Abstract
The aim of this study were to determine which antipsychotic are currently in use, to establish which doses are administrated to patients, to find out is there a practice of proscribing simultaneously more then one antipsy-chotic drug, to determine whether antipsychotic are proscribed in divided doses, to establish whether there is, besides antipsychotics, treatment with other medicaments (co-adminsitration), especially with antiparkinsonics. The research (study) is epidemiological-clinical prospective, descriptive and analytical and it was conducted at University hospitals in Sarajevo, Tuzla and Mostar. Criteria for inclusion, non-inclusion and exclusion from the study were precisely defined as a mean for formation of sample. Based on this hypothesis were established, zero and alterative. According to zero hypothesis in the treatment of schizophrenia at University hospitals in F/BiH new antipsychotic drugs are in use, small doses are proscribed (up to 20 mg), not more then one antipsychotic drug is used simultaneously, antipsychotics are administrated once a day and alongside with antipsychotics other medicaments are not co-administrated, especially antiparkinsons. The results of our study are showing that majority of patients are treated with classical antipsychotics. Minority of patients is treated with atypical neurolep-tics like olanzapine, which is proscribed only in Sarajevo. Use of risperidone and ziprasidone is registrated also only in Sarajevo, but only small number of patients is treated with these drugs. Most frequent antipsychotics were promazine and haloperidol. The range between minimal and maximal daily dose of promazine was from 50 to 450 mg/daily, and for haloperidol from 1 to 75 mg/daily. Above-mentioned drugs were administrated in an average from two to three times a day. Alongside with antipsychotics, other drugs were used. Most frequent was the use of biperidine in oral and parenteral formulation, as well as nitrazepam and diazepam. The importance of this study is following: data are useful for the current mental health care reform in F/B&H, results will point out place and position of F/B&H in contemporary world trends in the treatment of schizophrenia, they will contribute to rational use of antipsychotic therapy, they will point out possible ways in reduction of side effects, often dangerous adverse effects of antipsychotics, and they will give contribution to faster rehabilitation of schizophrenics with the reduction of financial means for the treatment of patients with schizophrenia.
Keywords: antipsychotics, treatment of schizophrenia
INTRODUCTION
Classic (typical) antipsychotics have two important lacks: poor effect in the treatment of negative schizophrenia symptoms and tendency to cause extrapyrami-dal side effects. It is considered that 20-30% of schizophrenic patients did not react (nonrespondents) on the treatment with typical antipsychotic medications. A need to discover new medications that will be more efficient than the existing ones, as well as growing demands of the health services for application of the psy-choactive medications, implied ongoing interest for faster development of pharmaceutical industry. Nevertheless, beside the great enthusiasm and proven benefit to the patients by new medications, provision of more comfortable and more bearable work to the staff at the psychiatric institutions, and contribution to the better economic situation in the society, the interest for identification of direct side effects and potential risk of their application is rising, beside the fact that the side effects of the psychopharmacological treatment are much smaller compared to other biological methods of therapy in psychiatry (electroconvulsive, insulin therapy and others). Atypical antipsychotics are mostly medications which have similar structure as already known antipsychotics (close to haloperidol and sulpiride), but others which have different chemical structure and mechanism of action are discovered (serotonin and dopamine antagonists) (1). Application of atypical antipsychotics is more common in the world than in our country (except clozap-ine), due to their high cost and because the current health insurance system cannot provide to the patients in our country affordable everyday use. However, we have to hope that soon these new antipsychotics will be available also to the professionals in our country.
PATIENTS AND METHODOLOGY
SELECTION OF PATIENTS
All patients with schizophrenia situated in the university hospitals in FB&H (Sarajevo, Tuzla, Mostar) included trough census in this study.
RESEARCH TYPE
This research is epidemiological, clinical, prospective, descriptive and analytical. Inclusion criteria’s:
diagnosed schizophrenia by neuropsychiatrist,
on antipsychotics treatment,
both genders, all ages,
patients without somatic disorders.
Exclusion criteria’s:
patients with schizophrenia and co morbidity (somatic),
pregnancy,
lactation
Criteria’s for non inclusion
patients which does not have diagnosed schizophrenia,
patients which does not take antipsychotic therapy.
RESEARCH AREA
The research is performed at the Psychiatric clinics of Universities in Sarajevo, Tuzla and Mostar. Census -a review of the patients is done simultaneously in all centers. The data was evaluated by following statistical methods. Mean values are computed for the results of each individual test. In addition, analyses of variance, significance of differences between the mean values and test of correlation significance between the tests used in the study were also performed. Obtained results are presented in form of text comments, table and charts.
RESULTS
Sample is consisted of 216 patients. From this number eighty five (85) patients are from Sarajevo, forty-four (44) from Mostar and eighty seven (87) from Tuzla. According to age structure, distribution of the patient is generally equal. The least number of patients is in the age group younger than twenty years 0,46%, and older than sixty 5,56% as in the whole sample, as well as in each center. Majority of patients is in the age group from forty to forty nine years of age 31,02% in Sarajevo and Mostar, and in Tuzla the most dominant age group from fifty up to fifty nine years 32,18% (Table 1 and Chart 1). Within the total sample most dominant is male patients, in total 131 patient or 60,65%, compared to 39,35% of women. Similar ratio is present in individual centers, where Sarajevo and Tuzla have similar distribution of male patients with 57,65 %, and 58,62%, and similar ratio of women 42,35% in Sarajevo, and 41,38 % in Tuzla. In Mostar also more dominant are male patients, with 70,45% of Mostar sample compared to 29,55% of women (Table 2 and Chart 2). Within the total sample 61,57% of patients have diagnosed schizophrenia, while 38,43% patients do not have confirmed diagnosis. In Mostar and Sarajevo there is 100% and 77,65% of patients with confirmed schizophrenia, while the least number of patients with schizophrenia diagnosis is in Tuzla 26,44 % (Table 3).
TABLE 1.
Patient’s age

CHART 1.

Patients age -by centers
TABLE 2.
Gender

CHART 2.

Gender
TABLE 3.
Patients with diagnosed schizophrenia

ANTYPSYCHOTIC TREATMENT AT THE UNIVERSITY HOSPITALS
Majority of patients received classic antipsychotic medications. In Sarajevo most frequently administered was promazine, orally and parenteral, for total of 38 patients or 28,6% of Sarajevo sample. In Tuzla most frequently administered antipsychotics was haloperidol and thioridazine for 20 and 21 patients, which are 19, 2%, and 20, 2% of total number of patients in Tuzla. In Mostar the leading antipsychotic is haloperidol, orally administered, and with which 29 patients were treated. This represent 31,2% of total number of patients in Mostar (Table 4). Fewer patients were treated with atypical narcoleptics such as olanzapine, which was applied in treatment only in Sarajevo for 15 patients or 11,3%. Clozapine was applied in all three centers but in very small percentage of cases (Table 4 and Chart 3). Among other medications in Sarajevo most frequently administered is nitrazepam in 20 cases (33,9%), as well as in Tuzla in 27 cases (26,5%). In Mostar most frequent medication is biperidine in oral and parenteral form in 32 cases which is more than half of treated patients, or ten cases (16,9%) (Table 5 and Chart 4). In Sarajevo 44 patients (51,8%) was treated with only one antipsychotic, 36 (42,4%) with two, while the combination of three or more antipsychotics received only five patients (5,9%). In Tuzla 70 patients (80,5%) received only one antipsychotic medication, 17 (19,5%) with two, while combination of three or more antipsychotics wasn’t use in the treatment. In Mostar seven patients (16,3%) was treated with only one antipsychotic, the majority of patients was treated with two 23 (53,5%), and the combination of three or more antipsychotic was used for 13 patients (30,2%). We can notice within the total sample that the majority of patients was treated with only one antipsychotic 121 (56,3%), and 76 (35,3%) patients was treated with two antipsychotics. Few patients were treated with three or more antipsychotics, 18 of them or 8,4% (Table 6). In Sarajevo 38 patients (44,7%) did not receive treatment with other medications, and with only one from the group of others 37 (43,5%) patients were treated. Application of two medications from the group of others is registered among 10 patients (11,8%). Eighteen patients in Tuzla (20,7%) were not treated with other medications, and with only one medication from the groups of others forty patients (50,6%) were treated. Application of two medications from the group of others is registered in 17 cases (19,5%). Combination of three other medications was applied in 8 cases (9,2%). Four patients in Mostar (9,1%) did not receive any other medication, and 26 (59,1%) were treated with only one from the group of others. Application of two other medications is registered in 10 cases (22,7%). Combination of three other medications is present in three cases (6,8%), while only one patient (2,3%) received four medications from the group of others. It is evident that in the whole sample (baseline) majority of patients were treated with only one medication from the group of others 107 (49,5%), after that most dominant are the patients that did not receive neither one other medication, sixty of them or 27,8% (Table 7). Within the total sample the most frequently applied classical antipsychotics were haloperidol, promazine, and from the group of new antipsychotics clozapine. Most frequently used other medication biperidine and diazepam. Administration of all medication is followed trough application of individual doses, daily doses and frequency of applications.
TABLE 4.
Application of typical and atypical antipsychotics (Overview by cities)

CHART 3.

Most frequently administered antipsychotics
TABLE 5.
Application of other medications (antiparkinsonics, anxiolitics, antidepressants) (overview by cities)

CHART 4.

Most frequent other medications
TABLE 6.
Number of applied antipsychotic medications

TABLE 7.
Number of administered other medications

INDIVIDUAL DOSES OF HALOPERIDOL (ORAL FORM)
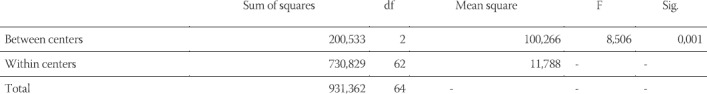
Within the total sample 65 (30,1%) patients were treated with haloperidol in oral form. In Sarajevo 16 patients were treated with haloperidol, in Tuzla 20, and in Mostar 29 patients, which is 30,1% of baseline (Table 8). Significant statistical difference between the centers regarding the administration of individual halo-peridol doses were noticed at the level 0,001 (Table 9).
TABLE 8.
Haloperidol -individual dose

TABLE 9.
Haloperidol -individual dose (ANOVA)
APPLICATION OF HALOPERIDOL BY DAILY DOSES
The highest average daily dose of haloperidol were administered in Mostar 18,13 mg, while similar daily doses are applied in Sarajevo and Tuzla 6,37 mg and 8,15 mg. (Table 10). There is a significant statistical difference between the centers by application by halo-peridol daily doses applied at the 0,001 level (Table 11).
TABLE 10.
Haloperidol -daily doses

TABLE 11.
Haloperidol -daily doses (ANOVA)

FREQUENCY OF HALOPERIDOL ADMINISTRATION
Frequency of haloperidol application is similar as well among the centers as well in the total sample (Table 12). Analyses of variance showed that there is not a statistically significant difference between the groups (cities) regarding the frequency of halo-peridol administration in the oral form (Table 13).
TABLE 12.
Frequency of haloperidol application

TABLE 13.
Frequency of haloperidol application (ANOVA)

CLOZAPINE APPLIED IN INDIVIDUAL DOSE
Three patients in Sarajevo were treated with clozapine, in Tuzla eleven, and in Mostar four patients. Total number of patients treated with clozapine is eighteen (8,3%) within baseline (Table 14). A significant statistical difference was not noticed between the tested centers regarding the applied individual clozapine doses (Table 15).
TABLE 14.
Clozapine -individual doses

TABLE 15.
Clozapine -individual dose (ANOVA)

DAILY DOSES OF CLOZAPINE APPLICATION
Average daily dose of clozapine was 229,16 mg, while the lowest daily dose is applied in Mostar 168,75 mg, and highest in Sarajevo 266,66 mg. Within the total sample, minimal daily dose of clozapine is 75 mg, and maximal daily dose is 450 mg (Table 16). A significant statistical difference was not noticed between the tested centers regarding the applied daily clozapine doses (Table 17).
TABLE 16.
Clozapine -daily doses

TABLE 17.
Clozapine-daily dose (ANOVA)

FREQUENCY OF CLOZAPINE USE
In all centers clozapine was administered three times per day, so there is not a statistically significant difference between the centers regarding the frequency of clozapine administration (Tables 18 and 19).
TABLE 18.
Frequency of clozapine administration

TABLE 19.
Frequency of clozapine administration (ANOVA)

OTHER MEDICATION -ORAL FORM
Biperidine
Biperidine applied in individual doses
In Sarajevo a total of 8 patients were treated with bi-peridine, in Tuzla 9, and in Mostar 32 patients. Total number of treated with biperidine is 49 (22,7%) within baseline (Table 20). Significant differences were not found between the centers in the relation to administered individual doses of biperidine (Table 21).
TABLE 20.
Biperidine -individual doses

TABLE 21.
Biperidine individual dose (ANOVA)

Biperidine administered in daily doses
Average daily dose of biperidine was 3,61 mg, while the lowest daily dose is applied in Mostar 2,22 mg168,75 mg, and highest in Sarajevo 5,87 mg (Table 22). Significant differences between the centers were not notices regarding the administered daily doses of biperidine (Table 23).
TABLE 22.
Biperidine -daily doses

TABLE 23.
Biperidine -daily doses (ANOVA)

FREQUENCY OF BIPERIDINE APPLICATION
Average frequency of biperidine administration varies in the total sample as well as between the centers (Table 24). There are statistically significant differences regarding the frequency of biperidine use between the centers (p=0,008) (Table 25).
TABLE 24.
Frequency of biperidine application

TABLE 25.
Frequency of biperidine application (ANOVA)

DISCUSSION
Conducted a comparative research regarding the applied antipsychotics in the period from 1989. until 1993. During the 1993 antipsychotics were prescribed to 299 patients (42%) from a total of 709 hospitalized patients. The treatment begins usually within the first 24 hours, while the hospitalization lasted around eighteen days. Highly potent antipsychotics were used 2,4 times more frequently than the low potent; 13% of patients were treated with clozapine. Average daily doses of the applied antipsychotics equivalent to daily doses of chlorproma-zine was 305 mg; and the maximal doses was 32% higher. Doses of highly potent antipsychotics (fluphenazine and haloperidol) are only 22%-33% above the mean values (2). Very rarely two or more antipsychotics were used, but it is noticed that there was a co administration of an-ticonvulsants (in 84% of cases, among which 92% was treated with valproate), benzodiazepines (81%), lithium (70%), one antidepressant (84%) or more (45%). The doses were in average higher by 20% among males, 42% lower for the patients older than 50 years compared to the patients aged 20-30, and 53% higher for the patients with schizophrenia or schizoaffective disorders compared to other diagnoses. A comparison with 1989. indicates that the average duration of hospitalization (N=50) seventy-three days which can indicate some differences in application of neuro-leptics and benzodiazepines, while there was present lower frequency of anticonvulsants and lithium use. Authors concluded that the highly potent antipsy-chotics and clozapine are the mostly used during the 1993, also that the doses of the highly potent are just slightly lower than the doses of low potent antipsy-chotics, and that the combination with the mood stabilizers also more frequent during 1993, wile the duration of hospitalization is 25% longer during the 1989. However, our research showed that in the minority of cases atypical antipsychotics, such as clozapine, were used. In Sarajevo three patients were treated with clozapine, in Tuzla eleven, and in Mostar four patients. Total number of treated with clozapine within the total sample was eighteen (8,3%). Average individual dose that was administered to these patients within the total sample was 68,61 mg, while the lowest individual dose was administered in Mostar 56,25 mg, and highest in Sarajevo 83,33 mg, with standard deviation of 31,45 and standard error of mean of 15,72, or 28,86 and 16,66 regarding city. The confidence interval varied from 6,19 to 106,30 or from 11,62 to 155,04 for the patients from Mostar and Sarajevo. Two long-term controlled comparison studies of clozapine use with the conventional antipsychotic medications discovered the advantages of clozapine, reflected in better psychological, social and functional results. Although this effect was not extreme, it was a long lasting and confirmed the profitability of its use (3). The doses in the United States are approximately double as the doses in the Europe (200-300 mg/day). Some of the side effects of clozapine use, such as: convulsions, confusion and sexual dysfunction, are related to dose and blood levels. However, increase of body mass was not dependant on dose. Latest reports about the optimal blood levels shows that the levels should be between 200 and 250 μg/ml, although many patients had a good response even on lower concentrations (4). Contemporary researches provided a strong evidences about the efficiency of second generation antipsychotics in the treatment of schizophrenia, and clearly indicated that cause much less extrapyramidal side effects (EPS) than the traditional medications (5). In addition, there are evidences that these medications have less potency to cause tardive dyskinesia (TD) than the first generation antipsychotics, and can be useful in the treatment of preexisting TD. In general, patients tolerate much better these medications than older antipsychotics, with few important exceptions, including the risk of agranu-locytosis in clozapine use and potential to increase body mass by many medications from this group. Due to their superior safety in terms of neurological side effects, it is consider that the second-generation antipsy-chotics should be available as the first choice of treatment in schizophrenia, and preferred in first episode patients (6). Conducted a study in the public hospitals in Hong Kong with obtained data about the treatment with antipsychotic medications in relation to the dose of antipsychotics, combined use of multiple antipsy-chotics, administration in divided daily doses and co administration of antipsychotics with the medication for Parkinson’s disease. Sample was consisted of 957 schizophrenic patients randomly selected. A census was made, and the questionnaire was consisted of items about demographic and clinical data, as well as description of all medications that patients received on the day of census. Results of study indicates that the average dose of anti-psychotics was 854 +/-759 (mean 600; rang 0-4450) mg CPZeq. More than two thirds of patients received multiple medications simultaneously, while less than 20% take their medication in divided daily doses. Antipar-kinsonics was used in 69,6% of patients. Authors opinion is that the treatment with antipsychotics in mainly in accordance with international standards. Problem area is simultaneous use of multiple antipsychotics both in acute and chronic cases, than use of higher doses than recommended, as well as frequent use of antiparkinsonics in chronic cases. Because of disseminated results, authors consider that the continuous medical education will lead to improvement of treatment quality for the patients with schizophrenia (7). Compared use of anti-psychotics among hospitalized patients during the three months of 1998 (n=349), 1993. (n=299) and 1989. (n=50). Results showed that during the 1998. Atypical antipsy-chotic was mostly used e.g. olanzapine was used more than risperidone and quetiapine while all three medications were prescribed more frequently than any other antipsychotic. Two or more antipsychotics were simultaneously applied during the hospitalization for 150 patients (43%) during 1998. Total dose (dose equivalent to chlorpromazine) administered during 1998 was 371 mg/ day, 29% higher than doses for the patients during 1993, and 46% higher than doses used in 1989. Higher doses of antipsychotics were applied for the patient s with psychotic disorders compared to the patients with the affective disorders. Higher doses also lead to significant improvement of clinical state, multiple pharmacological therapy, and was applied among younger patients. Authors concluded that there is a trend of higher total anti-psychotics doses and use of multiple medications, which requires a critical assessment of cost-benefit ratio (8). In Sarajevo 44 patients (51,8%) received treatment with only one antipsychotic medication, 36 (42,4%) with two antipsychotics, while the combination of three or more antipsychotics received only five patients (5,9%). In Tuzla 70 patients (80,5%) was treated with only one antipsychotic medication, and 17 (19,5%) with two, the combination with three or more medications was not applied in treatment. In Mostar 7 patients (16,3%) was treated with only one antipsychotic medication, and the majority of patients was treated with two antipsychot-ics, in total 23 (53,5%), while the combination of three or more antipsychotics received 13 patients (30,2%).
This research achieved goals that were set:
It is determined which antipsychotics are currently used.
Ranges of the individual and daily doses were determined.
Simultaneous administration of multiple antipsychotics is determined.
It is determined that the antipsychotics are administered in divided daily doses.
The existence of treatment with other medications beside antipsychotics is determined, especially antiparkinsonics.
CONCLUSION
New antipsychotic medications prove to be more efficient in the treatment of schizophrenia and cause much less extrapyramidal side effects (EPS) than the traditional medications. In addition, these medications have less potency to cause tardive dyskinesia (TD) than the first generation antipsychotics. In general, patients react much better these medications than older antipsychotics, with few important exceptions, including the risk of agranu-locytosis in clozapine use and potential to increase body mass by many medications from this group. Due to their superior safety in terms of neurological side effects, it is considered that the second-generation antipsychotics should be available as the first choice of treatment in schizophrenia, and prefered in first episode patients. This research is epidemiological, clinical, prospective, descriptive and analytical. The research is performed at the Psychiatric clinics of Universities in Sarajevo, Tuzla and Mostar. Criteria’s for inclusion, exclusion, and non-inclusion was precisely defined as the way of sampling. In relation to this a zero and alternative hypothesis was established. Majority of patients received classic antipsychotic medications. In Sarajevo most frequently administered was promazine, orally and parenteral, for total of 38 patients or 28,6% of Sarajevo sample. In Tuzla most frequently administered antipsychotics was haloperidol and thioridazine for 20 and 21 patients, which are 19, 2%, and 20, 2% of total number of patients in Tuzla. In Mostar the leading antipsychotic is haloperidol, orally administered, and with which 29 patients were treated. This represent 31,2% of total number of patients in Mostar. Fewer patients were treated with atypical neuroleptics such as olanzapine, which was applied in treatment only in Sarajevo for 15 patients or 11,3%. Clozapine was applied in all three centers but in very small percentage of cases. According to experts opinion, it is considered that the new antipsychotics (risperidone) represents the medication of choice for the first episode, as well as for the patients with relapses, with the other new atypical antipsychotics from the group of firs and second choice, dependably on clinical state of the patient. Clozapine and paren-teral long-acting atypical antipsychotics (if manufactured), represents second choice for the patients in relapse. By expert’s opinion, selection of dose is relative, in accordance with the manufacturer recommendations, although the experts advise that in same cases olanzapine and quetiapine can be applied in higher doses than recommended by manufacturer, especially in acute cases. Special importance has a clinical effect in the maintenance and dose adaptation treatment. In some cases the experts recommends lower antipsychotics doses in the treatment of maintenance for the acute states, although in some other cases they does not consider that lowering the dose is a necessity. Experts attitudes are similar that the maintenance treatment should be performed with the lower doses of classical antipsychotics, dose to possible risk of tardive dyskinesia, while the fear of tardive dyskinesia occurrence in application of new generation of antipsychotics minimal, and because of that there is less need to reduce a dose. Importance of this research reflects in following: the data are useful within the ongoing reform of mental health system in FB&H, results point out to the position of FB&H in the contemporary world trends in schizophrenia treatment, contribution to the rational use of antipsychotic therapy, imply the was to reduce frequency of side effects, which can frequently be dangerous, and contributes to the faster rehabilitation of schizophrenic patients with the reduction of financial costs of treatment.
REFERENCES
- 1.Loga S. Loga S, editor. Treatment psychiatric disorders, in Clinical psychiatry. Faculty of Medicine Sarajevo and Tuzla. :299–314. [Google Scholar]
- 2.Loga S. Loga S, editor. Treatment psychiatric disorders, in Clinical psychiatry. Faculty of Medicine Sarajevo and Tuzla. :299–314. [Google Scholar]
- 3.Baldessarini R. J, Kando J.C, Centorrino F. Hospitaluse of an-tipsychotic agents in 1989 and 1993 stable dosing with decreased length of stay. Am J Psychiatry. 1995;152(7):1038–1044. doi: 10.1176/ajp.152.7.1038. [DOI] [PubMed] [Google Scholar]
- 4.Rosenheck R, Cramer J, Allan E, et al. Cost effectiveness of clozap-ine in patients with high and low levels of hospital use. Arch. of Gen. Psychiatry. 1999;56:565–572. doi: 10.1001/archpsyc.56.6.565. [DOI] [PubMed] [Google Scholar]
- 5.Van der Zwaag C, McvGee M, McEvoy J.P, Freuden-Reich O, Wilson W. H, Copper T.B. Response of patients with treatment-refractory schizophrenia to clozapine within three serum ranges. Am J Psychiatry. 1996;153:1579–1584. doi: 10.1176/ajp.153.12.1579. [DOI] [PubMed] [Google Scholar]
- 6.Fleischhacker WW. In: Drug treatment of schizophrenia. Schizophrenia Maj M, Sartorius N, editors. Chichester: John Wiley &Sons Ltd; 1999. [Google Scholar]
- 7.Lieberman J.A. Maximizing clozapine therapy Managing side effects. J. Clin. Psychiatry. 1998;59(Suppl 3):38–43. [PubMed] [Google Scholar]
- 8.Yip K.C, Ungvari G.S, Cheung H.K, Ng F.S, Lau S.T. Survey of an-tipsychotic treatment for schizophrenia in Hong Kong. Chin Med J (Engl) 1997;110(10):792–796. [PubMed] [Google Scholar]
- 9.Centorrino F, Eakin M, Bahk WM, Kelleher JP, Goren J, Salvatore P, Egli S, Baldessarini R. J. Inpatientantipsychotic drug use in 1998, 1993, and 1989. Am J Psychiatry. 2002;159(11):1932–1935. doi: 10.1176/appi.ajp.159.11.1932. [DOI] [PubMed] [Google Scholar]


