Dear Editor,
Facing the COVID-19 pandemic, we agree with Ying Shao and colleagues that hospital management strategies have to be improved, not only in psychiatric wards but in all hospitals (Shao et al., 2020). During a long period starting from Jan 2020, shortage of hospital beds for COVID-19 was a serious public concern in Wuhan. It has been reported that the Fangcang shelter hospitals could be a powerful component of national responses to the pandemic, because these instant facilitates could rapidly increase the bed capacity of whole city (Chen et al., 2020). Nevertheless, at the beginning of COVID-19 epidemic in Wuhan, the number of COVID-19 patients dramatically increased so that six batches of designated hospitals were forced to operate continuously in order to take care of the patients. From Jan 21st to Mar 6th, 2020, a total of 86 hospitals were transformed to accept fever/COVID-19 patients only. Wuhan Red Cross Hospital (WRCH), a general hospital and a trusteeship hospital of Union Hospital, Tongji Medical College, happened to be the first one in these designated hospitals that turned into a healthcare system specialized in treating COVID-19 patients.
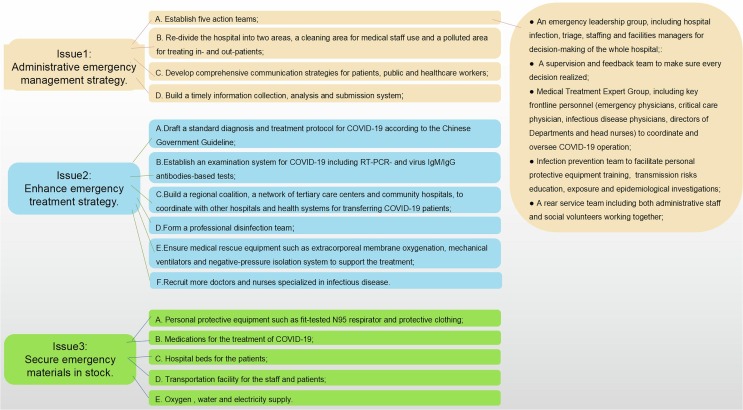
Although there was no protocol available on how to urgently transform a general hospital into an infectious disease hospital, at WRCH we changed our outpatients department into fever patients-only clinic in 8 h and completed a ten-step reform of the whole hospital within 48 h. As the first step, we set up a full time emergency leading group, an infection prevention team and a Medical Treatment Expert Group to coordinate and oversee COVID-19 operation for the whole hospital. Meanwhile, re-dividing WRCH into cleaning area for medical staff use and polluted area for treating in- and out-patients. Five passageways including patient channel, employee channel, administrative personnel channel, cleaning personnel channel and sewage channel were established to meet the requirements of hospital infection protection. Second, search for all kinds of personal protective equipment actively such as fit-tested N95 respirator and protective clothing from local and government resources. Moreover, to minimize transmission, a surgical mask was given to each patient. Third, urgently purchasing medical rescue equipment such as extracorporeal membrane oxygenation, mechanical ventilators, liquid oxygen tanks providing ample oxygen, and negative-pressure isolation system to support the treatment. Fourth, training all medical staff with infectious disease hospital instructions for self-protection and COVID-19 treatment with a standard protocol of Chinese Guideline. Fifth, to increase the bed capacity and reduce cross infection, patients without fever were all discharged within 24 h, allowing hundreds of fever patients admitted the next day. Sixth, recruiting more doctors and nurses specialized in infectious and respiratory disease. Fortunately, expert teams from Wuhan Union Hospital and Sichuan province came to strengthen the treatment forces. Seventh, rebuiding two intensive care units as there were abundant critically ill COVID-19 patients requiring advance therapies such as mechanical ventilation and ECMO (MacLaren et al., 2020). Eighth, we explored building regional coalition, a network of tertiary care centers and community hospitals, to coordinate other hospitals and health systems for transferring the COVID-19 patients. Ninth, establishing a telehealth network to perform multidisciplinary team consultation for COVID-19 patients both in our hospital system and between different hospitals. Tenth, a rear service team formed, including both our administrative staff and social volunteers, working together with greatest efforts to fully ensure the clothing, food, housing, travel and safety of key frontline personnel and steady operation of the hospital (Montemurro, 2020). With Steps 1 and 3 recently endorsed (Chopra et al., 2020), we now summarize all emergency management strategies in Fig. 1 .
Fig. 1.
Management strategies in emergent hospital reform for COVID-19.
Until Mar 19th, 2020, reformed WRCH had received 15,000 + outpatients with fever, treated and discharged 1206 inpatients with COVID-19. Hopefully, our experience could be useful for other hospitals in similar epidemic situations.
Author contributions
JL, QZ and XF drafted the manuscript and share first authorship. NX and ZL revised the final manuscript. NL, CH collected the data and NX is responsible for summarizing all data.
Funding
This work was supported by grants 2016YFC1306600 (to NX) and 2018YFC1314700 (to NX) from the National Key R&D Program of China, grants 81873782 (to NX) National Natural Science Foundation of China.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Chen Simiao, Zhang Zongjiu, Yang Juntao, Wang Jian, Zhai Xiaohui, Bärnighausen Till, Wang Chen. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. The Lancet. 2020;395(10232):1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra Vineet, Toner Eric, Waldhorn Richard, Washer Laraine. How Should U.S. Hospitals Prepare for Coronavirus Disease 2019 (COVID-19)? Ann. Intern. Med. 2020;172(9):621. doi: 10.7326/M20-0907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLaren G., Fisher D., Brodie D. Preparing for the Most Critically Ill Patients With COVID-19: The Potential Role of Extracorporeal Membrane Oxygenation. JAMA. 2020 doi: 10.1001/jama.2020.2342. [DOI] [PubMed] [Google Scholar]
- Montemurro N. The emotional impact of COVID-19: From medical staff to common people. Behav. Immun. Brain. 2020 doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Y., Shao Y., Fei J.M. Psychiatry hospital management facing COVID- 19: From medical staff to patients. Behav. Immun. Brain. 2020 doi: 10.1016/j.bbi.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]