The new coronavirus disease 2019 (COVID-19) which was first identified in the population of Wuhan/China in December of last year, has quickly expanded across the globe, with the World Health Organization (WHO) declaring it a pandemic on March 11 2020.
As of April 28 2020 [1], there have been more than 3 million documented infections worldwide with more than 200,000 associated deaths. Of significant concern, after the spread of the infection outside China, several countries have experienced an exponential rise in the number of identified cases, with Italy now reporting more than 6 times the number of deaths in China and the U.S having surpassed China as the most affected country with over 1 million identified cases, almost one third of them in the state of New York, a major epicenter of the disease. The costs of the COVID-19 pandemic have been significant, with marked economic disruption due to the widespread lockdowns for disease containment, increased jobless claims, high likelihood of a global recession and major changes in ordinary social relationships due to the recommended social distancing measures.
This worldwide healthcare problem, which has led to a deep breakdown of the previous modus operandi of most societies, has also inevitably affected the medical profession. Of notice, COVID-19 infections have higher morbidity and mortality rates in the elderly population. Due to the known natural progression of degenerative spinal changes with the aging process [2], this subgroup also has the greatest burden of spinal disorders requiring surgical attention. However, taking into account the relatively low percentage of infection in the total population, the direct impact of COVID-19 pandemic related to possible delays of surgical care in infected patients seems relatively small in the grand scheme. Overall, the indirect effects of the COVID-19 pandemic upon spinal care seems far more meaningful and noticeable. Such a deleterious impact can be traced to several factors such as the reallocation of hospital resources (such as nursing staff and ICU beds) to the care of patients with the coronavirus as well as cancellation of elective surgeries and office visits in order to reduce the chances of disease spread. The combination of both of these has led to sudden and drastic changes in the daily routine of not only spine surgeons but also of other professionals involved in spine care, such as pain management and rehabilitation physicians, physical therapists and occupational therapists. Such effects have been even more pronounced after several U.S. states and counties decreed ‘shelter-in-place’ policies. Another associated concern is the possible discharge of postoperative patients to nursing homes, rehabilitation and other long-term care facilities, especially when considering the tragic experience of a nursing home in Kirkland, Washington state, which witnessed a cluster of 35 COVID-19 related deaths among its 120 residents and 180 staff [3]. Finally, from an educational standpoint, it seems important to highlight that the CDC recommendations against gatherings of more than 10 people has also affected the daily routine of surgical training, with grand rounds and multidisciplinary meetings being either cancelled or held virtually. In addition to a possible detrimental effect upon residents training, the associated drop in operative cases due to OR restrictions may also have real implications for their graduation, especially taking into account that the Accreditation Council for Graduate Medical Education (ACMGE) has officially released a statement emphasizing that the minimum caseload requirements for trainees in surgical specialties will not be changed despite the COVID-19 pandemic [4].
From the patients’ perspective, the uncertainty of when they will be able to obtain surgery (or even alternative treatments such as injections) is likely associated with a degree pain, suffering and anxiety which seems challenging to properly quantify, but which could be quite meaningful for some patients. Moreover, in the same way previous studies have demonstrated that a breakdown in adequate patient-physician relationship may be associated with increased Emergency Department (ED) visits in the perioperative period [5], the relative lack of access to healthcare resources which is likely being experienced by a significant number of patients may also lead to increased number of unnecessary ED visits as well as increased opioid use. An additional concern is the possibility (or reality) of losing healthcare insurance due to layoffs. This is all the more meaningful as recent reports have estimated that the unemployment rate in the U.S. is currently above 20% [6], the highest level since the Great Depression, with 26.5 million additional people having been included to the list of those requiring unemployment benefit since the beginning of the pandemic in the U.S.
Finally, the COVID-19 pandemic has also greatly affected the daily operations of several healthcare industries. Such deleterious systemic effects tend to percolate throughout the whole healthcare environment, with negative consequences upon ongoing clinical trials (mainly related to cessation of patient enrollment as well as cancelled follow-up visits, imaging and laboratory tests). All of these tend to extend the required time for the completion of clinical studies, data analysis and FDA approval, with increased total costs for bringing such new technologies and drugs to the market [7].
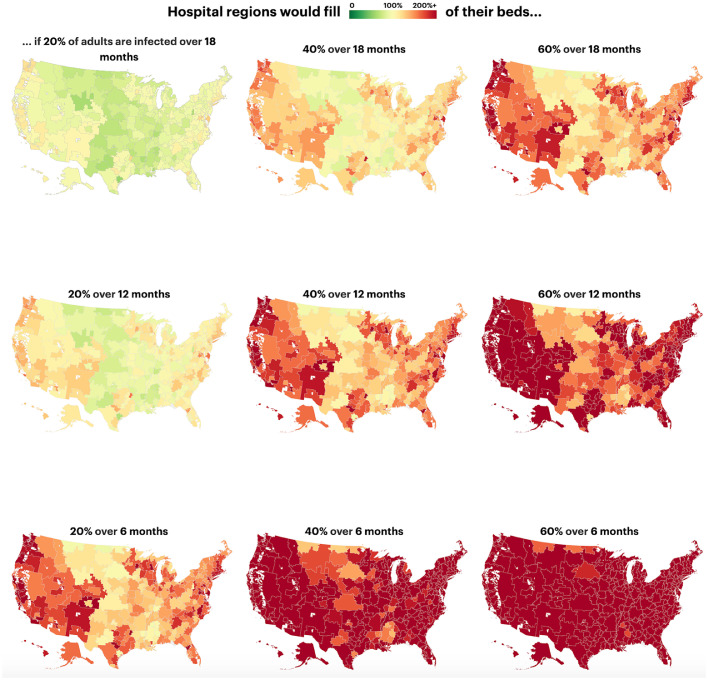
Taking into account the magnitude of the worldwide healthcare challenge associated with the COVID-19 pandemic (a process which bears all the features of a complex system, such as unpredictability, recurrent feedback loops as well as non-linear and iterative effects) [8], it seems inappropriate to consider even harsh restrictions unreasonable, especially considering the degree of epistemic uncertainty regarding the current prevalence, spreading patterns and long-term effects of this pandemic. As illustrated by a recent report in Science, an observational study in conjunction with mobility data, a networked dynamic metapopulation model and Bayesian inference [9], approximately 86% of all COVID-19 infections may be undocumented. This suggests that the total number of infections worldwide may be at least one order of magnitude higher than those in the official reports. Such estimations are corroborated by a recent study which suggested that the estimated proportion of people in NY city with positive antibodies for COVID-19 was approximately 21.2%. This would correspond to roughly 1.7 million NY city residents having been exposed to the disease, while official statistics report only 138,000 confirmed positive cases in the region [20]. Another worrisome report was recently released by the Harvard Global Health Institute [10]. Using data on COVID-19 patients, the model compares the amount of necessary hospital and ICU beds in each hypothetical evolution scenario for the pandemic with the actual numbers of beds available on a state-by-state basis. Assuming a hospitalization rate of 19% for those under 65 years and 28.5% for those over 65 years and an ICU rate of 19% for those hospitalized under 65 and 28.5% for those hospitalized over 65, even in a relatively low infection rate scenario (in which 20% of the population would become infected in 6 months) in the vast majority of states the number of necessary beds would exceed the current total capacity. In the moderate scenario, in which 40% of the population would become infected in 6 months, the number of necessary hospital beds would be more than 200% of the current capacity (Fig. 1).
Fig. 1.
Infographic showing the percentage of beds which would be occupied in each possible scenario of evolution of the COVID-19 pandemic in the U.S.
Reproduced under the Creative Commons license from Annie Waldman, Al Shaw, Ash Ngu, and Sean Campbell, Are Hospitals Near Me Ready for Coronavirus? Here Are Nine Different Scenarios. Propublica - March 17, 2020
As once stated by Donald Rumsfeld, then U.S. Secretary of State for Defense in February 2002: “There are “known knowns”. There are things we know that we know. There are “known unknowns”. That is to say, there are things that we now know we don’t know. But there are also “unknown unknowns”. There are things we do not know we don’t know.” [11] The latter seems clearly the most dangerous category as much in healthcare as it is in the field of national security, as clear awareness of (or even a hint of knowledge about) our degree of ignorance seems much better than the potentially catastrophic nature of absolute ignorance. In the face of “uknown unknowns”, prudence seems always to be the wisest attitude.
Although not specifically pertaining to our specialty (I am personally not aware of any report of spinal disorders related to the COVID-19 pandemic, although there has been a recent report of a COVID-19 associated acute hemorrhagic necrotizing encephalopathy) [12], in such unprecedented situation a great degree of flexibility and adaptation has been required of spine care providers in order to continue offering care. To achieve such goals, many spine surgeons have provided contributions to their institutions in establishing alternatives modes of care, including the adoption of telemedicine consults for post-operative evaluations and wound checks as well as triage teams to differentiate between urgent and elective referrals and surgeries. Although the specific details of the policy may vary from hospital to hospital, as a general rule any spinal disorder for which a delay of 6 to 8 weeks is not likely to compromise the standard of care, has been considered non-urgent and, therefore, have been temporarily postponed. This still leaves a substantial subgroup of patients with acute or progressive neurological deficits, spinal tumors, spinal infections as well as spinal instability which require proper triage for urgent of emergent attention.
Despite some concerns regarding the apparent ineffectiveness of warnings and recommendations from health experts upon official public policy [13], the scientific community as a whole should be congratulated for their meaningful efforts to properly address the COVID-19 pandemic. While numbers of infected cases officially reported by China have been seen with distrust by U.S. intelligence experts [14], the newly established Coronavirus Research Center at Johns Hopkins University [1] is a politically independent and scientifically reliable cornerstone for tracking the statistics of the COVID-19 pandemic spread worldwide. A collaborative effort by researchers across several organizations in partnership with the National Library of Medicine (NLM) at the National Institutes of Health (NIH), Microsoft and the Allen Institute for Artificial Intelligence has launched the Covid-19 Open Research Dataset (CORD-19), a database which already lists more than 57,000 scholarly articles from peer-reviewed journals as well as unpublished research in the form of bioRxiv and medRxiv. Additionally, experts working in several academic institutions as well as biotechnology companies and governmental institutions around the world (including the National Institute of Allergy and Infectious Diseases) are actively engaged in the development of new prevention strategies, such as vaccines [15], and in the proper scientific evaluation of the safety and efficacy of possible therapeutic candidates such as hydroxichloroquine [16] and remdesivir [17] (among others) [18] through prospective randomized clinical trials.
As a spine surgery community we are committed to both maintaining the standards of excellence in spinal care even (and especially) during critical times, as well as to a proactive attitude in assisting our institutions through our unique insight into the natural history and outcomes of spinal disorders in order to prioritize care and optimize resources allocation.
As stated in a quote often attributed to a famous twentieth century spiritual leader who dedicated her life to the care of the poor, the sick and the destitute: “None of us, including me, ever do great things. But we can all do small things, with great love, and together we can do something wonderful.” [19] This seems a quite timely advice. Although, as spine surgeons, most of us will likely not be directly involved in the critical care of COVID-19 patients or in the development of new drugs and vaccines for it, in such exceptional times it is our responsibility and a great privilege to, through our best efforts, attempt to mitigate the consequences of this pandemic upon our patients.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2020.100003.
Appendix. Supplementary materials
References
- 1.https://coronavirus.jhu.edu/map.html. Accessed on Apr 28, 2020.
- 2.Wang F., Cai F., Shi R., Wang X.H., Wu X.T. Aging and age related stresses: a senescence mechanism of intervertebral disc degeneration. Osteoarthritis Cartilage. 2016;24:398–408. doi: 10.1016/j.joca.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 3.https://www.nytimes.com/2020/03/21/us/coronavirus-nursing-home-kirkland-life-care.html - Accessed on Mar 26, 2020.
- 4.ACGME Response to the Coronavirus (COVID-19) - Mar 18https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19 - Accessed on Apr 8, 2020.
- 5.Levin J.M., Winkelman R.D., Smith G.A., Tanenbaum J.E., Xiao R., Mroz T.E., Steinmetz M.P.6. Emergency department visits after lumbar spine surgery are associated with lower Hospital Consumer Assessment of Healthcare Providers and Systems scores. Spine J. 2018;18:226–233. doi: 10.1016/j.spinee.2017.06.043. [DOI] [PubMed] [Google Scholar]
- 6.Lambert L. Real unemployment rate soars past 20%—and the U.S. has now lost 26.5 million jobs. Apr 23 - https://fortune.com/2020/04/23/us-unemployment-rate-numbers-claims-this-week-total-job-losses-april-23-2020-benefits-claims/ - Accessed on Apr 28, 2020.
- 7.Feuerstein A.As Covid-19 spreads, disruptions to clinical trial and drug development accelerate. STAT. Mar 23 - Accessed on Apr 8, 2020.
- 8.Moore S., Rogers T. Predicting the Speed of Epidemics Spreading in Networks. Phys Rev Lett. 2020;124 doi: 10.1103/PhysRevLett.124.068301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li R., Pei S., Chen B., Song Y., Zhang T., Yang W., Shaman J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020 Mar 16 doi: 10.1126/science.abb3221. pii: eabb3221[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanger-Katz M., Sarah Kliff S., Parlapiano A. These Places Could Run Out of Hospital Beds as Coronavirus Spreads. March 17, 2020 - https://www.nytimes.com/interactive/2020/03/17/upshot/hospital-bed-shortages-coronavirus.html - Accessed on Mar 25, 2020.
- 11.https://archive.defense.gov/Transcripts/Transcript.aspx?TranscriptID=2636 - Accessed on Apr 8, 2020.
- 12.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI Features. Radiology. 2020 Mar 31 doi: 10.1148/radiol.2020201187. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shane Harris, Greg Miller, Josh Dawsey and Ellen Nakashima. U.S. intelligence reports from January and February warned about a likely pandemic. The Washington Post. March 20, 2020 - https://www.washingtonpost.com/national-security/us-intelligence-reports-from-january-and-february-warned-about-a-likely-pandemic/2020/03/20/299d8cda-6ad5-11ea-b5f1-a5a804158597_story.html - Accessed on Mar 26, 2020.
- 14.Wadhams N., Jacobs J.China Concealed Extent of Virus Outbreak, U.S. Intelligence Says. https://www.bloomberg.com/news/articles/2020-04-01/china-concealed-extent-of-virus-outbreak-u-s-intelligence-says?utm_source=twitter&utm_content=politics&cmpid%3D=socialflow-twitter-politics&utm_medium=social&utm_campaign=socialflow-organic - Accessed on Apr 8, 2020.
- 15.Callaway E.Coronavirus vaccines: five key questions as trials begin.Nature. 2020;579:481. doi: 10.1038/d41586-020-00798-8. [DOI] [PubMed]
- 16.Zhou D., Dai S.M., Tong Q.COVID-19: a recommendation to examine the effect of hydroxychloroquine in preventing infection and progression.J Antimicrob Chemother. 202020. pii: dkaa114. doi: 10.1093/jac/dkaa114. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 17.Ko W.C., Rolain J.M., Lee N.Y., Chen P.L., Huang C.T., Lee P.I., Hsueh P.R. Arguments in favour of remdesivir for treating SARS-CoV-2 infections. Int J Antimicrob Agents. 2020;6 doi: 10.1016/j.ijantimicag.2020.105933. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baron S.A., Devaux C., Colson P., Raoult D., Rolain J.M. Teicoplanin: an alternative drug for the treatment of coronavirus COVID-19? Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105944. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.https://www.azquotes.com/quote/534868. Accessed on Mar 26, 2020.
- 20.Antibody Test Estimates 1.7 Million NYC Residents Have Had Coronavirus; 2020. [Accessed 28 Apr 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.