We appreciate the valuable comments to our article[1] by Professor Olson and his team. The comments reflect a considerable knowledge of intracranial pressure (ICP) measurement and management and a deep appreciation of the challenges to obtaining accurate ICP values in the clinical setting – a deceptively simple task. We humbly offer the following reply:
We acknowledge that 34 recordings from six patients is a small sample size of subjects. The study is intended as a pilot study needing validation in larger sample sizes for the reasons provided by Olson et al. However, the study size is deceptive, since there are over 4200 data points, and high resolution time frequency data, with waveform analysis applied to the data set. Hence, the relatively short duration and small number of subjects offers high data quality that would likely degrade with longer duration sampling and larger numbers of subjects. Hence, there is a trade-off between quality for quantity.
We acknowledge that our conclusion ‘there is concordance between ICPf and ICPe’ is only demonstrated when the external ventricular drain (EVD) is clamped (i.e. cerebral spinal fluid [CSF] drainage is not occurring). Validating ICPf during periods of drainage by direct comparison with another ICP waveform would require placement of an additional ICP monitor into the brain[2-5], which would increase patient risk. While we do not validate ICPf during CSF drainage in this study per se, we think that ICPf when measured during periods of drainage does provide clinically useful data. While there may be a theoretical difference in the function of the sensor during periods of drainage, the CSF flow rate is low and CSF turbulence is unlikely to significantly affect the performance of the sensor. Additionally, the contour of the ICPf waveform does not abruptly change at the onset of drainage suggesting the sensor continues to provide useful information.
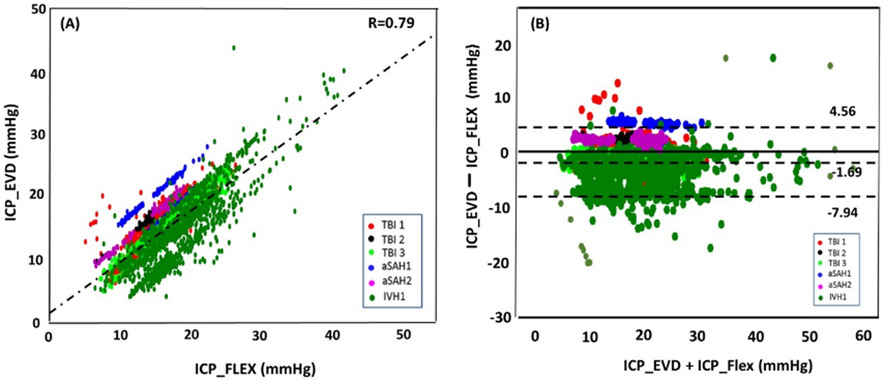
We agree that the difference between mean ICP from the two sources is not statistically different – in our study a mean difference of −1.69 mmHg was registered and the measurements from one source crossing the important threshold of 20 mmHg are not necessarily in agreement with measurements from another sources. To be able to accurately pinpoint the source(s) of this differences would be impossible without ensuring measurement from both sources were done after zeroing the sensors properly and according to the same reference point. Therefore, in future studies, a more rigorous control and execution of the ICP sensor zeroing will be needed.
Thank you very much for the good suggestion about re-creating Fig 3 using the technique used in Fig 5. We re-plotted Figure 3 accordingly and the data points were divided into three clusters as shown below. Traumatic brain injury (TBI) patients’ data concentrate around the regression line (red, black and light green points, Fig 3A), while the aSAH patients’ data and IVH patients’ data distributed in the two sides of the regression line. However, this observation will need to be interpreted with extreme caution due to the small number of subjects with each diagnosis. However, we do think this observation deserves further exploration in larger data sets, if available in the future.
Fig. 3.
A) A scatter plot between mean ICP from the conventional EVD (x-axis, ICPe) and from FLEX sensor at the tip (y-axis, ICPf) (n=4273). A significant linear correlation was found between the two ICPs. B) Bland–Altman plot between the two ICP measurements indicates that mean difference between the two ICPs is only −1.96 mmHg. 95% confidence interval of agreement is −7.94 to 4.56 mmHg. ICP intracranial pressure, EVD external ventricular drains. Each color represents one patient.
References
- 1.Liu X, Zimmermann LL, Ho N, Vespa P, Liao X, Hu X. Evaluation of a New Catheter for Simultaneous Intracranial Pressure Monitoring and Cerebral Spinal Fluid Drainage: A Pilot Study. Neurocrit Care [Internet]. 2018; Available from: 10.1007/s12028-018-0648-z [DOI] [PMC free article] [PubMed]
- 2.Helbok R, Olson DW, Le Roux P, Vespa P, Menon DK, Vespa P, et al. Intracranial Pressure and Cerebral Perfusion Pressure Monitoring in Non-TBI Patients: Special Considerations. Neurocrit Care. 2014; [DOI] [PubMed]
- 3.Mahdavi ZK, Olson DM, Figueroa SA. Association Patterns of Simultaneous Intraventricular and Intraparenchymal Intracranial Pressure Measurements. Neurosurgery. 2016;79:561–6. [DOI] [PubMed] [Google Scholar]
- 4.G.G. H, M.J. S, J.P. E, H.R. W, P.D. L. Relationship between intracranial pressure and other clinical variables in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2004; [DOI] [PubMed]
- 5.Olson DWM, Ortega Peréz S, Ramsay J, Venkatasubba Rao CP, Suarez JI, McNett M, et al. Differentiate the Source and Site of Intracranial Pressure Measurements Using More Precise Nomenclature. Neurocrit Care. 2019; [DOI] [PubMed]