Abstract
Public health crises, such as the outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) since Dec. 2019, are widely acknowledged as severe traumatic events that impose threats not only because of physical concerns but also because of the psychological distress of infected patients. We designed an internet-based integrated intervention and evaluated its efficacy on depression and anxiety symptoms in patients infected by SARS-CoV-2.
Keywords: Coronavirus disease 2019 (COVID-19), Internet-based integrated intervention, Depression, Anxiety
Public health crises, such as the outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) since Dec. 2019, are widely acknowledged as severe traumatic events that impose threats not only because of physical concerns but also because of the psychological distress of infected patients. We designed an internet-based integrated intervention and evaluated its efficacy on depression and anxiety symptoms in patients infected by SARS-CoV-2.
Wuhan, the capital city of Hubei Province, China, has attracted global attention because of the outbreak of SARS-CoV-2-infected pneumonia (coronavirus disease 2019 (COVID-19)). On Jan. 3, 2020, the SARS-CoV-2 was isolated in samples of broncho-alveolar lavage fluid from a patient in Wuhan and was confirmed as the cause of the novel CoV-infected pneumonia (Zhu et al., 2020). On Jan. 20, 2020, Chinese experts confirmed human-to-human transmission of SARS-CoV-2 and infection of medical staff. Three days after that, the Chinese government locked down Wuhan in an unprecedented effort to curb the spread of SARS-CoV-2 (Xinhua Net, 2020). The SARS-CoV-2 infection has been reported not only in China, but also in other countries. As of Mar. 12, 2020, the number of confirmed cases of the novel CoV approached 128 000 with a total of 4713 reported deaths in at least 118 countries.
In the fight against the SARS-CoV-2, COVID-19 patients have been experiencing enormous psychological pressure, specifically including a lack of knowledge about the consequences of infection by a potentially fatal new virus, isolation, and feelings of helplessness. These situations are giving rise to mental health problems, such as stress, anxiety, depressive symptoms, insomnia, and fear in patients with confirmed SARS-CoV-2. Moreover, symptoms of the infection, such as fever, fatigue, and dyspnea, as well as the side effects of treatments, could result in worsening mental distress (Xiang et al., 2020). Consistently, in the early stage of the SARS outbreak, the emergency of which had parallels with the COVID-19 epidemic, a range of psychiatric conditions, including high levels of stress, depressive symptoms, anxiety, insomnia, nightmares, and poor concentration, were reported by SARS patients (Chua et al., 2004). Further evidence suggested that these psychiatric morbidities might be still significant even when persons infected with SARS recovered physically (Tsang et al., 2004), and SARS survivors who had a history of psychiatric consultation in the acute phase of the illness had a higher risk for psychological distress later, after discharge from the hospital, and might warrant timely and focused mental health support services (Wu et al., 2005).
Although data from systematic studies of SARS-CoV-2 do not yet exist, evidence suggests that this disease has psychosocial consequences for COVID-19 patients (Duan and Zhu, 2020). The psychological impacts of SARS-CoV-2 should not be overlooked. However, evidence-based interventions targeted at COVID-19 patients are scarce. Thus, the aims of the present study are to introduce an internet-based integrated intervention to COVID-19 patients with psychological distress and to evaluate the efficacy of the provided mental health care on depression and anxiety symptoms in patients with COVID-19.
This is a prospective, randomized, controlled, 2-week study conducted in the First Affiliated Hospital, School of Medicine, Zhejiang University (Hangzhou, China) from Feb. 2 to Feb. 28, 2020. All the laboratory-confirmed COVID-19 patients in the isolation ward were screened by Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001) and Generalized Anxiety Disorder-7 (GAD-7) (Spitzer et al., 2006) for psychological distress and finally, a total of 26 COVID-19 patients were enrolled in this study. The inclusion criteria were as follows: (1) aged 18–65 years; (2) PHQ-9 or GAD-7 of ≥5; (3) completed at least a junior middle school level of education. Any participant who met one of the following criteria was excluded: (1) PHQ-9 or GAD-7 of ≥15; (2) with suicidal ideation; (3) use of any antipsychotics; (4) the underlying disease was too severe to complete the assessments; (5) unable to follow the instructions of the internet-based intervention. A list of random sequence assignments for each group was drawn up by computer at the beginning of the study. After recruitment, 26 participants were randomly assigned to groups sequentially, with an equal probability of receiving an internet-based integrated intervention (intervention group) or just supportive care (control group), with 13 participants in each group. The 17-item Hamilton Depression Scale (17-HAMD) (Hamilton, 1967) and Hamilton Anxiety Scale (HAMA) (Hamilton, 1959) were used to assess the severity of depression and anxiety symptoms, respectively, and the efficacy of the internet-based integrated intervention every week. The outcomes of psychological assessments were analyzed by repeated measures analyses of variance with time as the within-subjects factor and group as the between-subjects factor. Last observation carried forward (LOCF) analysis was performed only in patients who dropped out and failed to complete two-week intervention.
The internet-based integrated intervention is a self-help intervention containing four main components: breath relaxation training, mindfulness (body scan), “refuge” skills, and butterfly hug method. The instructions for this internet-based integrated intervention were audio-recorded and then put online. All subjects in the intervention group were guided to listen to the audio via their mobile phones and follow the instructions for intervention training at a fixed time every day for two weeks. It would take the patient about 50 min to finish this everyday task. In addition, during the study period, the participants in the control group received daily supportive care only.
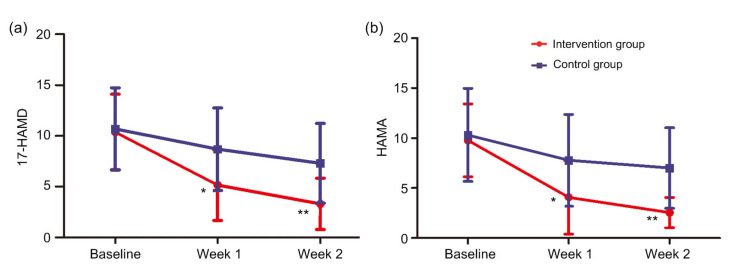
As indicated in Table 1, nine (34.6%) of the 26 patients had underlying diseases: four (15.4%) had hypertension, two (7.7%) had liver disease, and one (3.8%) each had gastric ulcer, coronary heart disease (CHD), and acquired immune deficiency syndrome (AIDS). No significant difference between the two groups was observed for age, gender, severity of illness, baseline scores of PHQ-9, GAD-7, 17-HAMD, or HAMA. Three patients in the intervention group and one patient in the control group failed to complete the assessments at the end of the second week because of discharge from hospital. Overall, there was a significant time effect indicating reduction in mean scores of 17-HAMD (F=37.35, P<0.001) and HAMA (F=26.58, P<0.001), as well as a main effect of group (17-HAMD: F=4.384, P=0.047; HAMA: F=5.634, P=0.026) and a group-by-time interaction (17-HAMD: F=5.268, P=0.009; HAMA: F=3.743, P=0.031). There were no main or interactive effects of age, gender, or severity of illness on scores of 17-HAMD and HAMA when introduced as covariates in the analyses. Post hoc analyses of the individual time points showed that scores of 17-HAMD and HAMA were significantly decreased in patients of the intervention group at the end of the first (17-HAMD, t=−2.381, P=0.026; HAMA, t=−2.263, P=0.033) and second (17-HAMD, t=−3.089, P=0.005; HAMA, t=−3.746, P=0.001) weeks, when compared with the patients of the control group (Fig. 1).
Table 1.
Demographic and clinical characteristics of all subjects (n=26)
| Characteristics | Intervention group (n=13) | Control group (n=13) | t/χ2 | P-value |
| Age (year) | 40.8±13.5 | 48.5±9.5 | t=−1.693 | 0.103 |
| Gender (male/female) | 9/4 | 7/6 | χ2=0.650 | 0.420 |
| Severity of illness | ||||
| Medium | 5 (38.5) | 4 (30.8) | ||
| Severe | 8 (61.5) | 9 (69.2) | χ2=0.170 | 0.680 |
| Coexisting conditions | ||||
| Any | 5 (38.5) | 4 (30.8) | ||
| Hypertension | 3 (23.1) | 1 (7.7) | ||
| Live disease | 1 (7.7) | 1 (7.7) | ||
| Gastric ulcer | 0 (0.0) | 1 (7.7) | ||
| CHD | 1 (7.7) | 0 (0.0) | ||
| AIDS | 0 (0.0) | 1 (7.7) | ||
| PHQ-9 score | 7.08±2.25 | 7.76±2.89 | t=−0.681 | 0.502 |
| GAD-7 score | 5.08±2.75 | 5.92±2.53 | t=−0.816 | 0.423 |
| PHQ-9 score≥5 | 12 (92.3) | 12 (92.3) | χ2=0.000 | 1.000 |
| GAD-7 score≥5 | 6 (46.2) | 10 (76.9) | χ2=2.600 | 0.107 |
Data were expressed as number, number (percentage), or mean±standard deviation (SD). CHD: coronary heart disease; AIDS: acquired immune deficiency syndrome; PHQ-9: Patient Health Questionnaire-9; GAD-7: Generalized Anxiety Disorder-7
Fig. 1.
Changes in scores of 17-HAMD and HAMA across the experimental groups
(a) Significant decreases of scores of 17-HAMD were observed in patients of the intervention group at the end of the first (t=−2.381, P=0.026) and second (t=−3.089, P=0.005) weeks when compared with the patients of the control group since recruitment. (b) Consistent with scores of 17-HAMD, as compared with the controls, patients of the intervention group showed decreased scores of HAMA with statistical significance at the end of the first (t=−2.263, P=0.033) and second (t=−3.746, P=0.001) weeks since recruitment. 17-HAMD, 17-item Hamilton Depression Scale; HAMA, Hamilton Anxiety Scale. * P<0.05, ** P<0.01, compared with the control group (n=13). Data are expressed as mean±standard deviation (SD)
In this study, we designed an internet-based integrated intervention focusing on relaxation, self-care, and raising the sense of security. To the best of our knowledge, it is the first time that the efficacy of this internet-based self-help intervention has been evaluated for COVID-19 patients with psychological distress. We found that patients of the intervention group exhibited significantly decreased levels of depression and anxiety symptoms in comparison with those of the control group, indicating that our internet-based integrated intervention showed a rapid improvement on mood disturbance and it should be applied in the management of psychological distress in COVID-19 patients.
To date, the popularity of internet services and smartphones has enabled mental health professionals and health authorities to provide online mental health services (Liu et al., 2020). It has been demonstrated in a previous meta-analysis that internet-delivered cognitive behavior therapy (ICBT) was as effective as face-to-face treatment for depressive symptoms, social anxiety disorder, and other psychological or somatic disorders (Andersson et al., 2014). In this context, internet-based interventions increasingly complement face-to-face counseling or therapy. Furthermore, internet-based interventions also showed advantages over face-to-face therapy, and the benefits mainly included low threshold accessibility, flexible use, independence of time and place, use at a self-determined pace, a high level of autonomy and privacy, and lower costs (Schröder et al., 2016). These factors might be especially relevant for COVID-19 patients since the human-to-human transmission of SARS-CoV-2 was confirmed and the infected patients were in quarantine. Internet-based intervention could also diminish the risk of infection in mental healthcare providers.
Consistent with our findings, prior evidence has been found for the benefit of internet-based intervention programs on mental health, particularly for depression, stress and distress, and anxiety. The types of interventions that predominated as efficacious included information and education with or without professional psychological support, and, to a lesser extent, combined with peer and psychological support (Sherifali et al., 2018). Nevertheless, in an internet-based intervention comprising five structured confrontational writing assignments, for individuals who experienced the death of a first-degree relative and who were significantly distressed, although writing decreased feelings of emotional loneliness and increased positive mood, writing did not affect grief or depressive symptoms. One possible explanation for the unexpected outcome might be related to the fact that the participants who entered the study were on average quite distressed (van der Houwen et al., 2010). In our study, only patients with mild to moderate depression or anxiety symptoms were recruited, and the results were in accord with our initial expectation. Taken together, the current findings provided information that individuals with mild to moderate psychological distress might be more suitable for internet-based intervention.
The results of the present study should be interpreted in the light of several limitations. First, the sample size of each group was relatively small, which limited its statistical power to detect real effects. Secondly, this study might have a risk of bias for blinding of outcome assessments, because the evaluation was also performed by the intervention provider. Thirdly, the study period of two weeks was relatively short for efficacy assessment, and follow-up measures that might confirm the stability of the current effects were not included in this study. Taken together, findings of the present study need to be confirmed in further studies that overcome those limitations.
In conclusion, the present study provided an internet-based integrated intervention focusing on relaxation, self-care, and raising sense of security for COVID-19 patients with psychological distress. The preliminary results of this study demonstrated a pleasing effect of the internet-based integrated intervention on mild to moderate depression and anxiety symptoms.
Footnotes
Project supported by the Science and Technology Department of Zhejiang Province (No. 2017C37037), the National Key Research and Development Program of China (Nos. 2016YFC1307100 and 2018YFC1314200), the Zhejiang Provincial Natural Science Foundation of China (Nos. LQ20H090012 and LQ20H090010), and the Zhejiang University Special Scientific Research Fund for COVID-19 Prevention and Control (No. 2020XGZX046), China
Contributors: Ning WEI conducted the intervention and collected the clinical data. Bo-chao HUANG designed the integrated intervention. Shao-jia LU wrote the first draft of the manuscript. Jian-bo HU, Chan-chan HU, Jing-kai CHEN, and Jin-wen HUANG designed and completed the audio records. Xiao-yi ZHOU, Shu-guang LI, Zheng WANG, and Dan-dan WANG performed the statistics and analyses of the data. Yi XU and Shao-hua HU designed the study. All authors have read and approved the final manuscript, and therefore, have full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Compliance with ethics guidelines: Ning WEI, Bo-chao HUANG, Shao-jia LU, Jian-bo HU, Xiao-yi ZHOU, Chan-chan HU, Jing-kai CHEN, Jin-wen HUANG, Shu-guang LI, Zheng WANG, Dan-dan WANG, Yi XU, and Shao-hua HU declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
References
- 1.Andersson G, Cuijpers P, Carlbring P, et al. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014;13(3):288–295. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chua SE, Cheung V, McAlonan GM, et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry. 2004;49(6):385–390. doi: 10.1177/070674370404900607. [DOI] [PubMed] [Google Scholar]
- 3.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry, online. 2020 doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 5.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 6.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu S, Yang LL, Zhang CX, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry, online. 2020 doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schröder J, Berger T, Westermann S, et al. Internet interventions for depression: new developments. Dialogues Clin Neurosci. 2016;18(2):203–212. doi: 10.31887/DCNS.2016.18.2/jschroeder. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sherifali D, Ali MU, Ploeg J, et al. Impact of internet-based interventions on caregiver mental health: systematic review and meta-analysis. J Med Internet Res. 2018;20(7):e10668. doi: 10.2196/10668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 11.Tsang HWH, Scudds RJ, Chan EYL. Psychosocial impact of SARS. Emerg Infect Dis. 2004;10(7):1326–1327. doi: 10.3201/eid1007.040090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van der Houwen K, Schut H, van den Bout J, et al. The efficacy of a brief internet-based self-help intervention for the bereaved. Behav Res Ther. 2010;48(5):359–367. doi: 10.1016/j.brat.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerg Infect Dis. 2005;11(8):1297–1300. doi: 10.3201/eid1108.041083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xinhua Net. Xinhua Headlines: a race against time!. Wuhan battles coronavirus. http://www.xinhuanet.com/english/2020-01/30/c_138743900.htm [Accessed on Mar. 12, 2020].2020. [Google Scholar]
- 16.Zhu N, Zhang DY, Wang WL, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(2):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]