Introduction
The broad differential diagnosis of scalp nodules includes pilar cyst, cylindroma, primary cutaneous malignancy, melanoma, Merkel cell carcinoma, angiosarcoma, and metastatic carcinoma. The most common cutaneous malignancies of the scalp are basal cell carcinoma and squamous cell carcinoma, in which less than 10% of cases represent metastatic disease.1 The most common cutaneous metastases to manifest in the scalp are the same as those that metastasize to the skin, such as melanoma, and visceral malignancies of the breast, lung, and colon.1 However, there are reports of other gastrointestinal cancers that metastasize to the scalp.
Distant cutaneous metastasis from cholangiocarcinoma is a rare phenomenon with approximately 30 reported cases in the literature. Cholangiocarcinoma itself is a rare malignancy with an aggressive course and poor prognosis that accounts for 3% of gastrointestinal tract cancers. Hepatitis C virus (HCV) is a known risk factor for cholangiocarcinoma and, in particular, intrahepatic cholangiocarcinoma.2 Here we describe a case, different from those reviewed by Liu et al,3 of cutaneous scalp metastasis as a first presentation of cholangiocarcinoma in a patient with known HCV.3
Case presentation
A 75-year-old Middle Eastern woman with a history of HCV presented with a growing pruritic scalp lesion present for 1 month in addition to altered mental status, decreased oral intake, nausea, vomiting, back pain, subjective weight loss, and fatigue worsening over 6 weeks. Physical examination found a 4-cm indurated pink nodular plaque with hemorrhagic crust on the mid frontal scalp (Fig 1) and 2 smaller satellite 6-mm pink papules on the posterior border. Her HCV viral load was 48,900 IU/mL; calcium level, 12.9 mg/dL; serum aspartate transaminase, 85U/L; alanine aminotransferase, 261 U/L; alkaline phosphatase, 303 U/L; total bilirubin, 6.2 mg/dL; direct bilirubin, 5.1 mg/dL; and ammonia, 14 μmol/L. An abdominal ultrasound scan was significant for a surgically absent gallbladder and multiple hypodense lesions in the liver concerning for metastases versus regenerative nodules secondary to cirrhosis. At presentation, there was no known primary malignancy. A 4-mm punch biopsy section (Fig 2, A) showed a dense infiltrate of poorly differentiated carcinoma entirely replacing the dermis, leaving the epidermis intact. On higher magnification (Fig 2, B) the tumor cells were attempting to re-form glandular structures consistent with adenocarcinoma. Immunohistochemistry findings were significant for tumor cells, strongly (3+) and uniformly expressing CK-7 antigen (Fig 3, A) and negative for CK-20 antigen (Fig 3, B). Additional immunohistochemistry findings were negative for estrogen receptor antigen (0+), progesterone receptor antigen (0+), and HER-2/neu antigen (0+) making metastatic breast cancer less likely. The immunophenotypic differential diagnosis suggested the primary malignancy arose from the liver, bile duct system, and pancreas.
Fig 1.

Initial scalp lesion as a 4-cm indurated pink nodular plaque with a crusted cap on the mid frontal scalp with 2 smaller satellite 6-mm pink papules.
Fig 2.
A, Dermis replaced by an infiltrative poorly differentiated carcinoma with an unremarkable epidermis consistent with metastasis. B, Tumor cells attempting to re-form glandular structures consistent with adenocarcinoma. (A and B, Hematoxylin-eosin stain; original magnifications: A, ×4; B, ×20.)
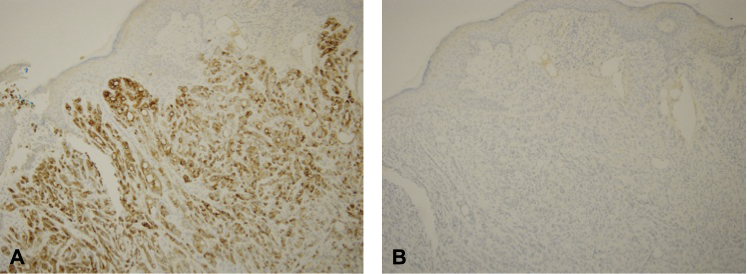
Fig 3.
A, Immunohistochemical stain. Tumor cells strongly (3+) and uniformly expressing CK-7 antigen. B, Immunohistochemical stain. Tumor cells negative (0+) expressing CK-20 antigen.
On additional clinical workup, CA 19-9 and CEA were elevated (15021.71 U/L and 8.74 ng/mL, respectively), with a normal α-fetoprotein (AFP) level (4.7 ng/mL). Computerized tomography with and without contrast of the chest and abdomen/pelvis found no pancreatic mass, no colorectal abnormalities, and multiple liver and lung metastatic lesions. These clinical, laboratory, and imaging findings were most consistent with metastatic cholangiocarcinoma.
Discussion
Hepatitis C is a known risk factor for hepatocellular carcinoma (HCC). Therefore, metastatic HCC was initially higher on the differential diagnosis for this patient. However, a normal AFP level and elevated CEA and CA 19-9 made this diagnosis less likely. Considering other diagnoses, HCV also increases the risk for cholangiocarcinoma, in particular, intrahepatic cholangiocarcinoma.2, 3, 4 Because the patient's gallbladder had been removed and there was no evidence of an obstructive tumor in the extrahepatic bile ducts on imaging, a feature more consistent with extrahepatic cholangiocarcinoma, her scalp metastasis and tumor markers were essential to the final diagnosis.5
Similar to a case presented by Hyun et al,6 immunohistochemical staining of a skin biopsy was necessary for diagnosis given the nonspecific and varying histopathologic features of metastatic cholangiocarcinoma that range from a well-differentiated adenocarcinoma with mucin production to a poorly differentiated carcinoma with evidence of reforming tubular and glandular structures. In this case, immunohistochemical staining for breast cancer markers was negative, and positive CK-7 and negative CK-20 were more consistent with a malignancy of hepatic or biliopancreatic origin. Given these staining results, in conjunction with the elevated CA 19-9, CEA, normal AFP, and normal ammonia, the most likely diagnosis was cholangiocarcinoma, rather than metastatic HCC.
Liu et al3 conducted a meta-analysis of 30 cases describing cutaneous metastases of primary cholangiocarcinoma that varied in clinical presentation and site location. Lesions presented as nodules, papules, and erythema with and without ulceration, and nodular presentation was more common on the scalp. Of the 30 patients described in the literature, 50% of cutaneous metastases were at the site of the catheter or percutaneous biliary drainage. However, the most common site of distant metastasis was the scalp (36.7%). In addition, cutaneous metastasis was the primary sign of the underlying malignancy in 26.7% of patients. However, this study did not mention any patients that had underlying HCV, a disease known to increase the risk of primary cholangiocarcinoma and as presented in this case.
This case highlights that although the most common scalp metastases are of breast, lung, and colorectal origin, primary cholangiocarcinoma should remain in the differential diagnosis. As in this case, clinicopathologic correlation with computed tomography imaging, liver enzymes, and gastrointestinal tumor markers is paramount given that the histopathologic and immunohistochemical characteristics of metastatic cholangiocarcinoma are nonspecific. Therefore, in a patient with metastatic disease with an unknown primary malignancy, primary cholangiocarcinoma should be considered in the differential diagnosis for patients with new scalp lesions with a history of HCV.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Richmond H.M., Duvic M., Macfarlane D.F. Primary and metastatic malignant tumors of the scalp: an update. Am J Clin Dermatol. 2010;11(4):233–246. doi: 10.2165/11533260-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 2.Li H., Hu B., Zhou Z.Q., Guan J., Zhang Z.Y., Zhou G.W. Hepatitis C virus infection and the risk of intrahepatic cholangiocarcinoma and extrahepatic cholangiocarcinoma: evidence from a systematic review and meta-analysis of 16 case-control studies. World J Surg Oncol. 2015;13:161. doi: 10.1186/s12957-015-0583-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu M., Liu B.L., Liu B. Cutaneous metastasis of cholangiocarcinoma. World J Gastroenterol. 2015;21(10):3066–3071. doi: 10.3748/wjg.v21.i10.3066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dogan G., Karincaoglu Y., Karincaoglu M., Aydin N.E. Scalp ulcer as first sign of cholangiocarcinoma. Am J Clin Dermatol. 2006;7(6):387–389. doi: 10.2165/00128071-200607060-00008. [DOI] [PubMed] [Google Scholar]
- 5.Saha S.K., Zhu A.X., Fuchs C.S., Brooks G.A. Forty-Year Trends in Cholangiocarcinoma Incidence in the U.S.: intrahepatic disease on the rise. Oncologist. 2016;21(5):594–599. doi: 10.1634/theoncologist.2015-0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyun S.Y., Lee J.H., Shin H.S., Lee S.W., Park Y.N., Park J.Y. Cutaneous metastasis from cholangiocarcinoma as the first clinical sign: a report of two cases. Gut Liver. 2011;5(1):100–104. doi: 10.5009/gnl.2011.5.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]