With the spread of the coronavirus disease 2019 (COVID-19) pandemic, the working routine in the Emergency Department (ED) has profoundly changed. The adjustment has affected many aspects of our division: we needed structural and environmental reorganization, new roles definition, skills and equipment.
Interestingly, while we were trying to manage the great increase of COVID-19 suspect patients into the ‘dirty’ ED area, we noticed a drop of the ED access to the ‘clean’ area, for non-COVID-19 issues. Therefore, we aimed to quantify this variation by comparing the ED reasons of admission, hospitalization and discharge during a similar period of the previous year.
The ED of Santa Croce and Carle Hospital in Cuneo, Italy, has a number of potentially referring patients of about 150 000 people. The total amount of ED examinations during 2018 and 2019 (excluding gynecological and pediatric patients which are managed separately) was, respectively, 46.154 and 45.395 patients. We compared the amount of ED accesses, the percentage of hospitalizations and the discharge diagnosis in the period between 21 February 2020 (the day of the first registered Italian case of COVID-19) and 3 April 2020, and the corresponding period of 2019. We also performed a targeted subanalysis of a restricted period, following the 11 March 2020 (day of the first confirmed case of COVID-19 in our area) to 3 April 2020.
As suggested by daily observation, the total number of ED examinations in 2020 has dramatically decreased: we recorded a 50% reduction compared to 2019 in the period after February 21, and a 68% reduction limiting the analysis in the beginning of the epidemic in our area. At the same time, we observed an increase of hospitalizations from 22 to 33%, considering the entire period, and from 22 to 44% from 11 March 2020 (Fig. 1).
Fig. 1.
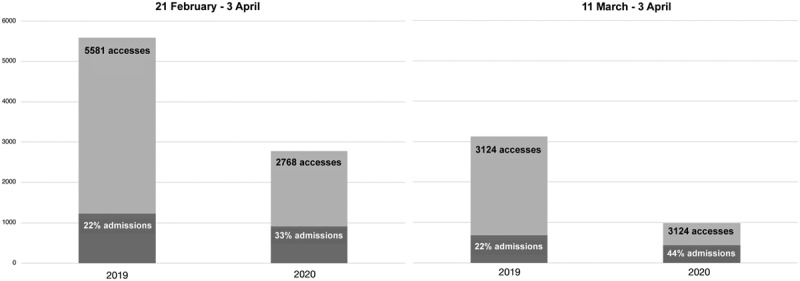
Number of emergency department access and hospital admissions in 2019 and 2020, between 21 February and 3 April and 11 March and 3 April.
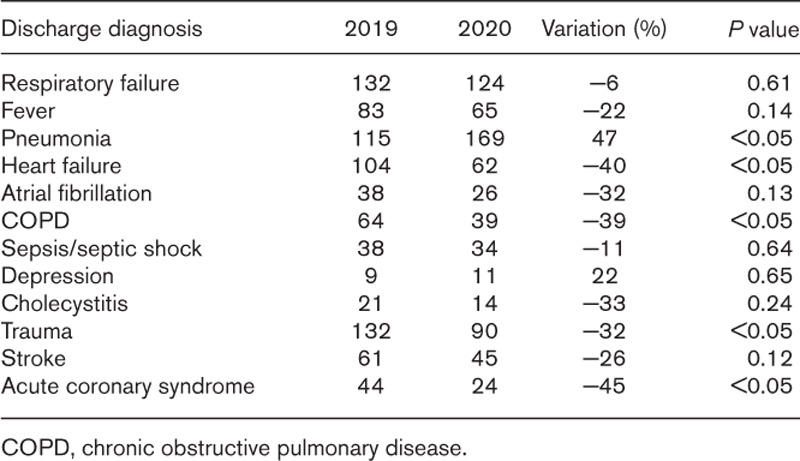
Considering the total population potentially referring to our ED, we found a significant drop in the ED access for lower back pain, general malaise, joint pain, dizziness and other nonurgent conditions in 2020 compared to 2019, among the former group of discharged patients. We also observed a significant reduction in trauma. In the group of the hospitalized patients, the expected significant increase of pneumonia was confirmed, with a substantial stability of respiratory failure, sepsis and fever, but a surprisingly reduction of life-threatening diagnoses as coronary syndrome, heart failure and stroke (Tables 1 and 2).
Table 1.
Variation of patients discharged from the emergency department in 2019 and 2020, by diagnosis
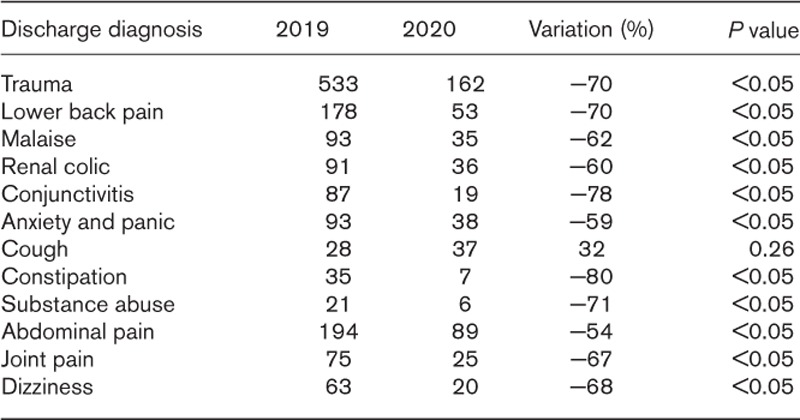
Table 2.
Variation of hospitalized patients from the emergency department in 2019 and 2020, by diagnosis
Some of these variations are easily explained. For example, the reduced access of traumatic accidents is secondary to the almost complete restriction of outdoor, work and ludic activities (and consequently of traffic) dictated by the government in these weeks.
Part of the access reduction could also be related to the increasingly cited ‘questionable use of the EDs’ in the last years; patients with chronic and nonurgent diseases that can be managed by general practitioners have probably desisted from referring to the ED, following the government indications against crowding and being afraid of getting infected.
While for nonurgent cases, the reduced use of the EDs may not have global health consequences, a delay or a lack of access of patients suffering from potentially serious and time-dependent pathologies, leads to worse prognosis and death. Why the delay in this group of patients is happening is debated. The fear of contagion probably plays a role, as well as lifestyle changes. It could be hypothesized that people are now less stressed and, for example, smoke less, because they stay at home and spend more time with their families. However, staying at home the whole day and smoking less could, in some people, lead to be more stressed instead, which adds up to the general panic caused by the pandemic. Other hypotheses would support a reduction in the EDs access for cardiovascular events parallel to a decrease in physical efforts, or to the theoretical decrease of pollution, possibly involved in the pathogenesis of the diseases. Somebody also speculates a direct biological protective role of the virus on the cardiovascular system, which has not been proven at the moment.
Whatever the reason, in this period of great attention to the COVID-19, we should not forget that the Coronavirus has not eradicated the other diseases, less than ever life-treating conditions. The present risk is that people are dying at home; the next future risk is that we could be overwhelmed, at the end of the pandemic, by patients presenting with advanced diseases and complications much more difficult to treat.
Health authorities should sensitize people with chest pain, neurological symptoms and dyspnea, regardless of the presence of fever, to refer to the EDs also in this moment. Moreover, scientific evidences and studies about behaviors of non-COVID19 patients, during the COVID-19 pandemic, should be implemented.


