Abstract
This review highlights the ultrasound findings reported from a number of studies and case reports and discusses the unifying findings from coronavirus disease (COVID-19) patients and from the avian (H7N9) and H1N1 influenza epidemics. We discuss the potential role for portable point-of-care ultrasound (PPOCUS) as a safe and effective bedside option in the initial evaluation, management, and monitoring of disease progression in patients with confirmed or suspected COVID-19 infection.
Amid the recent coronavirus disease (COVID-19) outbreak and resulting pandemic, there has been a growing necessity to determine novel ways of safely evaluating patients who are suspected to be infected with the virus. Given the limited supply, cost, and often slow turnaround time of available assays, testing every patient who presents with symptoms or with recent exposure is currently not a viable option. It has been cited that early computed tomography scanning of patients may be beneficial, because infected patients may demonstrate radiologic findings before the onset of severe clinical symptoms.1 However, the American College of Radiology recommends that computed tomography not be used to screen for or diagnose COVID-19 and that it be used sparingly in hospitalized, symptomatic patients given the risk of infection transmission posed to staff and subsequent patients.2
There is evidence that lung point-of-care ultrasound (POCUS) may be comparable to chest radiography and to computed tomography in terms of its ability to detect parenchymal and pleural pathology and to monitor response to therapies.3 Historically, ultrasound was found to be an important tool for the rapid evaluation and assessment of pulmonary status in patients during the 2013 avian influenza A (H7N9) epidemic.4,5 Similarly, lung ultrasound may aid in the identification and subsequent monitoring of suspected COVID-19 infections, perhaps even before the onset or progression of respiratory symptoms. Here, we review the ultrasound findings reported from a number of studies and case reports1,6–8 and discuss the unifying findings from COVID-19 patients and from the avian (H7N9) and H1N1 influenza epidemics. We also discuss the potential role for portable POCUS as a safe and effective bedside option in the initial evaluation, management, and monitoring of disease progression in patients with confirmed or suspected COVID-19 infection.
POCUS FINDINGS IN COVID-19: A REVIEW OF AVAILABLE STUDIES AND CASE REPORTS
Since the outbreak, multiple studies and case reports have emerged in the literature and social media evaluating the use of lung ultrasound in patients with confirmed COVID-19 infections.1,6–9 Table 1 shows the characteristics and lung ultrasound findings that have been associated with COVID-19.
Table 1.
POCUS Examinations Performed on COVID-19 Patients
| Source | Location | No. of Patients | Patient Characteristics | Ultrasound Device | Ultrasound Scanning Protocol | Lung Ultrasound Findings |
|---|---|---|---|---|---|---|
| Huang et al7 (2020) | Xi’an Chest Hospital (Shaanxi, China) | 20 | Noncritical COVID-19–confirmed patients. Average age 27–81 y, median 45 y (3 cases >65 y) with fever, radiographic features of pneumonia by computed tomography, and normal or decreased white blood cell count | SonoScape P50 | 12 Zone Method | Posterior and inferior lung field lesions Large number of B lines (“Waterfall Sign”), at times fused and fixed (“White Lung Sign”) Rough pleural lines Subpleural pulmonary consolidations Decreased blood flow Air bronchograms |
| Jin et al1 (2020) | Xiangya Hospital (Hunan, China) | 20 | COVID-19–confirmed patients (age, sex, acuity not mentioned) | Not identified | 12 Zone Method | Thickening of pleural line and irregularities B lines in various patterns Multiple patterns of consolidation including multifocal small, nontranslobar and translobar with mobile air bronchograms A lines during recovery Pleural effusions uncommon |
| Buonsenso et al9 (2020) | Agostino Gemelli University Hospital (Rome, Italy) | 1 | Noncritical COVID-19–confirmed patient, 52-y-old man presenting after 7 d of fever and flu-like symptoms, found to have perihilar infiltrates on chest radiograph and lymphopenia | Unidentified portable ultrasound | 12 Zone Method | Pleural irregularities Subpleural consolidations Areas of thick, confluent B lines as well as spared areas |
| Chen6 ( 2020) |
Hospital Universitario La Paz (Madrid, Spain) | 1 | Noncritical COVID-19–confirmed patient, 35-y-old emergency room physician who performed ultrasound scan self on days 1–9 after COVID-19 diagnosis | Butterfly iQ | Not reported | Small bilateral pleural effusions with a thickened pleural line Basal B lines Presence and spread of subpleural consolidations Normal lung ultrasound initially Ultrasound findings occur in the absence of shortness of breath/dyspnea and occur before malaise |
| Thomas et al8 (2020) | Victoria General Hospital (British Columbia, Canada) | 1 | Critical COVID-19–confirmed patient, 64-y-old health care worker presenting 10 d after symptom onset with fevers, hypoxemia (SpO2 88%), and bilateral infiltrates on chest radiograph | Not identified | Not reported | Pleural thickening Subpleural consolidations, (“skip lesions”) Multifocal B lines |
Abbreviations: COVID-19, coronavirus disease 2019; POCUS, point-of-care ultrasound; SpO2 peripheral oxygen saturation.
Huang et al7 utilized lung ultrasound to evaluate peripulmonary lesions of 20 noncritical COVID-19 patients at Xi’an Chest Hospital in China. The authors conclude that computed tomography may be inferior to lung ultrasound in detecting smaller peripulmonary lesions and effusions in COVID-19 patients. Lung ultrasound in these patients demonstrated (1) posterior and inferior lung field lesions, (2) B lines, (3) distorted pleural lines, (4) subpleural pulmonary consolidations, and (5) air bronchograms.7 While these findings may not be specific to COVID-19 compared to other viral pneumonias, identification of these patterns during a pandemic could certainly assist providers in determining individuals who are likely to be infected.
Jin et al1 performed lung ultrasound on 20 confirmed COVID-19 patients from Xiangya Hospital and Peking Union Medical College Hospital in China. Their early findings demonstrated that the use of ultrasound provided similar results to those of computed tomography and superior results to those of standard chest radiographs.1 Their findings included (1) thickening of the pleural line with irregularity, (2) B lines, (3) consolidation, (4) the appearance of A lines during recovery, and (5) the absence of pleural effusions.1 They concluded that ultrasound was an effective way to assess the severity of a patient’s pulmonary disease and to trend their disease progression and guide eventual respiratory weaning.
Dr Yale Tung Chen,6 an emergency physician from the Hospital Universitario La Paz in Spain, was recently found to be positive for COVID-19. He took it upon himself to ultrasound his own lungs and share his findings on Twitter as his disease progressed.6 His ultrasound findings were (1) small bilateral pleural effusions with a thickened pleural line, (2) basal B lines, and (3) the presence and spread of subpleural consolidations.6 Using a portable ultrasound device in concert with a social media platform has allowed Dr Chen6 to demonstrate, in near real time, the utilization of lung ultrasonography as it applies to the COVID-19 threat.
Figure.
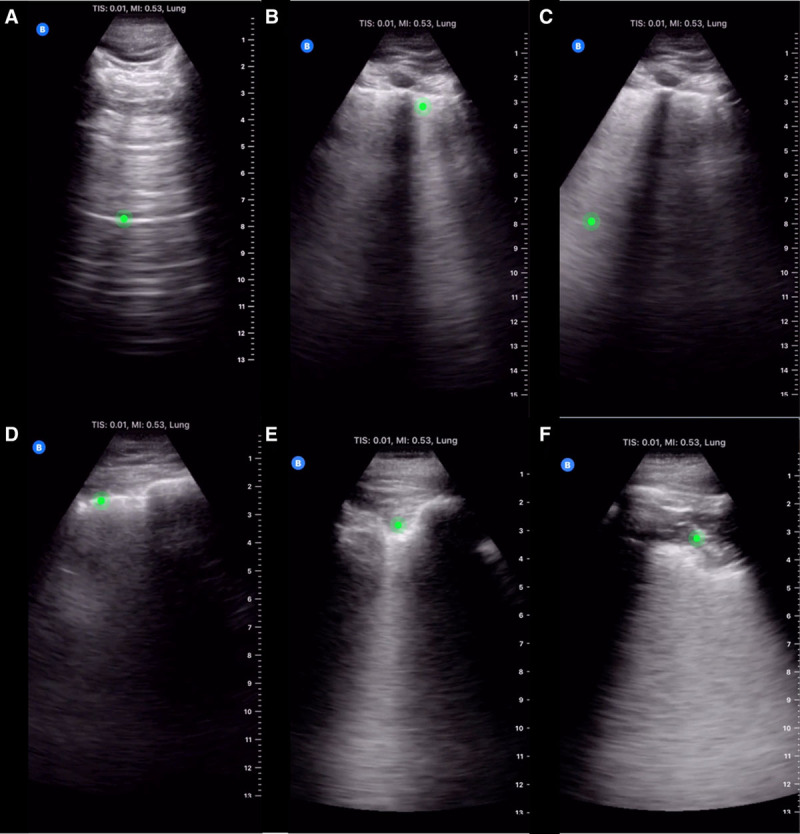
Common lung ultrasound findings in COVID-19. Lung ultrasound examination of COVID-19 patients may reveal normal lungs with A lines (A; Supplemental Digital Content 1, Video 1, http://links.lww.com/AA/D94) during the earliest stage of the infection, isolated B lines (B; Supplemental Digital Content 2, Video 2, http://links.lww.com/AA/D95; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96; Supplemental Digital Content, Video 4, http://links.lww.com/AA/D97), confluent B lines (C; Supplemental Digital Content 2, Video 2, http://links.lww.com/AA/D95), thickened and irregular pleural lines (D; Supplemental Digital Content 2, Video 2, http://links.lww.com/AA/D95; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96; Supplemental Digital Content 4, Video 4, http://links.lww.com/AA/D97), thickening and jagged pleural lines (E; Supplemental Digital Content 4, Video 4, http://links.lww.com/AA/D97), and/or subpleural consolidation with air bronchograms (F; Supplemental Digital Content 5, Video 5, http://links.lww.com/AA/D98).10 COVID-19 indicates coronavirus disease 2019.
Table 2 summarizes the ultrasound findings from the studies and case reports discussed above and includes (1) subpleural lesions in the inferior and posterior regions of the lung, which seems to be highly consistent with other cases of viral pneumonia (Figure D and F; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96 and Supplemental Digital Content 5, Video 5, http://links.lww.com/AA/D98)1,6,7; (2) individual and confluent B lines (Figure B and C; Supplemental Digital Content 2, Video 2, http://links.lww.com/AA/D95; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96; and Supplemental Digital Content 4, Video 4, http://links.lww.com/AA/D97)1,6–9; (3) signs of air bronchograms, especially peripherally (Figure F; Supplemental Digital Content 5, Video 5, http://links.lww.com/AA/D98)1,7–9; and (4) thickened or irregular pleural lines (Figure B, C, and E; Supplemental Digital Content 2, Video 2, http://links.lww.com/AA/D95; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96; and Supplemental Digital Content 4, Video 4, http://links.lww.com/AA/D97).1,6–9 Some of these findings are consistent with viral pneumonias from prior epidemics, including the subpleural consolidations described on ultrasound in influenza A (H1N1) and subpleural consolidations and B lines described in avian influenza A (H7N9).5,6,9 In contrast, normal lungs have an A-line pattern (Figure A; Supplemental Digital Content 1, Video 1, http://links.lww.com/AA/D94).
Table 2.
POCUS Examination Findings From COVID-19 Patients
| Summary of POCUS Examination Findings on COVID-19 Patients |
|---|
| Posterior and inferior lung field lesions7 Confluent and isolated B lines (Figure B and C; Supplemental Digital Content 2, Video 2, http://links.lww.com/AA/D95; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96; and Supplemental Digital Content 4, Video 4, http://links.lww.com/AA/D97)1,6–9 Thickened and/or irregular pleural lines (Figure B, C, and E; Supplemental Digital Content 2, Video 2, http://links.lww.com/AA/D95; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96; and Supplemental Digital Content 4, Video 4, http://links.lww.com/AA/D97)1,6–9 Presence of subpleural consolidations (Figure D and F; Supplemental Digital Content 3, Video 3, http://links.lww.com/AA/D96 and Supplemental Digital Content 5, Video 5, http://links.lww.com/AA/D98)1,6–9 Air bronchograms (Figure F; Supplemental Digital Content 5, Video 5, http://links.lww.com/AA/D98)1,7 |
Abbreviations: COVID-19, coronavirus disease 2019; POCUS, point-of-care ultrasound.
THE USE OF LUNG POCUS IN PRIOR EPIDEMICS: WHAT IS THE SAME?
During the 2009 influenza A (H1N1) pandemic, in which patients’ conditions rapidly deteriorated from self-limited febrile illness to an aggressive pneumonia, chest radiographs often failed to identify early interstitial lung disease.11 A cross-sectional study demonstrated abnormal ultrasound patterns showing interstitial syndrome in 15 of 16 patients who presented with normal chest radiographs, 63% of whom were subsequently diagnosed with viral (H1N1) pneumonia and 38% of whom were diagnosed with bacterial pneumonia.9 Overall, lung ultrasound was found to have 94% sensitivity and 89% specificity or a positive predictive value of 86% and a negative predictive value of 96% and outperformed chest radiography for the detection of viral pneumonia in symptomatic patients.5
The avian influenza A (H7N9) epidemics of 2013–2014 and 2016 saw large regional infection in China with a documented 1222 infections and a death rate of 40%.12 Serial lung ultrasounds of these patients demonstrated the effectiveness of POCUS in the early identification of pneumonia secondary to the H7N9 virus.4,5 In both patients who eventually developed acute respiratory distress syndrome (ARDS) as a result of the infection, serial lung ultrasound examinations showed B lines, pleural effusions, and small subpleural consolidations. These findings are consistent with previously documented findings in viral pulmonary infections such as measles and H1N1.4,5
Thus, ultrasonography has repeatedly proven to be an effective imaging modality to aid in both diagnosing and monitoring the progression of viral pneumonias. Its safety, in terms of lack of radiation exposure and relative ease of equipment sterilization to reduce the spread of infection, and accessibility to resource-limited settings make it an ideal choice during epidemics. Computed tomography, while reliable in providing good diagnostic quality imaging, is costly and carries the disadvantages of radiation exposure, lack of portability, and heightened risk of infectious spread.4,5
THE USE OF LUNG POCUS IN TODAY’S PANDEMIC: WHAT IS DIFFERENT?
Today, we have access to more affordable and portable ultrasound devices that far exceed the imaging capabilities of devices from even a decade ago. These devices may serve as an invaluable tool for the rapid diagnosis and day-to-day monitoring of suspected COVID-19 patients. In addition, today’s devices provide powerful platforms on which to share and integrate data quickly.
Traditional ultrasound has a number of limitations that portable ultrasound may be able to solve. The cost of an ultrasound machine can vary from $30,000 to upward of $150,000, prohibiting access to hospitals and care centers that are resource limited.13 Transport of these large devices to remote areas also creates added cost. These machines must be thoroughly sterilized after each use to prevent the spread of infection. Meanwhile, portable ultrasounds are available for between $2000 and $2500.14 A single handheld probe can be easily sterilized, while complete sterilization of the knobs, buttons, screens, and carts of traditional machines can be difficult and time consuming, if not impossible. Allotment of an ultrasound probe to each patient and/or the use of disposable probe covers can further help to reduce the risk of infectious spread from portable devices.14
The use of portable ultrasound for evaluating lung tissue is already common practice in many clinical settings, including emergency departments and intensive care units.13 Additional advantages include the ability to synchronize with current electronic medical records, the integration of artificial intelligence into the recognition of specific ultrasound findings, and the ability to integrate into social media, such as demonstrated by Dr Chen6 on Twitter, to promote information sharing.8,13,15 This could create a large crowdsourced index from which clinicians and scientists could continue to identify and share common findings in COVID-19 patients. Many ultrasound platforms also include video learning platforms to teach examination skills on demand, allowing for increased adoption among clinicians with limited ultrasound experience.15 Teleguidance further assists novice users by allowing them to leverage the skills of a remote expert user.15,16
RECOMMENDATIONS FOR THE USE OF LUNG ULTRASOUND IN THE COVID-19 PANDEMIC
Based on available data from prior epidemics and recent case reports, lung ultrasound may be preferred over chest radiography or computed tomography in the diagnosis and monitoring of COVID-19 patients due to its ease of bedside use, low associated cost, and reduced risk of infectious spread.1,4 Lung ultrasound can help clinicians to differentiate between a possible pneumonia and alternative causes of dyspnea while awaiting confirmatory testing or in areas where molecular assays are unavailable.
After the initial assessment, serial lung ultrasound examinations may be helpful to track the clinical trajectory of a seemingly unpredictable disease course and guide suitable treatment options and timing of interventions. For example, detection of a new consolidation with dynamic air bronchograms may suggest the development of a superimposed bacterial pneumonia. In addition to other clinical parameters, such ultrasound findings would support a decision to initiate antibiotics.15 Consolidations that are more posterior may advocate for early prone positioning in the appropriate clinical context. Similarly, increasing B lines suggests a trend toward deterioration in a patient who may benefit from titration of positive end-expiratory pressure (PEEP) to improve aeration. Atelectasis on lung ultrasound may suggest the need for additional PEEP and recruitment maneuvers. Although less common in viral pneumonia, the size, location, and appearance of any pleural effusions can be assessed by lung ultrasound to determine the need for drainage.
Serial lung ultrasounds may be particularly useful in assessing the clinical response to the above interventions and guiding the appropriateness for deescalation of care. Examinations should be performed in a standardized manner, such as by using a 12- or 14-zone method to cover all lung areas and incorporating a scoring system, as proposed by Soldati et al,16 to assist in the classification of findings. In this way, ultrasound can help predict responders and nonresponders to interventions, such as prone positioning and ventilation changes.17,18 Reduction in B lines, the reappearance of A lines, and the resolution of consolidations suggest recovery and would support a decision to wean respiratory support. Although beyond the scope of this article, it is important to note that cardiac ultrasound can also play a major role in optimizing the management of COVID-19 patients who may develop postviral cardiomyopathy19 and who may have weaning failure that is of cardiovascular origin.20
CONCLUSIONS
The COVID-19 pandemic has presented many new challenges for the medical community. As clinicians, we must embrace innovations that could make a difference in containing the disease. Lung ultrasound has the potential to improve the management of COVID-19 patients, with key advantages over other imaging modalities. The advent of affordable, portable ultrasound devices with advanced capabilities such as information sharing, video learning, and teleguidance may further increase patient and provider safety and improve patient care.
ACKNOWLEDGMENTS
We are thankful and grateful to Butterfly Network, Inc for allowing us to use their deidentified videos of COVID-19–confirmed patients in this article.
DISCLOSURES
Name: David L. Convissar, MD.
Contribution: This author helped write the manuscript.
Name: Lauren E. Gibson, MD.
Contribution: This author helped write the manuscript.
Name: Lorenzo Berra, MD.
Contribution: This author helped write the manuscript.
Name: Edward A. Bittner, MD, PhD.
Contribution: This author helped write the manuscript.
Name: Marvin G. Chang, MD, PhD.
Contribution: This author helped write the manuscript.
This manuscript was handled by: Thomas M. Hemmerling, MSc, MD, DEAA.
Supplementary Material
FOOTNOTES
GLOSSARY
- ARDS =
- acute respiratory distress syndrome
- COVID-19 =
- coronavirus disease 2019
- PEEP =
- positive end-expiratory pressure
- POCUS =
- point-of-care ultrasound
- PPOCUS =
- portable point-of-care ultrasound
- SpO2 =
- peripheral oxygen saturation
Published ahead of print 30 April 2020.
Funding: None.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website.
D. L. Convissar and L. E. Gibson contributed equally and share first authorship.
Reprints will not be available from the authors.
REFERENCES
- 1.Jin YH, Cai L, Cheng ZS, et al. for the Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team, Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM). A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radiology ACR. ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. March 22, 2020. Available at: www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed May 5, 2020.
- 3.Saraogi A.Lung ultrasound: present and future. Lung India. 2015;32:250–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsai NW, Ngai CW, Mok KL, Tsung JW.Lung ultrasound imaging in avian influenza A (H7N9) respiratory failure. Crit Ultrasound J. 2014;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu-Kun Zhang JL, Jian-ping Y, Ying Z, Jun C.Lung ultrasonography for the diagnosis of 11 patients with acute respiratory distress syndrome due to bird flu H7N9 infection. Virol J. 2015;12:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.yaletung. (2020, March 9). Day 1 #COVID diagnosis. Sore throat, headache (strong!), Dry cough but not shortness of breath. No lung US abnormalities. Will keep a #POCUS track of my lungs. #coronavirus [Tweet]. https://twitter.com/yaletung/status/1236970053515575297;yaletung. (2020, March 10). Day 2 after #COVID diagnosis. Less sore throat, cough & headache (thank God!), still no shortness of breath or pleuritic chest pain. #POCUS update: small bilateral pleural effusion, thickened pleural line & basal b-lines (plaps). #coronavirus [Tweet]. https://twitter.com/yaletung/status/1237292028221960193;yaletung. (2020, March 11). Day 3 after #COVID diagnosis. No sore throat/headache. Yesterday was cough day, still no shortness of breath/chest pain. Diarrhea started, lucky cough got better. #POCUS update: similar effusion, seems less thickened pleural line + no b-lines (PLAPS). #mycoviddiary [Tweet]. https://twitter.com/yaletung/status/1237688008444391425;yaletung. (2020, March 12). Day 4 after #COVID diagnosis. More cough & tiredness (very badly), still no dyspnea/chest pain. #POCUS update: Right side on resolution, Left side a more thickened pleural line + 2 subpleural consolidations. #mycoviddiary [Tweet]. https://twitter.com/yaletung/status/1238059289094295552;yaletung. (2020, March 13). Day 5 after #COVID diagnosis. Less cough & tired, still no dyspnea/chest pain. #POCUS update: Effusion resolved, as subpleural consolidations spread bilaterally on both posterior lower lobes. Started on HCQ yesterday. #mycoviddiary [Tweet]. https://twitter.com/yaletung/status/1238369049039515649;yaletung. (2020, March 14). Day 6 after #COVID diagnosis. Less cough, bit tired, still no dyspnea. No fever. Oxygen saturation 98%. #POCUS update: thick pleural line, b-lines and subpleural consolidations tend to resolve. Significant lung improve from yesterday. #mycoviddiary [Tweet]. https://twitter.com/yaletung/status/1238772633900068865;yaletung. (2020, March 15). Day 7 after #COVID diagnosis. Cough & weakness got worse (again), still no dyspnea. No fever. SpO2 96%. #POCUS update: similar to yesterday - thick pleural line, b-lines & consolidations tend to resolve. On paracetamol + HCQ. Stopped NSAIDs. #mycoviddiary [Tweet]. https://twitter.com/yaletung/status/1239129472802177024;yaletung. (2020, March 16). Day 8 after #COVID diagnosis. Less Cough & similar weakness, still no dyspnea or red flag symptoms. No fever. SpO2 96%. #POCUS update: Right resolved. Left lower lobe much better. Left lateral appeared new focal B-lines. On paracetamol + HCQ. #mycoviddiary [Tweet]. https://twitter.com/yaletung/status/1239482409604861952;yaletung. (2020, March 17). Day 9 after #COVID diagnosis. Feeling slightly better. More cough. No dyspnea or red flag symptoms. No fever. SpO2 97%. #POCUS update: similar to yesterday. Left lower & lateral with thick pleural line & focal B-lines. On paracetamol + HCQ. #mycoviddiary [Tweet]. https://twitter.com/yaletung/status/1239829327015022593.
- 7.Huang Y, Wang S, Liu Y.A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19). SSRN. 2020. February 26 [Epub ahead of print]. [Google Scholar]
- 8.Thomas A, Haljan G, Mitra A.Lung ultrasound findings in a 64-year-old woman with COVID-19. CMAJ. 2020;192:E399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buonsenso D, Piano A, Raffaelli F, Bonadia N, de Gaetano Donati K, Franceschi F.Point-of-Care lung ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:2776–2780. [DOI] [PubMed] [Google Scholar]
- 10.COVID-19 gallery. Butterfly Network Inc; Available at: www.butterflynetwork.com/covid19/covid-19-ultrasound-gallery. Accessed March 15, 2020. [Google Scholar]
- 11.Agarwal PP, Cinti S, Kazerooni EA.Chest radiographic and CT findings in novel swine-origin influenza A (H1N1) virus (S-OIV) infection. AJR Am J Roentgenol. 2009;193:1488–1493. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Human infection with avian influenza A (H7N9) virus – China. 2017. Available at: www.who.int/csr/don/26-october-2017-ah7n9-china/en/. Accessed May 5, 2020.
- 13.Patrick Lindsay M, Lauren G, Bittner EA, Chang MG.Portable point of care ultrasound (PPOCUS): an emerging technology for improving patient safety. Anesthesia Patient Safety Foundation. 2020;35:15–17. [Google Scholar]
- 14.Cheung JC, Lam KN.POCUS in COVID-19: pearls and pitfalls. Lancet Respir Med. 2020;8:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsung JW, Kessler DO, Shah VP.Prospective application of clinician-performed lung ultrasonography during the 2009 H1N1 influenza A pandemic: distinguishing viral from bacterial pneumonia. Crit Ultrasound J. 2012;4:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soldati G, Smargiassi A, Inchingolo R, et al. Proposal for international standardization of the use of lung ultrasound for patients with COVID-19: a simple, quantitative, reproducible method. J Ultrasound Med. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prat G, Guinard S, Bizien N, et al. Can lung ultrasonography predict prone positioning response in acute respiratory distress syndrome patients? J Crit Care. 2016;32:36–41. [DOI] [PubMed] [Google Scholar]
- 18.Wang XT, Ding X, Zhang HM, Chen H, Su LX, Liu DWChinese Critical Ultrasound Study Group (CCUSG). Lung ultrasound can be used to predict the potential of prone positioning and assess prognosis in patients with acute respiratory distress syndrome. Crit Care. 2016;20:385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Routsi C, Stanopoulos I, Kokkoris S, Sideris A, Zakynthinos S.Weaning failure of cardiovascular origin: how to suspect, detect and treat-a review of the literature. Ann Intensive Care. 2019;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


