Abstract
BACKGROUND
The prevalence of post-natal depression (PND) is high in India, as it is in many other low to middle income countries. There is an urgent need to identify PND and treat the mother as early as possible. Among the many paper and pencil tests available to identify PND, the Edinburgh Postnatal Depression Scale (EPDS) is a widely used and validated measure in India. However, the summary diagnostic accuracy and clinical utility data are not available for this measure.
AIM
To establish summary data for the global diagnostic accuracy parameter as well as the clinical utility of the non-English versions of the EPDS in India.
METHODS
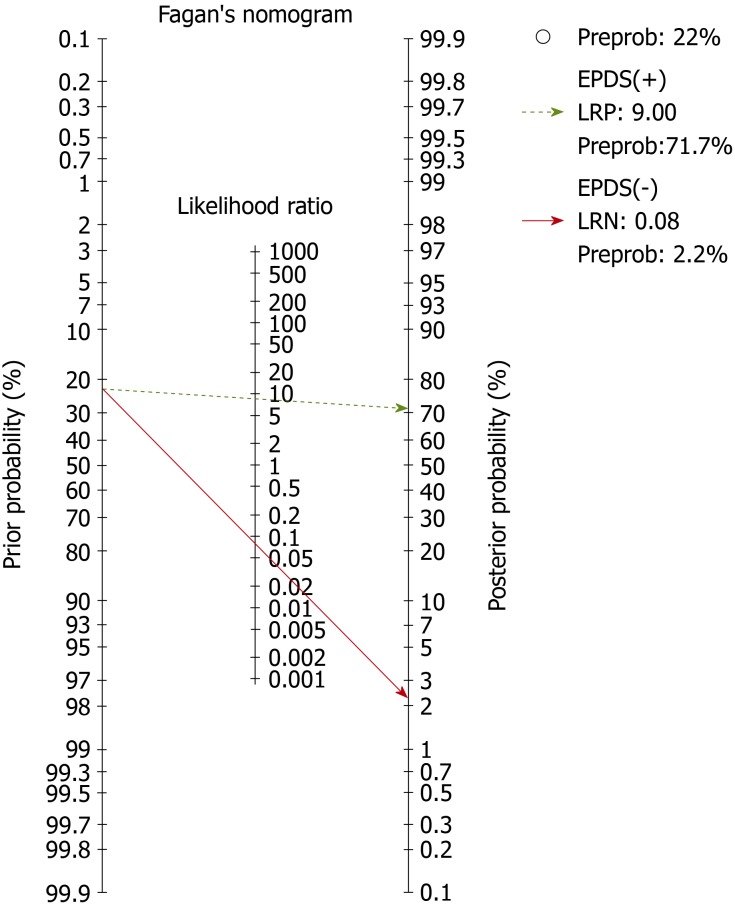
Two researchers independently searched the PubMed, EMBASE, MEDKNOW and IndMED databases for published papers, governmental publications, conference proceedings and grey literature from 2000-2018. Seven studies that evaluated the diagnostic accuracy of EPDS in five Indian languages against DSM/ICD were included in the final analysis. Two other investigators extracted the Participants’ details, Index measures, Comparative reference measures, and Outcomes of diagnostic accuracy data, and appraised the study quality using QUADS-2. Deek’s plots were used to evaluate publication bias. We used the area under the curve of the hierarchical summary area under the receiver operating characteristic curve, with the random effect model, to summarize the global diagnostic accuracy of EPDS. Using the 2 × 2 table, we calculated positive and negative likelihood ratios. From the likelihood ratios, the Fagan’s nomogram was built for evaluating clinical utility using the Bayesian approach. We calculated the 95% confidence interval (95%CI) whenever indicated. STATA (version 15) with MIDAS and METANDI modules were used.
RESULTS
There was no publication bias. The area under the curve for EPDS was 0.97 (95%CI: 0.95-0.98). The pre-test probability for the nomogram was 22%. For a positive likelihood ratio of 9, the positive post-test probability was 72% (95%CI: 68%, 76%) and for a negative LR of 0.08, the negative post-test probability was 2% (95%CI: 1%, 3%).
CONCLUSION
In this meta-analysis, we established the summary global diagnostic parameter and clinical utility of the non-English versions of the EPDS in India. This work demonstrates that these non-English versions are accurate in their diagnosis of PND and can help clinicians in their diagnostic reasoning.
Keywords: Clinical-utility, Diagnostic-accuracy, Edinburgh Postnatal Depression Scale, Meta-analysis, India, Validation
Core tip: Post-natal depression (PND) affects both the mother and baby. Currently, although one of the most common psychiatric disorders among women, early identification and treatment is underprovided in low and middle-income countries. Paper-and-pencil tests remain the primary mode of identifying PND, and the Edinburgh Postnatal Depression Scale is widely used and validated in many languages in India. This meta-analysis documents that the diagnostic parameters are good for Edinburgh Postnatal Depression Scale in India, and that its use can significantly help to scale up the services for PND.
INTRODUCTION
India is a low-middle income country with a birth rate of 20/1000 population, and the summary prevalence of Post-natal Depression (PND) was 22% in the country in 2017[1-3]. There is compelling evidence that PND is associated with morbidity and mortality in the mother-infant dyad[4,5]. Therefore, scaling-up identification and early, effective management of the identified mother-infant dyad is very much needed in India.
The Edinburgh Postnatal Depression Scale (EPDS) is an accurate screening measure[6,7] and improves the follow-up care of PND and maternal mental health[8]. In India, it is the most commonly used screening measure for PND. A recent meta-analysis demonstrates that 29 of the 38 prevalence studies on PND have used EPDS in India[3]. This measure has been translated and validated in the eight regional languages of India: Assamese, Bengali, Gujarati, Kannada, Konkani, Marathi, Punjabi and Tamil, and has been validated in both clinical and community settings in India against a variety of reference standards. The total EPDS threshold score for diagnosing PND has ranged from 6/7 to 12.5/13. Reflecting the possible effect of the varying prevalence of PND, the setting of the study, the threshold-score of EPDS, and the reference standard used or other methodological differences, the sensitivity and specificity have varied from 71%-100% and 77%-98%, respectively (further details are given in Table 1). Furthermore, good diagnostic accuracy does not always translate into good clinical utility among measures. The clinical utility of EPDS has not previously been studied in India. Therefore, because of the wide variation in diagnostic accuracy parameters, there is a need to generate summary diagnostic accuracy parameters from pooled studies for use across India, and its clinical utility needs to be demonstrated.
Table 1.
Summary of the included and excluded studies with their individual Quality Assessment of Diagnostic-Accuracy Studies-2 details
|
PICO details |
QUADAS-2 |
|||||||||||||
|
Risk of bias |
Applicability concerns |
|||||||||||||
| Ref. | Sample, n | Setting, Age, PN | EPDS language | EPDS thres-hold | Interview schedule, Reference standard | Sn | Sp | PS | IT | RS | F&T | PS | IT | RS |
| Patel et al[13], 2002 | 270 | Clinic, 18-40 yr, 6-8 wk PN | Konkani | 11/12 | CIS-R, ICD-10 | 92 | 85 | UC | L | L | UC | UC | UC | UC |
| Benjamin et al[14], 2005 | 121 | Clinic, 17-35 yr, NA-PN | Tamil | 8/9 | CIS-R, ICD-10 | 94.1 | 90.2 | UC | L | UC | UC | L | L | L |
| Werrett and Clifford[15], 2006 | 25 | Clinic, 23-40 yr; 5-8 wk, 10-14 wk PN | Punjabi | 12.5/13 | CIDI, ICD-10 | 71.4 | 93.7 | L | L | L | L | L | L | L |
| Fernandes et al[16], 2011 | 194 | Clinic, 3rd trimester | Kannada | 12/13 | MINI-Plus, DSM-IV | 100 | 84.9 | UC | L | L | UC | L | L | L |
| Desai et al[17], 2011 | 200 | Clinic, 18-35, up to 6 mo PN | Gujarati | 10.5/11 | SSI, DSM-IV | 100 | 98 | UC | L | UC | UC | L | L | L |
| Savarimuthu et al[18], 2012 | 137 | Community 21-30 yr, 4-6 wk PN | Tamil | 6/7 | CI, ICD-10 | 85.3 | 77.7 | UC | L | UC | L | L | L | L |
| Kalita et al[19], 2015 | 200 | Clinic, 18-42 yr, 6 wk PN | Assame-se | 13 | CI, ICD-10 | 88.9 | 85.3 | UC | L | UC | H | L | L | L |
| Maity et al[20], 2015 | 105 | Clinic, NA, NA | Bengali | 13 | NA | 84 | 91 | H | UC | H | H | H | H | H |
| Khapre et al[21], 2017 | 280 | Community, 25 yr median, 2 wk PN | Marathi | 12/13 | SSI, ICD-10 | 93.8 | 94.9 | UC | L | UC | UC | L | L | L |
Patient selection (PS): Describe methods of patient selection; Index text (IT): Describe the index test and how it was conducted and interpreted; Reference standard (RS): Describe the reference standard and how it was conducted and interpreted; Flow and timing (F&T): Describe any patients who did not receive the index tests or reference standard or who were excluded from the 2 × 2 table, and describe the interval and any interventions between index tests and the reference standard; H: High bias (if any signalling question was answered “no,”); L: Low bias (if the answers to all signalling questions for a domain were “yes,”); UC: Unclear (if insufficient data were reported to permit our judgment). PICO: Participants, Index measure, Comparative reference measure and Outcome of diagnostic accuracy; CIS-R: Clinical Interview Schedule (Revised); CI: Clinical Interview; CIDI: Composite international diagnostic interview; ICD-10: International Classification of Diseases, Edition 10; DSM-IV: Diagnostic and Statistical Manual, IVth Edition; MINIPlus: Mini International Neuropsychiatric Interview Plus; SSI: Semi-structured Interview; PN: Post-natal period; NA: Not available; QUADAS-2: Quality Assessment of Diagnostic Accuracy Studies-2.
Using this meta-analysis, we aim to fill in the lacunae in the existing literature, namely the absence of a summary global diagnostic accuracy and clinical utility parameter for use in India for non-English EPDS. Hence we: (1) Establish the summary global diagnostic accuracy of the non-English EPDS versions in India; and (2) Evaluate the clinical utility of the measure for post-natal Depression.
MATERIALS AND METHODS
Literature search
Two researchers (SMC and ER) independently electronically searched for relevant published studies in the PubMed, EMBASE (international database), MEDKNOW and IndMED (regional database) databases as well as hand-searched to augment the search with cross-references, published conference abstracts, Government of India publications, and grey literature from January 2000 to February 2018. We combined the search terms as follows: "diagnosis"[MeSH Terms] OR "diagnosis"[All Fields] OR "diagnostic"[All Fields]) AND accuracy[All Fields] AND ("psychiatric status rating scales"[MeSH Terms] OR ("psychiatric"[All Fields] AND "status"[All Fields] AND "rating"[All Fields] AND "scales"[All Fields]) OR "psychiatric status rating scales"[All Fields] OR ("Edinburgh"[All Fields] AND "postnatal"[All Fields] AND "depression"[All Fields] AND "scale"[All Fields]) OR "Edinburgh postnatal depression scale"[All Fields]) AND ("India"[MeSH Terms] OR "india"[All Fields].
Study selection and data extraction
Two other researchers (SR and SAV) extracted the required details independently, resolved any differences in extraction by consultation with another researcher (PSSR), and entered the information as electronic data. They extracted the participants, index measure, comparative reference measure and outcome of diagnostic accuracy details of each study. For a study to be included in the final analysis, it should have been conducted in India or among Indian populations, and must have compared the diagnostic accuracy of EPDS against either the Diagnostic and Statistical Manual (DSM) or International Classification of Diseases (ICD) for PND as the reference standard. Finally, each study had to report sufficient data to construct 2 × 2 tables for calculating the true positive, false positive, false negative and true negative values of EPDS against the reference standard.
Quality appraisal and risk of bias
Two researchers (SAV and PMM) also appraised the quality of the studies with Quality Assessment of Diagnostic-Accuracy Studies, version 2 (QUADAS-2)[9]. We calculated the Deek’s plot for publication bias[10].
Statistical analysis
We used the Area Under the Characteristic Curve of the Hierarchical Summary Receiver Operating Curve (HSAUROC), with random effects model, to establish the global diagnostic accuracy of EPDS[11]. This was the first outcome of this meta-analysis. Using the 2 × 2 table, we calculated the positive and negative likelihood ratios (+LR and –LR, respectively). From these likelihood ratios, we evaluated the post-test probabilities of EPDS using the Fagan’s nomogram (Bayesian approach); these post-test probabilities indicating the clinical utility was the second outcome of our study[12]. We calculated the 95% confidence interval (95%CI) whenever indicated. All analyses were done at the study level and not at the participant level. The analyses were done with STATA (version 15) using the MIDAS and METANDI modules.
RESULTS
Study characteristics
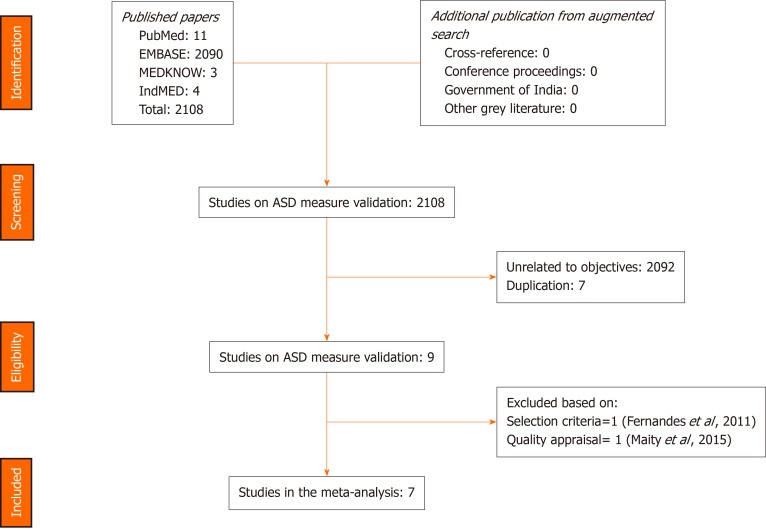
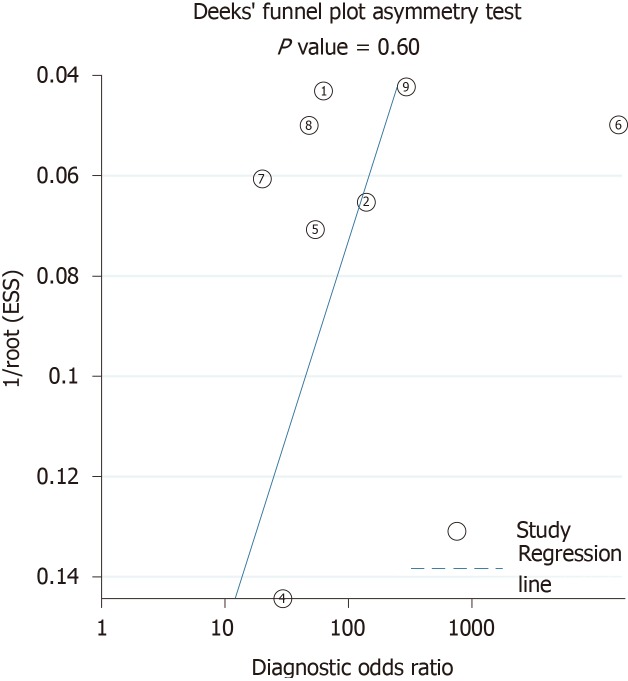
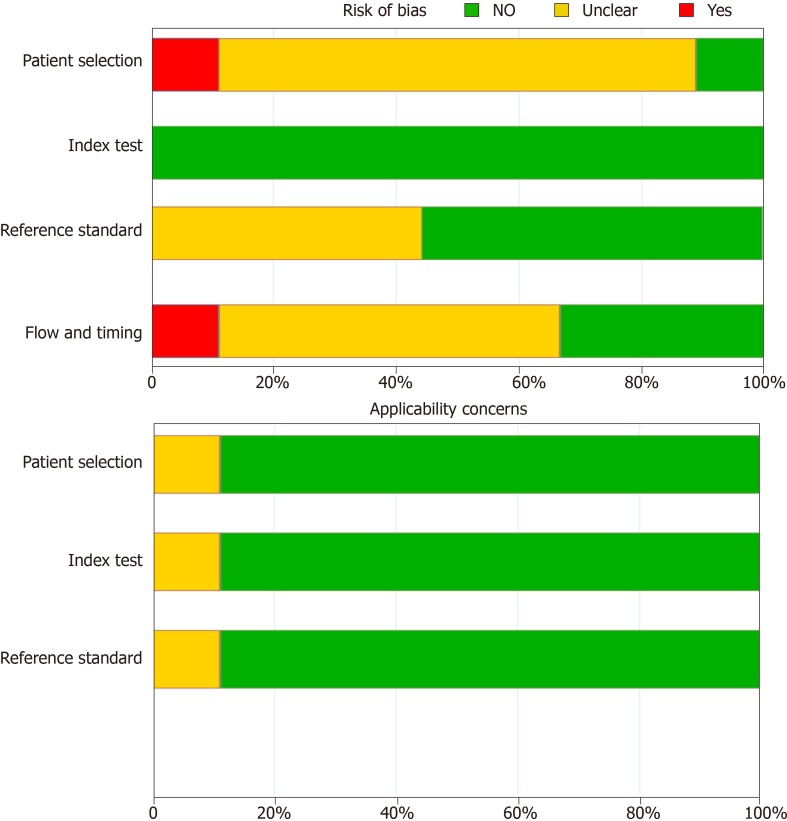
The search strategies provided 2108 titles and the diagnostic accuracy of EPDS was documented in nine studies in seven of the official languages of India[13-21]. One study in Kannada was excluded, as it included participants during their third trimester of pregnancy and not the post-natal period[16]. Another study in Bengali was excluded due to the poor quality of the study[20]. Figure 1 captures the PRISMA details, and Table 1 summarises the participants, index measure, comparative reference measure and outcome of diagnostic accuracy details and QUADAS -2 appraisal of each of the studies that were included or excluded in the final analysis (n = 1227). The QUADAS-2 appraisal demonstrated that in the risk of bias criteria, one study was rated as “at low risk of bias” across all domains. A rating of an unclear risk of bias was the most common rating across the appraisal domains. The Deek’s plot for publication bias is presented in Figure 2. In terms of applicability criteria, all seven studies were rated as applicable on all domains (Figure 3 for QUADAS-2 details). All studies had a cross-sectional design.
Figure 1.
Overview of PRISMA selection process of studies.
Figure 2.
The Deek’s plot for publication bias.
Figure 3.
The average Quality Assessment of Diagnostic-Accuracy Studies, version 2 appraisal for all included studies.
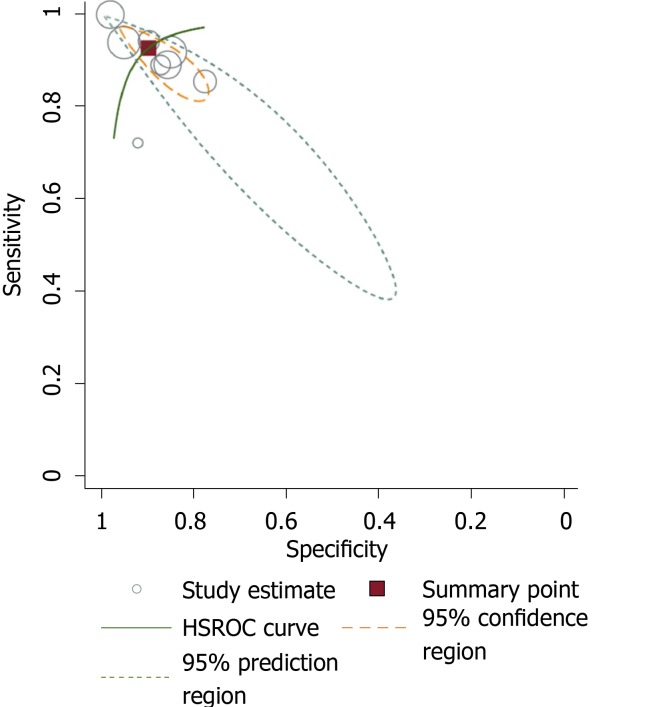
Diagnostic accuracy and clinical utility
The global diagnostic accuracy of EPDS as ascertained by HSAUROC was 0.97 (95%CI: 0.95-0.98) (Figure 4). The pre-test probability for the nomogram was 22%. For a +LR of 9, the positive post-test probability was 72% (95%CI: 68%, 76%) and for a -LR of 0.08, the negative post-test probability was 2% (95%CI: 1%, 3%) (Figure 5).
Figure 4.
The Hierarchical Summary Receiver Operating Characteristic Curve of Edinburgh Postnatal Depression Scale with its confidence and prediction contours. HSROC: Hierarchical Summary Receiver Operating Curve.
Figure 5.
The post-test probability of Edinburgh Postnatal Depression Scale calculated with Fagan’s nomogram.
DISCUSSION
Firstly, the global diagnostic accuracy of EPDS was excellent for the five different non-English versions in India. This HSAUROC value of 0.97 when converted to a more comprehensible clinical effect size of Cohen’s d or correlation coefficient r was 2.66 or 0.79, respectively[22]. This was a large effect size in the context of the diagnostic accuracy of EPDS when used as a screening measure for PND. Secondly, for the pre-test probability of 22%, the positive increment in diagnostic utility was 51% and the negative decrement was 20% for the post-test probability of EPDS. Given that the prevalence of PND in India is 22%[3], our incremental changes in post-test probability values have added considerable certainty to the diagnosis of PND when EPDS is used[12]. Thus, if a postnatal mother tests positive for EPDS, the chance she has PND increases from 22% to 72%; the clinician might therefore decide to actively engage in treatment. Conversely, if the patient tests negative, the chance of having PND decreases from 22% to 2%, and the clinician might decide not to actively treat the PND but engage instead in watchful waiting. Our finding about the diagnostic accuracy of EPDS versions is comparable with the values reviewed for the English versions in native English-speaking countries[6,7]. In comparison to some of the other selected non-English EPDS versions among African languages, the Chichewa version in Malawi, the Shona version in Zimbabwe, and the Nigerian version have relatively lower diagnostic accuracies than the summary value that is reported in this meta-analysis[23,24]. The translated version of EPDS in Afrikaans, Zulu, Tswana, Sotha, and Xhosa has demonstrated higher diagnostic accuracy for EPDS in South Africa[25]. Among European languages, the Danish version of EPDS has an Area Under the Curve of 0.96 and is comparable to our summary data[26], the Spanish version had an overall accuracy of 87.4%[27], and the French versions of EPDS has a sensitivity and specificity of 80% and 92%, and thus had lower diagnostic accuracy[28]. The other Asian language where EPDS has been validated includes Arabic[29], Chinese[30], and Japanese[31]; they have been found to have lower or similar diagnostic accuracies as in our meta-analysis.
The strengths of this study from a methodological perspective are that we followed the guidelines recommended by the Cochrane Diagnostic Test Accuracy Protocol. To present the summary of the global diagnostic accuracy of the EPDS, we used a summary line (HSROC) then summary point, as studies with various EPDS threshold values and two reference standards were analysed together. Furthermore, we anticipated the sensitivity as well as specificity of EPDS to differ widely between studies from the literature, and used the random effects model over the fixed effects model for analysis[6,7]. There was no publication or small study bias in our meta-analysis. Finally, from the policy implication standpoint, in about 69069 births expected per day in India[32], the need to identify the 22% of mothers with PND and deliver the integrated management of mother-baby dyad is a huge task. However, this can be achieved if PND is identified and EPDS is used as a valuable measure[33]. The National Mental Health Program should routinely incorporate the use of EPDS as the screening measure for PND in India through its District Mental Health approach.
In light of these findings, we conclude that the EPDS, with its many language versions and its brevity, is eminently suited for the screening of PND in India, where mental health resources are low but burden is high.
ARTICLE HIGHLIGHTS
Research background
Various language versions of Edinburgh Postnatal Depression (EPDS) have been validated in India. The summary global diagnostic accuracy and clinical utility of these versions was established.
Research motivation
The diagnosis of postnatal depression (PND) is often missed or misdiagnosed. This affects both the mother and the baby, with significant morbidity. The widely used EPDS in India has to be proven for the early identification of PND.
Research objectives
The aim of this meta-analysis was to document the summary diagnostic accuracy and clinical utility of the various language versions of EPDS in India.
Research methods
Seven studies were included in the analysis following the PRISMA guidelines. We used Area Under the Characteristic Curve of the Hierarchical Summary Receiver Operating Curve, with random effect model, to summarize the diagnostic accuracy of EPDS; Fagan’s nomogram was used for calculating clinical utility.
Research results
The global diagnostic accuracy of EPDS, as ascertained by Area Under the Characteristic Curve of the Hierarchical Summary Receiver Operating Curve, was 0.97 (95%CI: 0.95-0.98). For a PND prevalence of 22%, the positive post-test probability was 72% (95%CI: 68%, 76%) and the negative post-test probability was 2% (95%CI: 1%, 3%).
Research conclusions
We established the summary global diagnostic accuracy and clinical utility of the various versions of EPDS. The EPDS is effective in the early identification of PND.
Research perspectives
The EPDS in its various versions in India could be used for the scaling-up of PND treatment. The specific diagnostic parameters need to be further studied.
ACKNOWLEDGEMENTS
We acknowledge Professor Antonisamy B, Department of Biostatistics, Christian Medical College, Vellore for endorsing the data, analysis and conclusions of this study.
Footnotes
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
PRISMA 2009 Checklist statement: The authors prepared the research paper after reading the PRSIMA checklist 2009.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Peer-review started: December 26, 2019
First decision: February 19, 2020
Article in press: March 25, 2020
Specialty type: Psychiatry
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tu WJ S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Liu MY
Contributor Information
Paul Swamidhas Sudhakar Russell, Child and Adolescent Psychiatry Unit, Department of Psychiatry, Christian Medical College, Vellore 632 002, India.
Swetha Madhuri Chikkala, Child and Adolescent Psychiatry Unit, Department of Psychiatry, Christian Medical College, Vellore 632 002, India.
Richa Earnest, Child and Adolescent Psychiatry Unit, Department of Psychiatry, Christian Medical College, Vellore 632 002, India.
Shonima Aynipully Viswanathan, Child and Adolescent Psychiatry Unit, Department of Psychiatry, Christian Medical College, Vellore 632 002, India.
Sushila Russell, Child and Adolescent Psychiatry Unit, Department of Psychiatry, Christian Medical College, Vellore 632 002, India.
Priya Mary Mammen, Child and Adolescent Psychiatry Unit, Department of Psychiatry, Christian Medical College, Vellore 632 002, India.
References
- 1.The World Bank Group. World Bank Open Data: Free and Open access to global development data. 2018. [cited 3 April 2018] Available from: https://data.worldbank.org/?locations=IN-XN. html.
- 2.United Nations. World Population Prospects. 2017. Department of Economic and Social Affairs, Population Division. [cited 4 April 2018] Available from: https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_Wallchart.pdf.
- 3.Upadhyay RP, Chowdhury R, Aslyeh Salehi, Sarkar K, Singh SK, Sinha B, Pawar A, Rajalakshmi AK, Kumar A. Postpartum depression in India: a systematic review and meta-analysis. Bull World Health Organ. 2017;95:706–717C. doi: 10.2471/BLT.17.192237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen YH, Tsai SY, Lin HC. Increased mortality risk among offspring of mothers with postnatal depression: a nationwide population-based study in Taiwan. Psychol Med. 2011;41:2287–2296. doi: 10.1017/S0033291711000584. [DOI] [PubMed] [Google Scholar]
- 5.Parsons CE, Young KS, Rochat TJ, Kringelbach ML, Stein A. Postnatal depression and its effects on child development: a review of evidence from low- and middle-income countries. Br Med Bull. 2012;101:57–79. doi: 10.1093/bmb/ldr047. [DOI] [PubMed] [Google Scholar]
- 6.Eberhard-Gran M, Eskild A, Tambs K, Opjordsmoen S, Samuelsen SO. Review of validation studies of the Edinburgh Postnatal Depression Scale. Acta Psychiatr Scand. 2001;104:243–249. doi: 10.1034/j.1600-0447.2001.00187.x. [DOI] [PubMed] [Google Scholar]
- 7.Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119:350–364. doi: 10.1111/j.1600-0447.2009.01363.x. [DOI] [PubMed] [Google Scholar]
- 8.Leung SS, Leung C, Lam TH, Hung SF, Chan R, Yeung T, Miao M, Cheng S, Leung SH, Lau A, Lee DT. Outcome of a postnatal depression screening programme using the Edinburgh Postnatal Depression Scale: a randomized controlled trial. J Public Health (Oxf) 2011;33:292–301. doi: 10.1093/pubmed/fdq075. [DOI] [PubMed] [Google Scholar]
- 9.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 10.Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–893. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 11.Takwoingi Y, Guo B, Riley RD, Deeks JJ. Performance of methods for meta-analysis of diagnostic test accuracy with few studies or sparse data. Stat Methods Med Res. 2017;26:1896–1911. doi: 10.1177/0962280215592269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caraguel CG, Vanderstichel R. The two-step Fagan's nomogram: ad hoc interpretation of a diagnostic test result without calculation. Evid Based Med. 2013;18:125–128. doi: 10.1136/eb-2013-101243. [DOI] [PubMed] [Google Scholar]
- 13.Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: a study of mothers in Goa, India. Am J Psychiatry. 2002;159:43–47. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 14.Benjamin D, Chandramohan A, Annie IK, Prasad J, Jacob KS. Validation of the Tamil version of Edinburgh post-partum depression scale. J Obstet Gynecol India. 2005;55:241–243. [Google Scholar]
- 15.Werrett J, Clifford C. Validation of the Punjabi version of the Edinburgh postnatal depression scale (EPDS) Int J Nurs Stud. 2006;43:227–236. doi: 10.1016/j.ijnurstu.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Fernandes MC, Srinivasan K, Stein AL, Menezes G, Sumithra R, Ramchandani PG. Assessing prenatal depression in the rural developing world: a comparison of two screening measures. Arch Womens Ment Health. 2011;14:209–216. doi: 10.1007/s00737-010-0190-2. [DOI] [PubMed] [Google Scholar]
- 17.Desai N, Mehta R, Ganjiwale J. Validation of Gujarati version of Edinburg post natal depression scale among women within their first post partum year. Indian J Soc Psychiatry. 2011;27:16–23. [Google Scholar]
- 18.Savarimuthu RJ, Ezhilarasu P, Charles H, Balavendra A, Jacob KS. Validating the Tamil Version of the Edinburgh Postpartum Depression Scale in South Indian Setting. Indian J Cont Nsg Edn. 2012;13:27–32. [Google Scholar]
- 19.Kalita KN, Phookun HR, Das GC. A clinical study of postpartum depression: validation of the Edinburgh postnatal depression scale (Assamese version) Eastern J Psychiatry. 2014;11:14–18. [Google Scholar]
- 20.Maity C, Saha S, Sanyal D, Biswas A. The Bengali Adaptation of Edinburgh Postnatal Depression Scale. IOSR-JNHS. 2015;4:12–16. [Google Scholar]
- 21.Khapre M, Dhande N, Mudey A. Validity and Reliability of Marathi Version of Edinburgh Postnatal Depression Scale as a Screening Tool for Post Natal Depression. Natl J Community Med. 2017;8:116–121. [Google Scholar]
- 22.Rice ME, Harris GT. Comparing effect sizes in follow-up studies: ROC Area, Cohen's d, and r. Law Hum Behav. 2005;29:615–620. doi: 10.1007/s10979-005-6832-7. [DOI] [PubMed] [Google Scholar]
- 23.India Population, 2018. World Population Review. [cited 3 October 2018] Available from: http://worldpopulationreview.com/countries/india-population/
- 24.Stewart RC, Umar E, Tomenson B, Creed F. Validation of screening tools for antenatal depression in Malawi--a comparison of the Edinburgh Postnatal Depression Scale and Self Reporting Questionnaire. J Affect Disord. 2013;150:1041–1047. doi: 10.1016/j.jad.2013.05.036. [DOI] [PubMed] [Google Scholar]
- 25.Chibanda D, Mangezi W, Tshimanga M, Woelk G, Rusakaniko P, Stranix-Chibanda L, Midzi S, Maldonado Y, Shetty AK. Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Arch Womens Ment Health. 2010;13:201–206. doi: 10.1007/s00737-009-0073-6. [DOI] [PubMed] [Google Scholar]
- 26.Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. S Afr Med J. 1998;88:1340–1344. [PubMed] [Google Scholar]
- 27.Smith-Nielsen J, Matthey S, Lange T, Væver MS. Validation of the Edinburgh Postnatal Depression Scale against both DSM-5 and ICD-10 diagnostic criteria for depression. BMC Psychiatry. 2018;18:393. doi: 10.1186/s12888-018-1965-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alvarado R, Jadresic E, Guajardo V, Rojas G. First validation of a Spanish-translated version of the Edinburgh postnatal depression scale (EPDS) for use in pregnant women. A Chilean study. Arch Womens Ment Health. 2015;18:607–612. doi: 10.1007/s00737-014-0466-z. [DOI] [PubMed] [Google Scholar]
- 29.Guedeney N, Fermanian J. Validation study of the French version of the Edinburgh Postnatal Depression Scale (EPDS): new results about use and psychometric properties. Eur Psychiatry. 1998;13:83–89. doi: 10.1016/S0924-9338(98)80023-0. [DOI] [PubMed] [Google Scholar]
- 30.Ghubash R, Abou-Saleh MT, Daradkeh TK. The validity of the Arabic Edinburgh Postnatal Depression Scale. Soc Psychiatry Psychiatr Epidemiol. 1997;32:474–476. doi: 10.1007/BF00789142. [DOI] [PubMed] [Google Scholar]
- 31.Lee DT, Yip SK, Chiu HF, Leung TY, Chan KP, Chau IO, Leung HC, Chung TK. Detecting postnatal depression in Chinese women. Validation of the Chinese version of the Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1998;172:433–437. doi: 10.1192/bjp.172.5.433. [DOI] [PubMed] [Google Scholar]
- 32.Sasaki Y, Baba T, Oyama R, Fukumoto K, Haba G, Sasaki M. Re-evaluation of the Edinburgh Postnatal Depression Scale as screening for post-partum depression in Iwate Prefecture, Japan. J Obstet Gynaecol Res. 2019;45:1876–1883. doi: 10.1111/jog.14042. [DOI] [PubMed] [Google Scholar]
- 33.Stein A, Netsi E, Lawrence PJ, Granger C, Kempton C, Craske MG, Nickless A, Mollison J, Stewart DA, Rapa E, West V, Scerif G, Cooper PJ, Murray L. Mitigating the effect of persistent postnatal depression on child outcomes through an intervention to treat depression and improve parenting: a randomised controlled trial. Lancet Psychiatry. 2018;5:134–144. doi: 10.1016/S2215-0366(18)30006-3. [DOI] [PubMed] [Google Scholar]