The coronavirus disease 2019 (COVID-19) pandemic has accelerated the widespread adoption of collaboration and communication software to enable medical care at a distance1 and reduce the risk of transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) between patients and health-care providers from gathering together in hospitals, offices, or clinics. Most virtual care solutions have been implemented to ensure adequate physical distancing between patients and health-care providers, while ensuring that patients without COVID-19 can still access ambulatory care for acute or chronic medical conditions. Although previous efforts to expand virtual care offerings have been met with resistance, the COVID-19 pandemic has highlighted the tremendous value of care delivery at a distance to prevent contagion, but also to provide access to care under these extraordinary circumstances. As a culture, we have learned that many of the patients or providers we had previously deemed too uncomfortable or inept at using technology have actually become quite proficient with videoconferencing for shopping, exercise, socialising, and learning.
For the past two decades, our academic medical centre and others have been building capability in ambulatory virtual visits in specialty care, virtual urgent care for minor complaints, and interfacility emergency virtual consults for time-sensitive conditions like acute stroke.2, 3, 4, 5 These efforts have been rudimentary at most institutions due to complex technology integration, substantial regulatory barriers, and a lack of reimbursement. One of the greatest criticisms of virtual care in the past has been its depersonalisation of the patient–provider experience, which is too distant for the intimate connection required for good care.6 Ironically, this attribute of care delivery at a distance is now virtual care's greatest asset. Providers are scrambling to provide options that ensure safe, effective, and equitable access to care for patients in the setting of relaxed regulations and broader reimbursement. Here we describe two innovations in virtual care delivery that have been developed and deployed across our organisation, virtual rounds and a virtual intercom communication system, and give suggestions for how these innovations might be implemented at other institutions.
Maintaining an adequate supply of health-care workers is vital to reducing mortality due to COVID-19. Many health-care systems have struggled to preserve members of the workforce after community spread has begun. At our hospital (Massachusetts General Hospital, Boston, MA, USA) at the start of the epidemic, health-care workers who were exposed to COVID-19 were removed from patient contact until they were asymptomatic or had tested negative. After learning that in one morning (March 16, 2020) 60 health-care workers at our hospital had potential exposures to COVID-19 that required them to be confined to home isolation for several days pending test results, we realised that traditional medical rounds were a communal activity with large numbers of health-care workers frequently huddled together around a computer screen or test results, discussing clinical management, reviewing abnormal findings on radiological images, or discussing findings from examinations. To implement physical distancing among our health-care workers, who often gathered in multidisciplinary groups of eight to ten individuals, we created virtual rounds as a means of so-called medical distancing. In this model, one or two health-care workers are physically present on the ward, while all others join remotely via collaboration software (Microsoft Teams, Microsoft Corporation, Redmond, WA, USA) from home or other locations in the hospital (figure 1 ). This approach creates a digital replica of normal medical rounds, preserving the intimacy of group work, social supports, task management (eg, order entry, note writing, consulting colleagues), and image sharing while avoiding the dense clustering of individuals. Also, no longer constrained by physical space, members of the virtual rounds can invite others to join in with daily work, such as pharmacists, allied health professionals, coordinators, quality staff, and case management staff. Scribes to support documentation and other support staff can easily be incorporated into virtual rounds. This approach also allows providers in self-isolation to continue to contribute meaningfully and support their teammates. Virtual teams might experience less psychological trauma caused by physical distancing and wearing personal protective equipment (PPE), and enable otherwise non-essential personnel and student trainees (who have been frequently removed from hospital settings during the pandemic) to re-join the workforce, thereby creating a scalable platform for knowledge sharing and collaborative teams between facilities to help with load balancing as needed across health systems.
Figure 1.
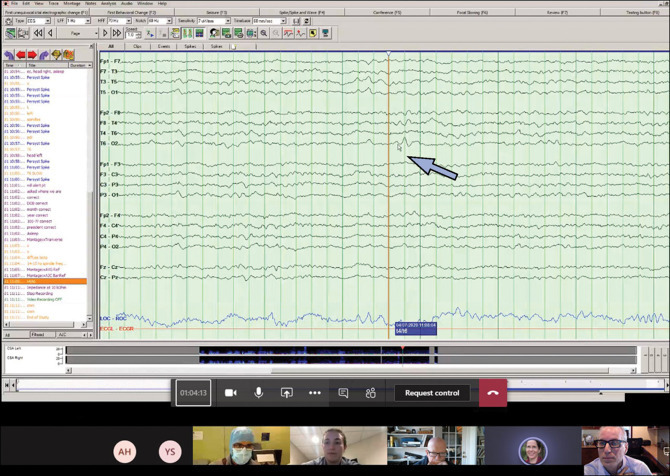
Screenshot taken during a virtual round
The screenshot is from the perspective of a home-based participant (LHS; lower right video panel) joining rounds, while six other teams members have joined from their own devices and are shown in the lower row of images as icons or actual video capture. A patient with suspected seizures is being reviewed, and an area of frontotemporal phase reversing spikes is highlighted by the on-screen white cursor controlled by the attending physician, indicated here for clarity with the large blue arrow.
We encountered several challenges with the development of this model. The process involved reconfiguring a previously purchased, unit-based, portable laptop computer used by the medical team during normal medical rounds, so that it could launch and run the collaborative software. All team members were invited from our corporate network directory to a standing recurring meeting for daily rounds, and could join or leave as needed repeatedly during the morning as the onsite providers moved from room to room on the ward. Because only individuals in our organisation were invited to the daily rounds, and all parties were visible and known during rounds to the other participants, patient privacy and security were always maintained and a business associated agreement between our hospital system and Microsoft continues to further ensure that proper privacy and security standards are met. Information systems personnel helped support and train new teams as the virtual rounds programme spread across medical and subspecialty services in our health system. Team members were instructed not to forward the invite to individuals outside of the medical team. For patients who were known to be positive for COVID-19, the laptop was not brought into the room and the exam was described afterwards. For patients without COVID-19, the laptop was brought into the room and pointed at the patient during the exam so all team members could see the findings. The laptop was only controlled by the attending physician and was wiped down with a cloth and sanitising solution at the end of rounds each day. Because the attending physician was physically present on rounds, notes and billing processes followed usual practice. Ongoing research will study factors associated with adoption, user satisfaction, frequency of safety reports, and costs of support and maintenance.
Another aspect of this pandemic is the social isolation of the sick and dying because hospitals have restricted visitors, including for those on ventilator support in intensive care.7 To reduce use of PPE and physical contact time for health-care workers assigned to patients with COVID-19, we deployed a video intercom communication system that allows a nurse or consultant to connect via any device to a securely configured tablet computer mounted securely on an IV pole with a variety of commercially available and specially designed brackets (figure 2 ). The configuration of the tablet computer is locked and has an auto-answer feature enabled so nurses can monitor patients without disturbing them, and engage in high-quality two-way conversations whenever needed without the patient having to take any action. This approach preserves human contact and capacity for increased human connection with patients because the patient can see the nurse's full face and facial expressions without a mask and goggles, and the interactions can be less rushed. When physiological monitor alerts require immediate patient observation, nurses can swiftly appear on the screen from anywhere in the hospital. This video intercom is now widely deployed across our health system, with over 1500 units deployed as of April 29, 2020, with over 2600 video sessions per day. The devices are enabled with commercially available videoconferencing software (Vidyo [Hackensack, NJ, USA] and SBR Health [Cambridge, MA, USA]) and centrally managed with access to the software distributed through an enterprise application system to all authorised users or managed clinical computers and handheld devices.
Figure 2.
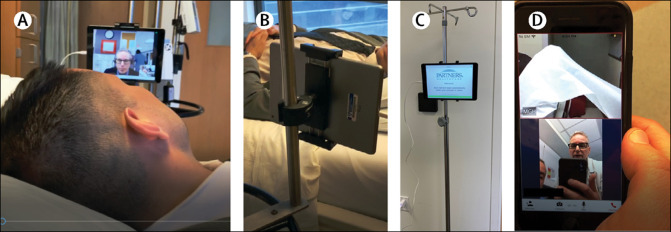
The video intercom communications system
The system is displayed from the perspective of simulated patient (JE) who is speaking with a health-care worker (LHS) who is using a desktop computer and headphones for enhanced patient privacy (A). A back (B) and front (C) view of the system deployed in a patient room, and a nurse accessing the device on a hospital-configured and hospital-issued smartphone device (D).
Although we have not had the time or opportunity to design a controlled trial of the effect of the virtual intercom communication system on patient experience, anecdotal reports from nursing leadership and patients has been overwhelmingly positive, and in the initial deployment, of the 45 min required for a typical nursing admission, more than 70% of the duration of the admission process was done over the virtual intercom communication system, with the nurse outside of the room. The main challenge we have encountered has been deploying sufficient technical support for these devices that are now considered critical, being used 24 h a day, 7 days a week, and the need to reset devices sporadically for network disconnections. Medical interpreters can now join any virtual intercom communication system encounter, and the platform will soon be expanded to other devices to allow access from a central physiological monitoring hub, and bring families and others to the bedside virtually.8 High rates of depression, anxiety, and post-traumatic stress disorders have been diagnosed in patients and health-care workers after COVID-19-related care episodes.9 The profound social isolation of being quarantined in a hospital room without visitors and with little or no human contact, other than brief visits from people wearing full PPE, might also contribute to worse health outcomes. The virtual intercom communication system platform and other virtual care solutions could allow family members, social workers, health-care professionals, and medical interpreters to spend the time with patients that is necessary to increase their understanding of the disease process, medical management plan, and support serious illness conversations, to name just a few benefits.
Some have likened this surge of digital activity to the rural electrification project of the 1930s that extended modern industrial society to even the most remote parts of the USA.10 This digital surge portends the clinical COVID-19 surge, and has faced its own challenges, as internet service providers and videoconferencing platforms struggle under the load and occasionally have service brownouts or blackouts. But the mainstreaming of digital health tools and collaboration software will be one of the few positives to come from this pandemic, and many of the new digital skills and innovations are likely to remain long after the pandemic has resolved. Our health-care system will have taken a giant step towards modernisation, with the potential for greater efficiency in care delivery and increased value in health care. If appropriate reimbursement for virtual care becomes an expectation rather than the exception, it will open up new avenues of care delivery and lay the groundwork for major advances in machine learning and artificial intelligence, and the integration of these advances into routine care delivery.
The traditional methodical and cautious roll-out of information technology in medicine must shift overnight to agile implementations of minimum viable products. These new innovations must rapidly embed themselves into existing support structures and then evolve iteratively to ensure medical grade reliability and quality and avoid the chaos of an explosion of small-scale innovations without support or institutional backing. Lives are at stake, and time is of the essence.
This online publication has been corrected. The corrected version first appeared at thelancet.com/digital-health on May 8, 2020
Acknowledgments
LHS reports grants from the US National Institute of Neurological Disorders and Stroke and the Patient-Centered Outcomes Research Institute and personal fees from LifeImage outside of the submitted work. All other authors declare no competing interests. We thank Benjamin Meller and Keith Jennings for their help in designing and implementing the virtual rounds and video intercom solutions, and Michael Bowley, who led the clinical implementation pilot at Massachusetts General Hospital.
References
- 1.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMp2003539. published online March 11. [DOI] [PubMed] [Google Scholar]
- 2.Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40–44. [PubMed] [Google Scholar]
- 3.Schwamm LH. Telehealth: seven strategies to successfully implement disruptive technology and transform health care. Health Aff (Millwood) 2014;33:200–206. doi: 10.1377/hlthaff.2013.1021. [DOI] [PubMed] [Google Scholar]
- 4.Shah SJ, Schwamm LH, Cohen AB, et al. Virtual visits partially replaced in-person visits in an ACO-based medical specialty practice. Health Aff (Millwood) 2018;37:2045–2051. doi: 10.1377/hlthaff.2018.05105. [DOI] [PubMed] [Google Scholar]
- 5.Silva GS, Farrell S, Shandra E, Viswanathan A, Schwamm LH. The status of telestroke in the United States: a survey of currently active stroke telemedicine programs. Stroke. 2012;43:2078–2085. doi: 10.1161/STROKEAHA.111.645861. [DOI] [PubMed] [Google Scholar]
- 6.Miller EA. The technical and interpersonal aspects of telemedicine: effects on doctor-patient communication. J Telemed Telecare. 2003;9:1–7. doi: 10.1258/135763303321159611. [DOI] [PubMed] [Google Scholar]
- 7.Hendin A, La Rivière CG, Williscroft DM, O'Connor E, Hughes J, Fischer LM. End-of-life care in the emergency department for the patient imminently dying of a highly transmissible acute respiratory infection (such as COVID-19) CJEM. 2020 doi: 10.1017/cem.2020.352. published online March 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armitage R, Nellums LB. The COVID-19 response must be disability inclusive. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30076-1. published online March 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou X, Snoswell CL, Harding LE, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E Health. 2020;26:377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 10.Lewis J, Severnini E. Short- and long-run impacts of rural electrification: evidence from the historical rollout of the U.S. power grid. J Dev Econ. 2020;143 [Google Scholar]


