Abstract
A 69-year-old woman underwent routine screening with CT scan of the chest, which showed a new right upper lobe lesion. Interval increase in size of the right upper lobe nodule over 3 months, prompted a CT-guided biopsy of the lung that confirmed a diagnosis of malignant pulmonary spindle cell carcinoma (PSCC) with 90% programmed death ligand 1 expression. Positron emission tomography CT demonstrated localised stage IIA disease. Given histologically proven PSCC and the rapid growth of her tumour, curative radiation with stereotactic body radiation therapy (SBRT) to the right upper lobe primary tumour was planned as patient was deemed not to be a surgical candidate. Repeat imaging with a CT chest 2 months after SBRT demonstrated good local control of the primary disease in the right upper lobe despite rapidly advancing distant metastasis. The patient continues systemic therapy with pembrolizumab, to which she has shown good response.
Keywords: lung cancer (oncology), radiotherapy, pathology
Background
Spindle cell carcinoma (SpCC) is a rare highly malignant histological subtype of sarcomatoid carcinoma that consists purely of spindle cells derived from epithelium and comprises of only 0.4% of all lung malignancies.1
The 2015 WHO Classification of Lung Tumors categorised SpCC, International Classification of Diseases for Oncology code 8032/3, as a subtype of sarcomatoid carcinoma, in conjunction with pleomorphic carcinoma, giant cell carcinoma, carcinosarcoma and pulmonary blastoma.2 SpCC can occur in multiple organs including the oral cavity, larynx, prostate, kidneys and much less often, in the lungs.3 Pulmonary spindle cell carcinoma (PSCC) is under reported in clinical literature, with only limited data available on clinical presentation, treatment options and natural history of the disease.
Here we report a case of PSCC in a 69-year-old woman treated with stereotactic body radiation therapy (SBRT) as first-line therapy.
Case presentation
A 69-year-old woman with a medical history of chronic obstructive pulmonary disease (COPD) presented to our oncology centre following the discovery of a new right upper lobe lesion on routine screening CT scan of the chest 4 months prior. The patient’s symptoms were limited to chronic cough, shortness of breath and decreased appetite. She was a past smoker with a 42-year pack smoking history. Physical examination was unremarkable and performance status was determined to be 2 on the Zubrod Scale.
Investigations
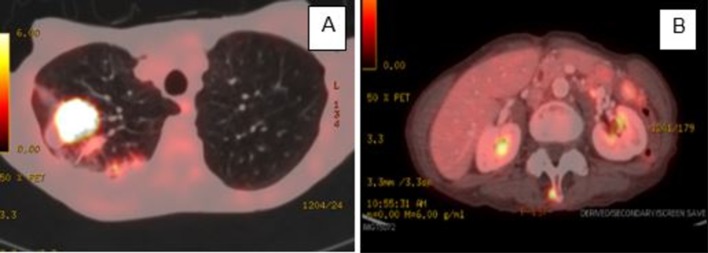
Positron emission tomography (PET)/CT completed just prior to presentation showed a 0.8 cm right upper lobe nodule that was stable/ borderline improved compared with her last CT with only mild fluorodeoxyglucose (FDG) uptake. Biopsy was offered but the patient initially deferred biopsy and opted for close follow-up with surveillance imaging. At 3 months follow-up, a repeat CT showed an interval increase in size of the right upper lobe (RUL) nodule to 2.4×1.8 cm (figure 1).
Figure 1.

CT scan of chest. A 2.4×1.8 cm circular nodule in the right upper lung field (marked with measurement).
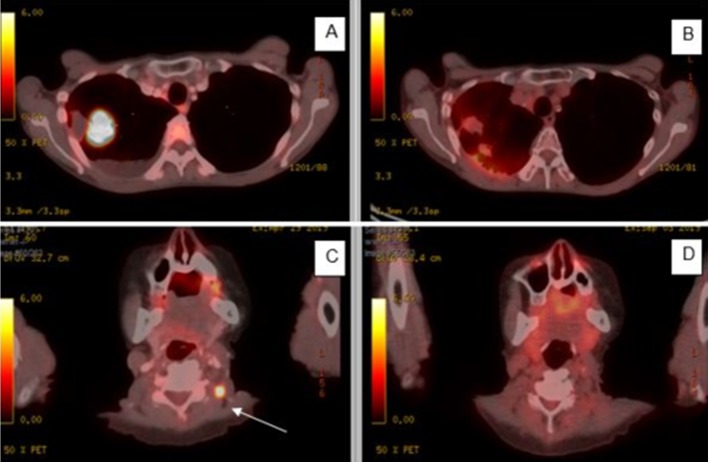
At this time, the patient agreed to a biopsy of the right upper lobe nodule. CT-guided biopsy of the lung was unfortunately complicated by a right sided pneumothorax, pneumonia and COPD exacerbation. The histology of the biopsy specimen confirmed a diagnosis of malignant PSCC with a 90% programmed death ligand 1 (PD-L1) expression (figure 2).
Figure 2.
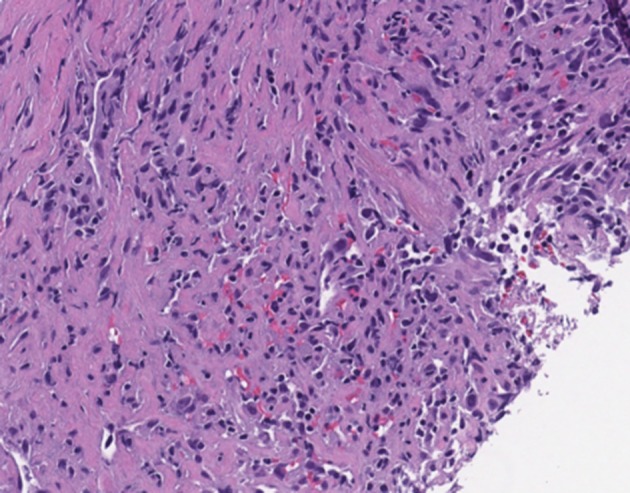
Histological analysis of lung tumour biopsy showing predominantly spindle cells with augmented mitotic activity and necrosis.
On resolution of complications of biopsy a month later, a repeat PET/CT was performed and showed a further increase in size and activity of the right upper lobe tumour now measuring 3×2 cm with standardised uptake value (SUV) of 22.2 (figure 3A), as well as three new FDG-avid foci suspicious for metastasis. These intramuscular lesions were located in the left lateral neck, left posterior upper chest, and there was also a small paraspinal L3 nodule (figure 3B). The L3 paraspinal nodule was biopsied and revealed skeletal muscle with rare degenerating fibres and no tumour present. Despite this negative biopsy result of the L3 paraspinal nodule, concern for metastatic disease in the neck was discussed between the thoracic surgeon, medical oncologist and radiation oncologist. Given the rapid growth of disease, coupled with the patient’s diminished pulmonary function tests, a multidisciplinary team decision was made in favour of SBRT for local control.
Figure 3.
PET/CT findings. (A) 3×2 cm FDG-avid multilobulated mass that had increased in size from previous CT chest. (B) FDG uptake within a small soft tissue mass abutting the right aspect of the L3 posterior process with SUV of 6.2. FDG, fluorodeoxyglucose; PET, positron emission tomography.
Treatment
The patient was dispositioned to receive SBRT with a total dose of 54 Gy in three fractions to the right upper lobe tumour as curative treatment of clinical stage IIA PSCC (figure 4).
Figure 4.

Radiation treatment plan for SBRT to right upper lobe tumour with a total dose of 54 Gy. SBRT, stereotactic body radiation therapy.
Surveillance imaging after completion of SBRT to the right upper lobe tumour showed progressive intramuscular implants in the left neck that had significantly increased in size since previous PET-CT done 2 months prior. One of the lesions in the paraspinal muscles of left upper neck had significantly increased from a prior size of 1.0 cm in the axial plane to 1.9×1.7 cm with features of central necrosis and enhancing septations as well as ring enhancement (figure 5). There were also new pulmonary metastasis in the left upper lung and a ring-enhancing metastasis in the right parieto-occipital lobe confirmed with an MRI brain. Ultrasound-guided biopsy of the left neck intramuscular lesion confirmed metastatic SpCC.
Figure 5.
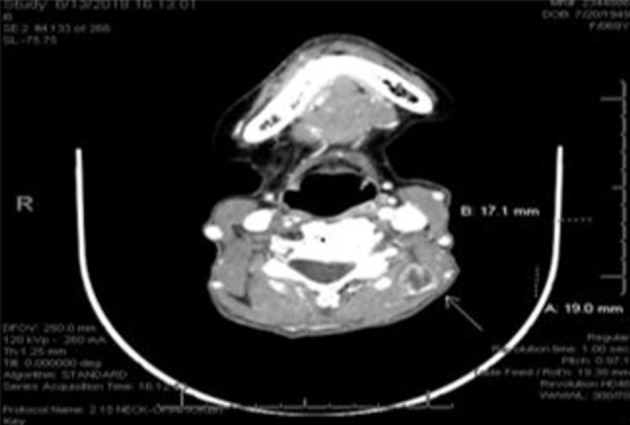
CT neck showing progressive left paraspinal upper neck intramuscular metastasis 1.9×1.7 cm (arrow).
At this time, systemic monotherapy with pembrolizumab 200 mg intravenously every 3 weeks was initiated with primary tumour PD-L1 expression of 90%. She was also dispositioned to receive stereotactic radiosurgery for treatment of the brain metastasis.
However, before stereotactic radiosurgery could be performed, the patient was hospitalised for ileocecal intussusception secondary to multiple small bowel metastases. CT of the abdomen and pelvis at the time also showed new right adrenal gland metastatic implants. Surgical intervention with exploratory laparotomy for reduction of intussusception was conducted successfully without complications. She was discharged without incident but was readmitted a week later for recurrent malignant intussusception. She was not a candidate for further surgical intervention due to multifocal disease and comorbidities. Her small bowel intussusception was therefore managed with small oral challenges that lead to spontaneous resolution.
Following discharge from hospital, she went on to receive stereotactic radiosurgery to the right parieto-occipital and new left frontal lobe metastasis found on follow-up MRI brain. Prescription dose to both sites were 20 Gy each with gamma angle at 90°. She continues to receive pembrolizumab as systemic therapy with a goal of life prolongation.
Outcome and follow-up
Following the completion of two cycles of pembrolizumab and at about 2 months post-SBRT to the primary tumour, PET-CT revealed evidence of significant response to therapy with a decrease in FDG avidity and good local control of right upper lobe mass, shrinkage of the left apical nodule and resolution of intramuscular chest wall and neck avidity (figure 6). No evidence of disease was noted in the bowel and adrenal glands. MRI brain at this time also showed a decrease in size of the right occipital lobe lesion compared with previous examination. Follow-up imaging at 6 months post-SBRT showed continued regression of the right upper lobe (RUL) primary tumour.
Figure 6.
PET-CT prior to treatment compared to 4 months after SBRT to primary tumour and two subsequent cycles of pembrolizumab. (A, B) Significant decrease in size of right upper lobe mass that became mostly cavitary and much less FDG avid. (C, D) Complete resolution of left neck intramuscular FDG avid lesion. FDG, fluorodeoxyglucose; PET, positron emission tomography; SBRT, stereotactic body radiation therapy.
Discussion
PSCC only accounts for about 0.4% of all lung cancers. As a result of this low incidence, limited literature exists on the clinical features, treatment options and progression of this disease.1 4 Despite its generally poor prognosis, treatment options for PSCC are the same as for other non-small cell lung carcinomas (NSCLC) including surgery, chemotherapy/immunotherapy and radiation therapy.5 Pembrolizumab as the choice for monotherapy is based on the results of Phase I/II KEYNOTE-001 study in NSCLC patients.6 Li et al also reported that traditional Chinese medicine may have a role in improving survival in patients with PSCC.7 Due to the rapid progression of disease and widely metastatic nature of PSCC, many patients initially present with extensive stage IV disease, and therefore little is documented about the role of local control with surgery or radiation therapy in these patients.
In our case, the tumour was detected on routine CT chest which is not unusual for PSCC as reported in previous literature by Morimoto et al and Matsi and Kitagawa.8 9 Her symptoms at presentation could be attributed to her longstanding emphysema rather than PSCC. SpCC was diagnosed on biopsy showing an abundance of spindle cells with hyperchromic nuclei and high mitotic activity.1 A large proportion of sarcomatoid cancers, including SpCC, are positive for high PD-L1 expression and although PD-L1 expression has been shown to confer a worse prognosis for these patients, it provides a caveat for targeted immunotherapy with pembrolizumab.10
The high mitotic activity of SpCC confers the highly malignant nature of PSCC as evident in our patient who rapidly progressed to stage IV disease. This case supports SBRT as a reasonable modality to achieve local control of PSCC especially at the earlier stages of disease. It is well tolerated with an extensively documented good safety profile.11 Nevertheless, PSCCs are highly metastatic cancers so systemic therapy is needed to improve overall survival as evidenced by this patient’s significant response to pembrolizumab.
Learning points.
Pulmonary spindle cell carcinoma (PSCC) is a rare tumour with high propensity for distant metastasis and usually carries a poor prognosis.
Stereotactic body radiation therapy is a reasonable modality to achieve good local control of PSCC especially in patients who are not candidates.
Systemic therapy is important in improving overall survival of these patients.
Footnotes
Contributors: Supervised by SJG. Patient was under the care of SJG, AAV and CL. Report was written by MDA and edited by SJG, AAV and CL.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Terada T. Spindle cell carcinoma of the lung: frequency, clinical features, and immunohistochemical studies of three cases. Respir Med CME 2010;3:241–5. 10.1016/j.rmedc.2009.10.003 [DOI] [Google Scholar]
- 2.Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health organization classification of lung tumors. J Thorac Oncol 2015;10:1243–60. 10.1097/JTO.0000000000000630 [DOI] [PubMed] [Google Scholar]
- 3.DJ Q, Liu B, Feng L, et al. Pulmonary spindle cell carcinoma with unusual morphology: a rare case report and review of the literature. Medicine;2017969240:e7129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mainwaring MG, Poor C, Zander DS, et al. Complete remission of pulmonary spindle cell carcinoma after treatment with oral germanium sesquioxide. Chest 2000;117:591–3. 10.1378/chest.117.2.591 [DOI] [PubMed] [Google Scholar]
- 5.Sardar M, Azharuddin M, Khan WJ, et al. Spindle cell carcinoma of the Lung/Pleura: an incidental finding. Cureus 2018;10:e2848. 10.7759/cureus.2848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 2015;372:2018–28. 10.1056/NEJMoa1501824 [DOI] [PubMed] [Google Scholar]
- 7.Li W, Chen M, Zhao Y. Long-Term survival in a patient with pulmonary spindle cell carcinoma treated with traditional Chinese medicine. Case Reports 2018;2018:225989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morimoto M, Osaki T, Kodate M, et al. Spindle cell carcinoma of the lung. Gen Thorac Cardiovasc Surg 2011;59:129–32. 10.1007/s11748-010-0607-x [DOI] [PubMed] [Google Scholar]
- 9.Matsui K, Kitagawa M. Spindle cell carcinoma of the lung. A clinicopathologic study of three cases. Cancer 1991;67:2361–7. [DOI] [PubMed] [Google Scholar]
- 10.Yvorel V, Patoir A, Casteillo F, et al. Pd-L1 expression in pleomorphic, spindle cell and giant cell carcinoma of the lung is related to TTF-1, p40 expression and might indicate a worse prognosis. PLoS One 2017;12:e0180346. 10.1371/journal.pone.0180346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao J, Yorke ED, Li L, et al. Simple factors associated with radiation-induced lung toxicity after stereotactic body radiation therapy of the thorax: a pooled analysis of 88 studies. Int J Radiat Oncol Biol Phys 2016;95:1357–66. 10.1016/j.ijrobp.2016.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]