surgery. On average, all expectations were fulfilled in hip patients in 79%, and in knee patients in 63%. Ninety-one per cent of the hip patients were satisfied with the outcome of surgery, while knee patients were satisfied with the outcomes of surgery in 86% of cases.
Retrospective versus prospective designs
Of the eight preoperative studies, seven studies (88%) prospectively assessed expectations before surgery. Only one study adopted a retrospective design in which patients were asked, after surgery, to recall their preoperative expectations.33 Three out of seven studies (43%) which prospectively assessed preoperative expectations reported a significant positive association between expectations and satisfaction (Table 4). The one study examining preoperative expectations after surgery (i.e. retrospectively) also reported a significant positive relationship with satisfaction.33 As such, according to the best-evidence synthesis, conflicting findings are reported as to whether preoperative expectations are related to satisfaction in a prospective design. Moreover, limited evidence existed for the relationship between preoperative expectations and satisfaction in a retrospective design.
Comparing differences in follow-up period
Most studies adopted a follow-up period of approximately one year (68%). The significance of the relationship between (fulfilment of) expectations and satisfaction varied largely between different follow-up times and did not point towards a fixed optimal follow-up period (Table 5). Therefore, limited evidence existed for the notion that fulfilment of expectations leads to satisfaction up to six months after surgery. However, strong evidence existed for up to one year after surgery, conflicting evidence for up to two years and strong evidence for up to six years.
Table 5.
Percentage of studies with a significant relationship between (fulfilled) expectations and satisfaction found across studies, stratified for follow-up period.
| Relationship | Yes (percentage) | No (percentage) | Total (22) | |
|---|---|---|---|---|
| Up to six months | 2 (100%) | 0 (0%) | 2 | |
| Fulfilment | 1 (50%) | 0 (0%) | ||
| Preoperative expectations | 1 (50%) | 0 (0%) | ||
| Up to one year | 10 (80%) | 2 (20%) | 12 | |
| Fulfilment | 9 (100%) | 0 (0%) | ||
| Preoperative expectations | 1 (25%) | 2 (75%) | ||
| Up to two years | 3 (50%) | 3 (50%) | 6 | |
| Fulfilment | 2 (67%) | 1 (33%) | ||
| Preoperative expectations | 1 (33%) | 2 (67%) | ||
| Up to six years | 2 (100%) | 0 (0%) | 2 | |
| Fulfilment | 1 (100%) | 0 (0%) | ||
| Preoperative expectations | 1 (100%) | 0 (0%) |
Discussion
This best-evidence synthesis provides an overview of the literature regarding the relationship between (fulfilment of) outcome expectations and satisfaction with outcome, and the influence of used methodology and patient group on the (existence of the) relationship. Almost all studies assessing fulfilment of expectations reported a significant positive association with either level of satisfaction or the odds of being satisfied with the results of surgery (93%). In contrast, only half of the studies reported a significant relationship between preoperative expectations and satisfaction with outcomes of surgery.
One cross-sectional study found that preoperative expectations were generally related to a high level of satisfaction when assessing expectations retrospectively. Nonetheless, they did not state whether either low or high expectations, or having expectations in general, was related to satisfaction.33 Thereby, it seems that the findings regarding the relationship between preoperative expectations and satisfaction become more conflicted when assessing the relationship prospectively. Some patients might not be able to recall their preoperative expectations after surgery as the amount of time between the actual expectation and the recall of this expectation, as well as the meaningfulness of the expectation for the patient, determines the accuracy of the recall.55 Patients may even experience some sort of recall bias or response shift. Due to this possible response shift, patients change their views about expectations to match their present status.43 In fact, it is found that about 35% of all patients recalled their preoperative function as higher or lower than the actual level of functioning.56
The expectation-confirmation theory states that disconfirmation or dissatisfaction results from a lack of balance between expectations and fulfilled expectations.57 Patients might therefore (unconsciously) change their preoperative expectations postoperatively in order to diminish imbalance between expectations and outcomes and to prevent dissatisfaction. Consequently, both high and low expectations could in essence lead to satisfaction when these expectations are fulfilled.58,59 However, it can be noted that high expectations have an advantage over low expectations. It was proposed that patients with realistic high expectations might be more motivated to obtain the desired results in rehabilitation by adhering to instructions and training,54 and might actually achieve these results through some sort of self-fulfilling prophecy60 resulting in fulfilled expectations, leading to a high level of satisfaction. Moreover, as Eisler et al stated: ‘The motivation to undergo surgery reflects its reward value and the expectation of success’.37 It is therefore of great importance to create and maintain high expectations, considering that a delay, or even refusal of surgery may result from low expectations. Nevertheless, unrealistic high expectations (i.e. high expectations which are not in accordance with actual expected outcomes) could in turn lead to dissatisfaction and lower health-related quality of life61 and, unfortunately, up to half of the patients have too optimistic expectations.24,26 Summarizing the results of this systematic review, thereby taking into account the existing evidence regarding expectations in TKA and THA patients, it should be noted that patients should have high expectations in order to achieve optimal results, yet should be guarded from unrealistic high or low expectations, as they could lead to unfulfilled expectations and consequently to dissatisfaction.
The contradictory findings from studying only the effect of preoperative expectations on satisfaction were absent when fulfilment of expectations was studied instead. Almost all studies in which the relationship between fulfilment of expectations and satisfaction was examined, found a significant relationship. Only one study told patients what expectations they had cited before and asked how they were now fulfilled.34 This study was the only study which found no relationship between fulfilment and satisfaction. Even though it was previously found that a possible response shift could not interfere with the significance of the relationship between fulfilled expectations and satisfaction,46 future research should examine the effects between recalled and actual fulfilled expectations on satisfaction.
The results in this review differ largely between follow-up times and do not point towards a fixed optimal follow-up period. As Barlow et al46 pointed out, a form of timing bias could exist, as expectations may not be fulfilled up to two years after surgery, considering that function could progress up to two years after surgery. Furthermore, no large differences were found in terms of fulfilled expectations or percentage of satisfied patients when differentiating between hip and knee patients. In other studies, THA patients generally met more expectations and were more satisfied with the outcome than TKA patients.45 It seems that these patients returned to function to a larger and faster extent than TKA patients.4,8,45 Therefore, expectations might be met at an earlier stage. Nonetheless, after six months, improvement in function returned to the same level for both patient groups.4 The return to the same level of improvement between hip and knee patients, which is found after six months, could explain why, in our review, fulfilled expectations and satisfaction rates are no different between hip and knee patients, as the majority of studies examined fulfilled expectations beyond six months post surgery. However, considering that there are differences between hip and knee patients, future research should examine whether the optimal level of expectations also differs between hip and knee patients.
This study has a number of limitations. The definition of ‘satisfaction with outcome’ might be a subject of debate since satisfaction is assessed with different instruments in the literature. Moreover, the operationalization of outcome expectations was quite diverse as well. Some studies do not report the method of assessment, while others thoroughly examined several domains of expectations (e.g. expectations regarding symptoms, pain, mobility, quality of life) and satisfaction (e.g. pain, function, hospital experience, and performing regular activities/sport). The lack of consensus on the operationalization of constructs may be a reason for contradictory findings in preoperative studies. Nonetheless, this explanation for contradictory findings seems unlikely, as there were no conflicting findings in fulfilment studies, while they also differed in operationalization of the constructs. The relationship between fulfilled expectations and satisfaction with outcome seems robust, despite differences in measurement and operationalization of the constructs. Another limitation might be the inclusion of a study with revision surgery.37 Although the main objective of that study was not to examine level of expectations, findings might be confounded due to prior experiences, which could have influenced the level of expectations. In addition, only statements regarding the significance of the relationships could be made and not regarding the strength or impact of the relationship, as we were unable to extract effect sizes.
In conclusion, fulfilment of expectations is consistently associated with satisfaction regardless of study design or patient group (i.e. hip or knee patients). Emphasis in future research should be placed on the operationalization and measurement of expectations and satisfaction to determine the (strength of the) influence of these different forms of assessment on the (existence of the) relationship between (fulfilled) expectations and satisfaction with outcome. It should be examined what the optimal level of expectations would, or could, be and how changes in (fulfilled) expectations relate to changes in satisfaction. Furthermore, research should be broadened to other patient groups as well to examine the generalizability of these results to ‘the patient’ in general.
Acknowledgments
We thank Maria Karabatzakis for her contribution in the quality assessment.
Footnotes
ICMJE Conflict of interest statement: TG reports board membership of Nederlandse Orthopaedische Vereniging, outside the submitted work.
The other authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Corti MC, Rigon C. Epidemiology of osteoarthritis: prevalence, risk factors and functional impact. Aging Clin Exp Res 2003;15:359–363. [DOI] [PubMed] [Google Scholar]
- 2. Lawrence RC, Felson DT, Helmick CG, et al. ; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 2008;58:26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol 2006;20:3–25. [DOI] [PubMed] [Google Scholar]
- 4. Hamilton D, Henderson GR, Gaston P, MacDonald D, Howie C, Simpson AHR. Comparative outcomes of total hip and knee arthroplasty: a prospective cohort study. Postgrad Med J 2012;88:627–631. [DOI] [PubMed] [Google Scholar]
- 5. Katz JN. Total joint replacement in osteoarthritis. Best Pract Res Clin Rheumatol 2006;20:145–153. [DOI] [PubMed] [Google Scholar]
- 6. Lützner J, Hübel U, Kirschner S, Günther KP, Krummenauer F. [Long-term results in total knee arthroplasty: a meta-analysis of revision rates and functional outcome]. Chirurg 2011;82:618–624. [DOI] [PubMed] [Google Scholar]
- 7. Söderman P, Malchau H, Herberts P, Zügner R, Regnér H, Garellick G. Outcome after total hip arthroplasty: Part II. Disease-specific follow-up and the Swedish National Total Hip Arthroplasty Register. Acta Orthop Scand 2001;72:113–119. [DOI] [PubMed] [Google Scholar]
- 8. Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am 2004;86:963–974. [DOI] [PubMed] [Google Scholar]
- 9. Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am 2002;84:171–177. [DOI] [PubMed] [Google Scholar]
- 10. Hamilton DF, Lane JV, Gaston P, et al. What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open 2013;3:e002525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Anakwe RE, Jenkins PJ, Moran M. Predicting dissatisfaction after total hip arthroplasty: a study of 850 patients. J Arthroplasty 2011;26:209–213. [DOI] [PubMed] [Google Scholar]
- 13. Khatib Y, Madan A, Naylor JM, Harris IA. Do psychological factors predict poor outcome in patients undergoing TKA? A systematic review. Clin Orthop Relat Res 2015;473:2630–2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Polkowski GG, II, Ruh EL, Barrack TN, Nunley RM, Barrack RL. Is pain and dissatisfaction after TKA related to early-grade preoperative osteoarthritis? Clin Orthop Relat Res 2013;471:162–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ware JE, Jr, Snyder MK, Wright WR, Davies AR. Defining and measuring patient satisfaction with medical care. Eval Program Plann 1983;6:247–263. [DOI] [PubMed] [Google Scholar]
- 16. Lochman JE. Factors related to patients’ satisfaction with their medical care. J Community Health 1983;9:91–109. [DOI] [PubMed] [Google Scholar]
- 17. Baumann C, Rat AC, Osnowycz G, et al. Do clinical presentation and pre-operative quality of life predict satisfaction with care after total hip or knee replacement? J Bone Joint Surg Br 2006;88:366–373. [DOI] [PubMed] [Google Scholar]
- 18. Mahomed N, Sledge C, Daltroy L, Fossel A, Katz J. Self-administered Patient Satisfaction Scale for joint replacement arthroplasty. J Bone Joint Surg Br 1998;80:9. [Google Scholar]
- 19. Jain D, Bendich I, Nguyen LL, et al. Do patient expectations influence patient-reported outcomes and satisfaction in total hip arthroplasty? A prospective, multicenter study. J Arthroplasty 2017;32:3322–3327. [DOI] [PubMed] [Google Scholar]
- 20. Jain D, Nguyen LL, Bendich I, et al. Higher patient expectations predict higher patient-reported outcomes, but not satisfaction, in total knee arthroplasty patients: a prospective multicenter study. J Arthroplasty 2017;32:S166–S170. [DOI] [PubMed] [Google Scholar]
- 21. Lingard EA, Sledge CB, Learmonth ID; Kinemax Outcomes Group. Patient expectations regarding total knee arthroplasty: differences among the United States, United Kingdom, and Australia. J Bone Joint Surg Am 2006;88:1201–1207. [DOI] [PubMed] [Google Scholar]
- 22. Scott CE, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 2010;92:1253–1258. [DOI] [PubMed] [Google Scholar]
- 23. Baker PN, van der Meulen JH, Lewsey J, Gregg PJ; National Joint Registry for England and Wales; Data from the National Joint Registry for England and Wales. The role of pain and function in determining patient satisfaction after total knee replacement. J Bone Joint Surg Br 2007;89:893–900. [DOI] [PubMed] [Google Scholar]
- 24. Mannion AF, Kämpfen S, Munzinger U, Kramers-de Quervain I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res Ther 2009;11:R139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Palazzo C, Jourdan C, Descamps S, et al. Determinants of satisfaction 1 year after total hip arthroplasty: the role of expectations fulfilment. BMC Musculoskelet Disord 2014;15:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 2006;452:35–43. [DOI] [PubMed] [Google Scholar]
- 27. Quintana JM, Escobar A, Aguirre U, Lafuente I, Arenaza JC. Predictors of health-related quality-of-life change after total hip arthroplasty. Clin Orthop Relat Res 2009;467:2886–2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thambiah MD, Nathan S, Seow BZ, Liang S, Lingaraj K. Patient satisfaction after total knee arthroplasty: an Asian perspective. Singapore Med J 2015;56:259–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H. The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review. Health Technol Assess 1999;3:1–96. [PubMed] [Google Scholar]
- 30. Uhlmann RF, Inui TS, Carter WB. Patient requests and expectations: definitions and clinical applications. Med Care 1984;22:681–685. [DOI] [PubMed] [Google Scholar]
- 31. Haanstra TM, van den Berg T, Ostelo RW, et al. Systematic review: do patient expectations influence treatment outcomes in total knee and total hip arthroplasty? Health Qual Life Outcomes 2012;10:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scott CEH, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br 2012;94:974–981. [DOI] [PubMed] [Google Scholar]
- 33. Mancuso CA, Salvati EA, Johanson NA, Peterson MG, Charlson ME. Patients’ expectations and satisfaction with total hip arthroplasty. J Arthroplasty 1997;12:387–396. [DOI] [PubMed] [Google Scholar]
- 34. Lim JB, Chou AC, Yeo W, et al. Comparison of patient quality of life scores and satisfaction after common orthopedic surgical interventions. Eur J Orthop Surg Traumatol 2015;25:1007–1012. [DOI] [PubMed] [Google Scholar]
- 35. Vissers MM, de Groot IB, Reijman M, Bussmann JB, Stam HJ, Verhaar JA. Functional capacity and actual daily activity do not contribute to patient satisfaction after total knee arthroplasty. BMC Musculoskelet Disord 2010;11:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Arden NK, Kiran A, Judge A, et al. What is a good patient reported outcome after total hip replacement? Osteoarthritis Cartilage 2011;19:155–162. [DOI] [PubMed] [Google Scholar]
- 37. Eisler T, Svensson O, Tengström A, Elmstedt E. Patient expectation and satisfaction in revision total hip arthroplasty. J Arthroplasty 2002;17:457–462. [DOI] [PubMed] [Google Scholar]
- 38. Kiran A, Bottomley N, Biant LC, et al. Variations in good patient reported outcomes after total knee arthroplasty. J Arthroplasty 2015;30:1364–1371. [DOI] [PubMed] [Google Scholar]
- 39. Mancuso CA, Sculco TP, Wickiewicz TL, et al. Patients’ expectations of knee surgery. J Bone Joint Surg Am 2001;83:1005–1012. [DOI] [PubMed] [Google Scholar]
- 40. Clement ND, MacDonald D, Patton JT, Burnett R. Post-operative Oxford knee score can be used to indicate whether patient expectations have been achieved after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:1578–1590. [DOI] [PubMed] [Google Scholar]
- 41. Mancuso CA, Jout J, Salvati EA, Sculco TP. Fulfillment of patients’ expectations for total hip arthroplasty. J Bone Joint Surg Am 2009;91:2073–2078. [DOI] [PubMed] [Google Scholar]
- 42. Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty 2009;24:716–721. [DOI] [PubMed] [Google Scholar]
- 43. Schwartz CE, Andresen EM, Nosek MA, Krahn GL; RRTC Expert Panel on Health Status Measurement. Response shift theory: important implications for measuring quality of life in people with disability. Arch Phys Med Rehabil 2007;88:529–536. [DOI] [PubMed] [Google Scholar]
- 44. Culliton SE, Bryant DM, Overend TJ, MacDonald SJ, Chesworth BM. The relationship between expectations and satisfaction in patients undergoing primary total knee arthroplasty. J Arthroplasty 2012;27:490–492. [DOI] [PubMed] [Google Scholar]
- 45. Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K. Comparing patient outcomes after THA and TKA: is there a difference? Clin Orthop Relat Res 2010;468:542–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Barlow T, Clark T, Dunbar M, Metcalfe A, Griffin D. The effect of expectation on satisfaction in total knee replacements: a systematic review. Springerplus 2016;5:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Waljee J, McGlinn EP, Sears ED, Chung KC. Patient expectations and patient-reported outcomes in surgery: a systematic review. Surgery 2014;155:799–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty 2017;32:3854–3860. [DOI] [PubMed] [Google Scholar]
- 49. Duivenvoorden T, Verburg H, Verhaar JA, Bierma-Zeinstra SM, Reijman M. [Patient expectations and satisfaction concerning total knee arthroplasty]. Ned Tijdschr Geneeskd 2017;160:D534. [PubMed] [Google Scholar]
- 50. Wells GA, Shea B, O’Connell D, Peterson JEA, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (date last accessed 30 December 2016).
- 51. Slavin RE. Best evidence synthesis: an intelligent alternative to meta-analysis. J Clin Epidemiol 1995;48:9–18. [DOI] [PubMed] [Google Scholar]
- 52. Lievense AM, Bierma-Zeinstra SM, Verhagen AP, Verhaar JA, Koes BW. Prognostic factors of progress of hip osteoarthritis: a systematic review. Arthritis Rheum 2002;47:556–562. [DOI] [PubMed] [Google Scholar]
- 53. Mancuso CA, Sculco TP, Salvati EA. Patients with poor preoperative functional status have high expectations of total hip arthroplasty. J Arthroplasty 2003;18:872–878. [DOI] [PubMed] [Google Scholar]
- 54. Gonzalez Saenz de Tejada M, Escobar A, Bilbao A, et al. A prospective study of the association of patient expectations with changes in health-related quality of life outcomes, following total joint replacement. BMC Musculoskelet Disord 2014;15:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol 1990;43:87–91. [DOI] [PubMed] [Google Scholar]
- 56. Razmjou H, Yee A, Ford M, Finkelstein JA. Response shift in outcome assessment in patients undergoing total knee arthroplasty. J Bone Joint Surg Am 2006;88:2590–2595. [DOI] [PubMed] [Google Scholar]
- 57. Appleton-Knapp SL, Krentler KA. Measuring student expectations and their effects on satisfaction: the importance of managing student expectations. J Mark Educ 2006;28:254–264. [Google Scholar]
- 58. Hudak PL, Hogg-Johnson S, Bombardier C, McKeever PD, Wright JG. Testing a new theory of patient satisfaction with treatment outcome. Med Care 2004;42:726–739. [DOI] [PubMed] [Google Scholar]
- 59. Younger AS, Wing KJ, Glazebrook M, et al. Patient expectation and satisfaction as measures of operative outcome in end-stage ankle arthritis: a prospective cohort study of total ankle replacement versus ankle fusion. Foot Ankle Int 2015;36:123–134. [DOI] [PubMed] [Google Scholar]
- 60. Andrykowski MA, Brady MJ, Greiner CB, et al. ‘Returning to normal’ following bone marrow transplantation: outcomes, expectations and informed consent. Bone Marrow Transplant 1995;15:573–581. [PubMed] [Google Scholar]
- 61. Merton RK. The self-fulfilling prophecy. Antioch Rev 1948;8:193–210. [Google Scholar]