Abstract
Background
Postpartum depression is an umbrella, which encompasses several mood disorders that follow childbirth within 6 weeks. Screening for postpartum depression would improve the ability to recognize these disorders and enhance care that ensures improved clinical outcomes. Early identification of postpartum depression is important in order to plan for implementation strategies that allow for timely treatment and support of women with postpartum depression.
Objective
To determine the prevalence and associated factors of postpartum depression among women who gave birth in the last six weeks in Gondar town, Northwest Ethiopia, 2018.
Methods
A community based cross-sectional study was conducted among 526 women who gave birth in the last 6 weeks from July 1 to 30, 2018 in Gondar town. Cluster sampling technique was used. Data were collected by semi-structured and pretested questionnaire and entered into epi-Info version 7.0 and then analyzed by SPSS version 20.0. Both bivariate and multivariable logistic regression model were fitted. Adjusted odds ratio with 95% confidence interval has been computed and variables with p-value <0.05 were considered statistically significant.
Results
The prevalence of postpartum depression among 526 postnatal women was 25% (95% CI: 21, 28). Abortion history (AOR = 1.79, 95% CI: 1.07, 2.97), birth weight <2.5 kg (AOR = 3.12, 95% CI: 1.78, 5.48), gestational age below 36 weeks (AOR = 2.18, 95% CI: 1.22, 3.88) unplanned pregnancy (AOR = 2.02, 95% CI: 1.24, 3.31), relatives' mental illness (AOR = 1.20: 1.09–3.05), had no antenatal visit (AOR = 4.05, 95% CI: 1.81, 9.05), had no postnatal visit (AOR = 1.82, 95% CI: 1.11, 3.00) were factors significantly associated with postpartum depression. Conclusion and Recommendations. The prevalence of PPD was found to be higher. Variables like abortion history, low birth weight, gestational age below 36 weeks, unplanned pregnancy, relatives' mental illness, had no antenatal visit, and had no postnatal visit were predisposing factors to postpartum depression. Preventive measures to avoid low birth weight and pregnancy complications are also identified as proactive ways to reduce postpartum depression. Early identification and treatment of depression during ANC and postpartum care can mitigate the impact of PPD on the mother-baby dyad. Emphasis must be given women to have ANC and PNC follow up.
1. Introduction
Postpartum depression is a very common problem, which occurs in women of childbearing age within 6 weeks of childbirth, but is often unrecognized or undiagnosed and a significant public health burden [1]. Risk factors for postpartum depression include social stressors, such as poverty, intimate partner violence, history of pregnancy loss, unintended pregnancy, and these variables have adverse effects on maternal health [2]. An important distinction that makes postpartum depression unique from other depression disorders is that it is marked by prominent anxiety components [3]. The problem of postnatal depression not only has immediate adverse effects on the mother, her newborn, child, and the family but can also lead to long-term morbidity of chronic or recurring depression [4].
Current models of postpartum care in developed countries originated in the beginning of the 20th century in response to the high maternal and neonatal mortality rates of the time [5]. Untreated postpartum depression can have adverse long-term effects. In addition to the maternal risk from chronic depression, offspring may exhibit emotional, behavioral, cognitive, and interpersonal impacts associated with their mother's depression [6].
Four million births occur in the world annually; approximately forty percent of new mothers are affected with different types of postpartum mood disorders including depression symptoms before and during pregnancy [7].
The relevance of this research on PPD establishes not only the regional prevalence of the disorder but identifies proactive approaches to both identify the disorder and modify the complications of PPD. The endpoint is to mediate the impact of PPD on the mother and child dyad, the family, and the community.
The prevalence of postpartum depression varies from 1.9% to 82.1% in developing countries [8]. Global studies show differing prevalence rates, with researchers in Canada reporting a prevalence of 40% [9], and in Jamaican 56% and 34% depression prevalence during prepartum and postpartum periods, respectively [9]. Studies show that the prevalence of postpartum depression is 9.2% in Sudan [10]. In addition, in a study carried out in eastern Tigray zone, Ethiopia, the prevalence of major depression at six weeks postpartum was 19% [11].
The effects of postnatal depression on the mother, her marital relationship, and her children make it an important condition to diagnose, treat, and prevent. The provision of care will vary depending on the socio-demographic and obstetric factors. Globally, PPD prevalence and associated risk factors are important to identify, especially in low and middle income countries.
The aim of this research is to translate this information to health care workers and to women in order to improve care related to PPD. The identification of the magnitude and risk factors that determine postpartum depression will help health care providers and other concerned bodies to suggest the diagnosis and interventions to be designed for the neglected postpartum depression. Postpartum depression is a neglected problem. It causes a lot to maternal ill health, jeopardizes the newborn health, and quite often destablizes the family. The study will also provide greater inputs to the government and program managers for designing of programs, proper implementation, and evaluation of their contribution for the achievement of the new adopted agenda as Sustainable Development Goals (SDGs) in relation with postpartum depression.
2. Method
2.1. Study Design & Period
A community based cross-sectional study design was conducted from July 1 to 30, 2018.
2.2. Study Area
The study was conducted in Gondar town which is located 750 km from Northwest of Addis Ababa, the capital city of Ethiopia. According to the 2017 population projection, the total population size of Gondar town was estimated to be 338,646. From the total population of Gondar city 23.58% were women in the reproductive age group. The city has one comprehensive specialized hospital, 8 health centers, and three private maternity specialty clinics that give maternity services and one private primary hospital.
2.3. Source Population
All women who gave birth in Gondar town.
2.4. Study Population
All women who gave birth in the last 6 weeks prior to the study period and reside more than 6 months in the selected Kebele of Gondar town.
2.5. Inclusion Criteria
All mothers who gave birth 6 weeks prior to the data collection period at the selected kebeles of Gondar city.
2.6. Sample Size Estimation
The sample size was determined by considering the assumptions for single proportion formula.
| (1) |
n = initial sample size,
a = level of significance,
p = prevalence of ante partum depression (19%) [12],
w = marginal error of 5%,
| (2) |
By assuming 2 design effect and 10% of nonresponse rate.
Sample size was =519 but I have got 7 additional participants in the cluster. The final sample size was 526.
2.7. Sampling Procedure
Gondar town has a total of 21 kebeles. The reference population was homogeneous, we use those 21 kebeles as a cluster; from these 8 kebeles were selected randomly using the lottery method. Then from each selected clusters, we took all women who gave birth in the last six weeks. Then the data collector used map and location of the urban health extension workers to get selected mothers as shown in the following (Figure 1).
Figure 1.
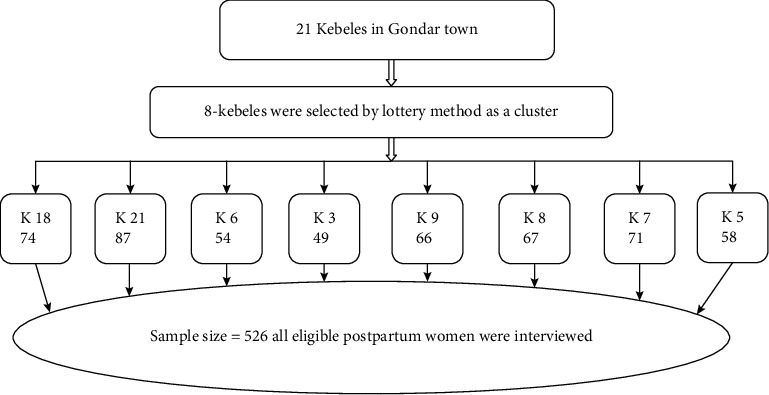
Schematic presentation of sampling procedure to assess prevalence and associated factors of postpartum depression among women who gave birth in the last six weeks at Gondar town, Northwest Ethiopia, 2018 (n = 526).
2.8. Variables of the Study
2.8.1. Dependent variable
Postpartum depression
2.8.2. Independent variable
Socio-demographic variables: age, ethnic group, marital status, educational level, residence.
Obstetric variables: parity, premature labor, unplanned pregnancy, losing or hospitalizing a baby, mode of delivery, pregnancy complication or illness, stressful life event during pregnancy, experienced death of baby, and undesired fetal sex. Previous psychiatric history: history of depression and family history of psychiatric problems, and social support.Social support: poor husband support, domestic violence, child birth without the presence of any relatives, unsatisfactory relationship with mother-in-law, unsatisfactory relationship with husband.
2.9. Operational Definitions
2.9.1. Postpartum Depression (PPD)
Postpartum depression is a psychiatric disorder that occurs in the women following delivery up to six weeks if ≥13 according to (EPDS). In the scale, the question numbers 1, 2, & 4 are scored 0, 1, 2, & 3 with first choice scored as 0, and the last choice scored 3, and question numbers 3, 5–10 are reversely scored with the first choice as 3 and the last choice scored as 0. After adding up all the scores, women who scored greater than or equal to 13 were concluded to have postpartum depression.
2.9.2. History of Depression
Women who had mental illness that can interfere with a person's life. Sever feelings of sadness, hopelessness, and loss of interest in activities.
2.9.3. Happy Spouse
Happy relationship/marriage with husband.
2.9.4. Data Collection Tools and Procedures
Data were collected through pretested semi-structured face to face interview. The semi-structured questionnaires were prepared in local language, Amharic, to make it simple and understandable. One diploma midwifery student in each kebele for data collection and two BSc midwifery supervisors, total of 8 data collectors and 2 supervisors were recruited.
2.9.5. Data Quality Control
The questionnaire was prepared in English, and then translated to Amharic (local language) and back to English to maintain consistency of the tool. Training was provided for data collectors and supervisors for one day about the purpose of the study and techniques of data collection. The trained data collectors were supervised during data collection and each questionnaire was checked for completeness in a daily basis. Data entry was conducted and it was cross checked. The questionnaire was pretested to check the response, language clarity, and appropriateness of the questionnaire, while the pretest was done outside study area at Maksegnit city with 5% of sample size. At the end of the pretest depending on its outcome, the correction measures were under taken.
2.9.6. Data Processing and Analysis
Data cleaning was performed to check for accuracy, completeness, consistencies, and missed values and variables. After the data had been checked for completeness and accuracy, it was coded manually and then entered to Epi Info version 7.0 and exported to Statistical Package of Social Science (SPSS) version 20 for analysis. Descriptive statistics was performed on numerical value, standard deviation, frequencies, proportion to describe study population in relation to dependent and independent variables. Binary logistic regression was used to identify statistically significant independent variables and independent variables having p-value less than 0.2 will go to multivariable logistic regression for further analysis. Adjusted odds ratio with 95% confidence interval was used to determine the degree and direction of association between covariates and the outcome variable. To adjust for confounding variables, a multivariable logistic regression was done, model fitness was checked using Hosmer–Lemeshow goodness of fit test, and a p-value <0.05 with 95% confidence interval for odds ratio (OR) was used to determine significance.
2.9.7. Ethical Clearance
Ethical clearance was obtained from the Institutional Review Board (IRB) of University of Gondar on behalf of the Ethics Review Committee of the department of midwifery. A letter of cooperation was obtained from Gondar town health office. The reasons why the research was to be done was explained to the study subjects; informed consent was obtained from each study subject after explanation of the purpose of the study, and involvement (to be participant) was after their complete consent. Any mother who was not willing to participate in the study was not forced to participate, no personal identifications were included in the data sheet, and all data taken from the participants were kept strictly confidential and used only for the study purpose.
3. Result
3.1. Socio-Demographic Characteristics of Participants
A total of 526 women were enrolled and the response rate was 100%. Mean age of the study participants was 28.7 years (standard deviation = 5.2) and 65.6% of them were orthodox Christians. More than three-fourths of the participants were married (80%). Nearly two-thirds of the respondents were (69.2%) up to intermediate in education and 42% of them were housewife by occupation. On the other hand, 68.9% of their husbands had working job (Table 1).
Table 1.
Socio-demographic and economic related characteristics of women in Gondar town who gave birth in the last 6 weeks, Northwest Ethiopia, 2018, (n = 526).
| Variables | Frequency | Percent (%) |
|---|---|---|
| Ethnicity | ||
| Amhara | 394 | 74.9 |
| Others∗ | 132 | 25.1 |
| Religion | ||
| Orthodox | 345 | 65.6 |
| Others∗∗ | 181 | 34.4 |
| Current maternal age (in years) | ||
| Below 30 | 299 | 56.8 |
| 30 and above | 227 | 43.2 |
| Marital status | ||
| In marital relation | 421 | 80.04 |
| Not in marital relation | 105 | 19.96 |
| Maternal education | ||
| Non educated | 14 | 2.7% |
| Up to intermediate | 364 | 69.2 |
| College and above | 148 | 28.1 |
| Husband education ( n = 421 ) | ||
| Noneducated | 10 | 2.4 |
| Inter-mediate | 234 | 55.6 |
| College and above | 177 | 34 |
| Maternal occupation | ||
| House wife | 221 | 42 |
| Student | 46 | 8.8 |
| Employed | 232 | 44.1 |
| Daily labor | 27 | 5.1 |
| Husband occupation ( n = 421 ) | ||
| Employed | 290 | 68.9 |
| Merchant | 101 | 24 |
| Daily labor | 30 | 7.1 |
| Family income (ETB∗ | ||
| <750 ETB | 24 | 4.56% |
| 750–1200 ETB | 53 | 10.08% |
| >1200 ETB | 449 | 85.36% |
Other∗ = Kemanit, Tigre, Gurage, Agew; other∗∗ = Muslim, catholic and protestant; ETB∗ = Ethiopian birr.
3.2. Obstetrics Related Characteristics of Respondents
More than one half (62%) of respondents had given birth below three times, while 65.2% of them had two or more living children. Fifty six (38.6%) of respondents had faced severe headache complication in the indexed pregnancy. Nearly half of the study subjects (58.56%) gave birth spontaneously vaginally. Around one half of the participants (50.8%) had four or more antenatal care whereas 53.5% of women had one postnatal care visit. Moreover, 15.2% of the indexed neonates were admitted to neonatal intensive care unit (Table 2).
Table 2.
Obstetrics related factors of women in Gondar town who gave birth in the last 6 weeks, Northwest Ethiopia, 2018, (n = 526).
| Variables | Frequency | Percent (%) |
|---|---|---|
| Parity | ||
| Below 3 | 326 | 62 |
| 3 and above | 200 | 38 |
| Live births | ||
| Below 2 | 183 | 34.8 |
| 2 and above | 343 | 65.2 |
| Ever had abortion | ||
| Yes | 117 | 22.2 |
| No | 409 | 77.8 |
| Total abortion ( n = 117 ) | ||
| Below two | 110 | 94 |
| Two and above | 7 | 6 |
| Mode of delivery | ||
| Spontaneous vaginal | 308 | 58.5 |
| Cesarean section | 186 | 35.4 |
| Instrumental | 32 | 6.1 |
| Birth weight | ||
| Below 2.5 kg | 95 | 18 |
| 2.5 kg and above | 431 | 82 |
| Gestational age in weeks | ||
| Below 36 weeks | 86 | 16.3 |
| 36 and above weeks | 440 | 83.7 |
| Planned pregnancy | ||
| Yes | 382 | 72.6 |
| No | 144 | 27.4 |
| Complication in the indexed pregnancy | ||
| Yes | 145 | 27.6 |
| No | 381 | 72.4 |
| Type of complication in the indexed pregnancy( n = 145 ) | ||
| Vaginal bleeding | 50 | 34.5 |
| Severe headache | 56 | 38.6 |
| Other∗ | 39 | 26.9 |
| ANC visit | ||
| Yes | 484 | 92 |
| No | 42 | 8 |
| Number of ANC visit ( n = 484 ) | ||
| Below 4 | 238 | 49.2 |
| 4 and above | 246 | 50.8 |
| Desired sex of the baby | ||
| Yes | 203 | 38.6 |
| No | 323 | 61.4 |
| PNC visit | ||
| Yes | 368 | 70 |
| No | 158 | 30 |
| Number of PNC visit ( n = 368 ) | ||
| Below 2 | 197 | 53.5 |
| 2 and above | 171 | 46.5 |
| Newborn admitted | ||
| Yes | 80 | 15.2 |
| No | 446 | 84.8 |
Other∗ = fever, swelling, blurring of vision and fetal movement.
3.3. Depression Related Characteristics of Respondents
Among the respondents, 46 (8.7%) of them had relatives with a mental illness history. Out of these, 60% of the women reported that her mother had mental illness problem. Sixty-three (12%) of the respondents had history of depression. Nearly three quarters of the candidate's husband (76%) were happy with their current marital status (Table 3).
Table 3.
Depression related characteristics of women who gave birth in the last 6 weeks at Gondar town, Northwest Ethiopia, 2018, (n = 526).
| Variables | Frequency | Percent (%) | ||
|---|---|---|---|---|
| Relatives' mental illness history | ||||
| Yes | 46 | 8.7 | ||
| No | 480 | 91.3 | ||
| Who had mental illness history ( n = 46 ) | ||||
| Mother | 28 | 60 | ||
| Other∗ | 18 | 40 | ||
| History of depression | ||||
| Yes | 63 | 12 | ||
| No | 463 | 88 | ||
| Happy with marriage | ||||
| Yes | 399 | 75.9 | ||
| No | 127 | 24.1 | ||
Other∗ = brother and sis.
3.4. Social-Support Related Characteristic of Respondents
Among the respondents, 19.2% of them were abused by their husbands. The common type (71.3%) of the abuse was verbal in kind. Most of the women relatives (88.8%) were present in health facilities in the indexed child birth. On the other hand, (55.3%) the respondents had happy relationship with their husband's family (Table 4).
Table 4.
Social-support characteristics of respondents who gave birth in the last 6 weeks in Gondar town, Northwest Ethiopia, 2018, (n = 526).
| Variables | Frequency | Percent (%) | ||
|---|---|---|---|---|
| Abused by your husband | ||||
| Yes | 101 | 19.2 | ||
| No | 425 | 80.8 | ||
| Type of abuse ( n = 101 ) | ||||
| Verbal | 72 | 71.3 | ||
| Physical | 24 | 23.8 | ||
| Other∗ | 5 | 4.9 | ||
| Presence of relatives at health institutions during delivery | ||||
| Yes | 467 | 88.8 | ||
| No | 59 | 11.2 | ||
| Happy relationship with your husband's families | ||||
| Yes | 291 | 55.3 | ||
| No | 235 | 44.7 | ||
Other∗ = verbal and physical.
3.5. Prevalence of Postpartum Depression
From the entire respondents the prevalence of postpartum depression was found to be 25% (95% CI: 21–28) as shown in Figure 2.
Figure 2.
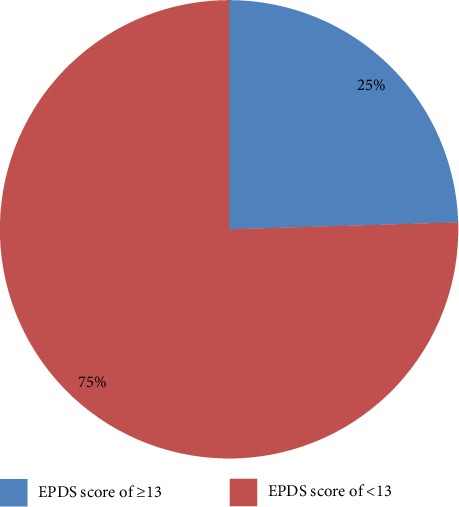
Prevalence of postnatal depression among women who gave birth in the last 6 weeks in Gondar town, Northwest Ethiopia, 2018 (n = 526).
3.6. Factors Associated with Postpartum Depression
The bivariate logistic regression analysis revealed that husband's occupation, income, live children, women who had abortion history, weight of newborn infant, gestational age at birth, planned pregnancy, complication during last pregnancy, ANC visit, PNC visit, history of relatives' mental illness, previous history of depression, happy with spouse, and relatives present at health facilities in the indexed delivery had association of postpartum depression at p-value less than 0.2.
Concerning multivariable logistic regression analysis, abortion history, birth weight, gestational age, planned pregnancy, ANC visit, history of relatives' mental illness, and women who had PNC visit were found to be significant associated factors of postpartum depression at P-Value <0.05.
According to this study, the odds of developing postpartum depression among women who ever had abortion were nearly two times than those who had no abortion history (AOR = 1.79, 95% CI: 1.07, 2.97).
In the current study, women who had low birth weight (<2.5 kg) new born were three times more likely to develop postpartum depression as compared to their counter parts (AOR = 3.12, 95% CI: 1.78, 5.48).
In this statistical analysis, respondents who gave birth below 36 weeks of gestational age were two times more likely to develop postpartum depression as compared to women who delivered at gestational age of 36 or more weeks (AOR = 2.18, 95% CI: 1.22, 3.88).
It was noted that unplanned pregnancy has been associated with the development of postpartum depression. The odds of developing postpartum depression among respondents who had unplanned pregnancies were two times than those women who had planned pregnancies (AOR = 2.02, 95% CI: 1.24, 3.31).
Participants who did not have antenatal visits were exposed to postpartum depression development. The study revealed that respondents who did not have antenatal visits were four times more likely to be depressed compared to those who had antenatal follow-up (AOR = 4.05, 95% CI: 1.81, 9.05). There is also a strong relationship between postnatal visit and postnatal depression. In this study, the odds of developing postpartum depression among respondents who did not have postnatal visits were nearly two times more likely to be depressed than those who had postnatal visits (AOR = 1.82, 95% CI: 1.11, 3.00). The report also declared that the odds of developing postpartum depression among participants whose relatives had mental illness history were 1.2 times more likely to be depressed than those whose relatives did not have mental illness history (AOR = 1.20, 95% CI: 1.09, 3.05) (Table 5).
Table 5.
Associated factors of postpartum depression among women who gave birth in the last 6 weeks in Gondar town (n = 526), 2018.
| Variable | PPD | COR [95% CI] | AOR [95% CI] | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Live birth | ||||
| Below 2 | 52 (28.4) | 131 (71.6) | 1 | 1 |
| 2 and above | 77 (22.4) | 266 (77.6) | 1.37 (0.48,1.10) | 0.99 (0.55, 1.79) |
| Ever had abortion | ||||
| Yes | 41 (35) | 76 (65) | 1.97 (1.26, 3.08) | 1.79 (1.07, 2.97)∗ |
| No | 88 (21.5) | 321 (78.5) | 1 | 1 |
| Birth weight | ||||
| Below 2.5 kg | 45 (47.4) | 50 (52.6) | 3.72 (2.33, 5.94) | 3.12 (1.78, 5.48)∗∗∗ |
| 2.5 kg and above | 84 (19.5) | 347 (80.5) | 1 | 1 |
| Gestational age in weeks | ||||
| Below 36 | 41 (47.7) | 45 (52.3) | 3.64 (2.25, 5.91) | 2.18 (1.22, 3.88)∗ |
| 36 and above | 88 (20) | 352 (80) | 1 | 1 |
| Planned pregnancy | ||||
| Yes | 72 (18.8) | 310 (81.2) | 1 | 1 |
| No | 57 (39.5) | 87 (60.5) | 2.82 (1.85, 4.30) | 2.02 (1.24, 3.31)∗∗ |
| Complication in the indexed pregnancy | ||||
| Yes | 46 (31.7) | 99 (68.3) | 1.67 (1.09, 2.55) | 1.19 (0.71, 1.97) |
| No | 83 (21.8) | 298 (78.2) | 1 | 1 |
| ANC visit | ||||
| Yes | 100 (20.7) | 384 (79.3) | 1 | 1 |
| No | 29 (69) | 13 (31) | 8.6 (4.30, 17.08) | 4.05 (1.81, 9.05)∗∗ |
| PNC visit | ||||
| Yes | 67 (18.2) | 301 (81.8) | 1 | 1 |
| No | 62 (43.1) | 96 (56.9) | 2.90 (1.92, 4.39) | 1.82 (1.11, 3.00)∗ |
| Relatives' mental illness history | ||||
| Yes | 15 (32.6) | 31 (67.4) | 1.55 (0.81, 2.98) | 1.20 (1.09, 3.05) |
| No | 114 (23.8) | 366 (76.2) | 1 | 1 |
| History of depression | ||||
| Yes | 25 (36.8) | 38 (63.2) | 2.27 (1.31, 3.94) | 1.35 (0.68, 2.67) |
| No | 104 (22.5) | 359 (77.5) | 1 | 1 |
| Presence of relatives at institution during delivery | ||||
| Yes | 107 (22.9) | 360 (77.1) | 1 | 1 |
| No | 22 (37.3) | 37 (62.7) | 2.00 (1.13, 3.54) | 0.97 (0.46, 1.85) |
Note. ∗∗∗ = P value <0.001, ∗∗ = P value <0.01, ∗ = P value <0.05.
4. Discussion
The aim of this study was to assess the prevalence and associated factors of postpartum depression among women who gave birth in Gondar town, Ethiopia.
The study evidenced that the prevalence of postpartum depression was found to be 25%. This finding is in accordance with studies conducted in Iran—23.2% [12] and 28.1% in the Trabzon province [13]. However, the reports of the current study were found to be higher compared to studies done in Canada 8.69% [14], New Delhi 12.75% [15], Kampala-Ugandan urban primary health care 6.1% [16], Gujarati 12.5% [1], Harare Ethiopia 13% [17], and 19% prevalence in the eastern zone of Tigray [11]. The possible explanation might be the differences in study setting and type of design utilized. The other difference might be 68.2% of the respondents in this study were secondary and above by education. Higher educational levels for mothers may contribute to reporting postpartum depression, as they are aware of their depression and are empowered to report the symptoms. This also attributes that women with good educational level may have intellectual skills and better copying strategies.
On the other hand, the estimate of postpartum depression in the current study was lower than the study conducted in Victoria South Australia 38.3% [18], Nepal University Hospital 29% [19], Rawalpindi General Hospital 33.1% [20], in Cape-Town 45.1% [21], in Turkey 32.1% [12], and 48.6% in Karachi, Pakistan [22]. The higher prevalence may be related to the site of delivery, as many studies listed were conducted in university hospitals and regional referral centers. The findings may also be impacted by those patients who have access to care and those who seek care for depression in the postpartum period. The other explanation might be due to socio-cultural differences of respondents. It is vital to consider the role of culture and the impact patient's beliefs and the cultural support for receiving help for postpartum depression.
Women who ever had abortion, birth weight below 2.5 kg, gestational age below 36 weeks, planned pregnancy, antenatal visit, relatives who had mental illness, and postnatal visit were factors significantly associated with development of postpartum depression.
According to this study, the odds of developing postpartum depression among respondents who ever had abortion were nearly two times more likely to be depressed compared to those who had no abortion history. This report was supported by studies conducted at Gujarati postpartum women [1] and rural southern Ethiopia [2]. This might be because of the fact that women who had abortion will pose different psychosocial problems and they might regret for fear of complication development during their life of pregnancy.
The study revealed that the odds of developing postpartum depression among respondents whose new born child with low birth weight were three times more likely to be depressed as compared those who had high birth weight (≥2.5 kg) of new born. This report was in accordance with studies conducted in Canada [23]. This could be that depressed or anxious women may have exaggerated pessimistic concerns about the health of their newborn compared with those women who are psychologically well. Lastly, it might be due to the reason that low birth weight is likely to cause women to feel depressed for the newborn and to feel that she has failed to fulfill the baby's needs during her life span of pregnancy.
In this statistical analysis, respondents who gave birth below 36 weeks of gestational age were two times more likely to be depressed compared to those who gave birth at gestational age of 36 or more weeks. This finding is supported by a study conducted in Canada [23], Istanbul, Turkey [12], Arabic women [24], and Harare, Ethiopia [11]. The study might be due to the uncertainty about the survival of the newborn and doubts about one's capacity to cope with the care of an abnormal or ill newborn child.
It was noted that unplanned pregnancy has been associated with the development of postpartum depression. The odds of developing postpartum depression among respondents who had unplanned pregnancies were two times more likely to be depressed compared those whose pregnancies were planned. The result was supported with studies conducted in Uganda, and Nigeria [11, 25], Istanbul, Turkey [26], Kuwait [1], and Harare, Ethiopia [11]. The possible explanation might be because in African cultures child bearing was so widely desirable that issues of whether a baby was wanted never arose, even though individual women might not be psychologically or economically prepared for pregnancy. An unplanned baby's birth is likely to affect the whole life and career plans of a woman. This unplanned life course may predispose women to develop depression in her postpartum period.
Participants who did not have antenatal visits were exposed for development of postpartum depression. The study revealed that respondents who did not have antenatal visits were four times more likely to be depressed compared to those who had antenatal follow-up. This report was in agreement with studies conducted at north Carolina, Colorado [27], Khartoum, Sudan [28] and Gondar University Hospital, Ethiopia [29]. The study results may be affected by the care given during the antenatal care visits, where counseling and anticipatory guidance is given by care providers to expectant mothers. The care may build maternal self-esteem and resiliency, along with knowledge about normal and problem complications to discuss at care visits. Mothers who value ANC care may also have different views on their right to mental and physical wellness, including access to care.
There is also a strong relationship between postnatal visit and postnatal depression. In this study, the odds of developing postpartum depression among respondents who did not have postnatal visits were nearly two times more likely to be depressed compared to those who had postnatal visits. Although assumed that accessing care would lead to increased diagnosis of postpartum depression, the postpartum visits may in fact provide guidance, reassurance, and appropriate referrals that are unavailable to those who do not seek care. Health care professionals have an ability to both educate and empower mothers as they care for their babies, their families, and themselves.
The report also declared that the odds of developing postpartum depression among participants whose relatives had mental illness history were 1.2 times more likely to be depressed compared to those whose relatives did not have mental illness history. This finding was in accordance with studies conducted in Istanbul, Turkey [26], Bahraini [1], and Arba Minch, Ethiopia. The links between genetic pre-disposition to mood disorders, considering both nature and nurture are important to address. PPD may be seen as a “normal” condition for those who are acquainted with relatives with mood disorders, especially during the childbearing years. Family history of mental illness can be easily elicited in the ANC first visit history. This information targets women who may have additional PPD risks and need special attention during the postnatal period.
5. Conclusion and Recommendation
The prevalence of postpartum depression was found to be higher compared to the national target value. Factors that are associated with increased PPD include women who have had abortion history, low birth weight newborn, gave birth prematurely, had unplanned pregnancy, had no ANC follow up, and had no PNC follow up. Women at increased risks also had relatives with mental health histories, and those with previous history for depression were more likely to have postpartum depression after their birth.
Early identification and treatment of depression during postpartum care can mitigate the impact of PPD on the mother-baby dyad. Emphasis must be given women to have ANC and PNC follow-up.
Acknowledgments
The authors are very grateful to the University of Gondar for the approval of the ethical clearance. Our last gratitude goes to Gondar town administrative office and kebele leaders for their endless hospitality and commitment to make this project possible. They would also like to extend their appreciation to the study participants, supervisors, and data collectors.
Abbreviations
- CI:
Confidence interval
- EPDS:
Edinburgh postnatal depression scale
- PPD:
Postpartum depression
- PND:
Post natal depression
- SPSS:
Statistical package for social scientists
- SSA:
Sub saharan Africa
- WHO:
World health organization
- ANC:
Ante natal care
- PNC:
Post natal care.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Eyerualem Desta drafted the proposal. Mengstu Melkamu analyzed the data and drafted the paper. Both Mengstu Melkamu and Haymanot Alem approved the proposal with some revisions, participated in data analysis, and revised subsequent drafts of the paper. All authors read and approved the final manuscript. These authors contributed equally to this work.
References
- 1.Desai N. D., Mehta R. Y., Ganjiwale J. Study of prevalence and risk factors of postpartum depression. National Journal of Medical Research. 2012;2(2):194–8. [Google Scholar]
- 2.Telake A., Abebaw F., Girmay M., Charlotte H. Coping strategies of women with postpartum depression symptoms in rural Ethiopia: a cross-sectional community study. BMC Psychiatry. 2018;18(1):1–13. doi: 10.1186/s12888-018-1624-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leigh B., Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC psychiatry. 2008;8(1):1–24. doi: 10.1186/1471-244x-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World health organization. WHO Technical Consultation on Postpartum and Postnatal Care. Switzerland: WHO Press; 2010. [PubMed] [Google Scholar]
- 5.Stewart D. E., Robertson E., Dennis C.-L., Grace S. L., Wallington T. Postpartum depression: literature review of risk factors and interventions. Toronto: University Health Network Women’s Health Program for Toronto Public Health. 2003:1–289. [Google Scholar]
- 6.Iranfar S., Shakeri J., Ranjbar M., Nazhad Jafar P., Razaie M. Is unintended pregnancy a risk factor for depression in Iranian women? East Mediterr Health Journal. 2005;11(4):618–624. [PubMed] [Google Scholar]
- 7.Norhayati M. N., Nik Hazlina N. H., Asrenee A. R., Wan Emilin W. M. A. Magnitude and risk factors for postpartum symptoms: a literature review. Journal of Affective Disorders. 2015;175:34–52. doi: 10.1016/j.jad.2014.12.041. [DOI] [PubMed] [Google Scholar]
- 8.Wissart J., Parshad O., Kulkarni S. Prevalence of pre-and postpartum depression in Jamaican women. BMC Pregnancy and Childbirth. 2005;5(1) doi: 10.1186/1471-2393-5-15.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khalifa D. S., Glavin K., Bjertness E., Lien L. Postnatal depression among Sudanese women: prevalence and validation of the Edinburgh postnatal depression scale at 3 months postpartum. International Journal of Women's Health. 2015;7:1–8. doi: 10.2147/ijwh.s81401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deribachew H. M., Zaid T., Desta S., Berhe D. Assessment of prevalence and associated factors of postpartum depression among postpartum mothers in eastern zone of Tigray. European Journal of Pharmaceutical, and Medical Research. 2016;3(10):1–16. [Google Scholar]
- 11.Arikan I., Korkut Y., Demir B. K., Sahin S., Dibeklioglu S. E. The prevalence of postpartum depression and associated factors: a hospital-based descriptive study. Journal of Clinical and Analytical Medicine. 2017;8(4):300–5. doi: 10.4328/JCAM.5030. [DOI] [Google Scholar]
- 12.Mirza I., Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: systematic review. BMJ. 2004;328(7443):p. 794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayvaz S., Hocaoglu C., Tiryaki A., Ismail A. K. The incidence of postpartum depression in Trabzon province and the risk factors during gestation. Turkish Journal of Psychiatry. 2006;17(4):1–8. [PubMed] [Google Scholar]
- 14.Farheen Z., Aruna N., Ruby A., Arwalla R. Postpartum depression in women: a risk factor analysis. Journal of Clinical and Diagnostic Research. 2017;11(8):13–16. doi: 10.7860/jcdr/2017/25480.10479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakku J. N., Nakasi G., Mirembe F. Postpartum major depression at six weeks in primary health care: prevalence and associated factors. African Health Sciences. 2006;6(4):207–214. doi: 10.5555/afhs.2006.6.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abayneh S., Bilisuma T., Tiba A., Shewasinad S. Prevalence of postpartum depression and associated factors among postnatal women attending at Hiwot Fana Specialized University Hospital, Harar, East Ethiopia. Open Access Journal of Reproductive and Sexual Disorders. 2018;1(1):4–19. doi: 10.32474/oajrsd.2018.01.000102. [DOI] [Google Scholar]
- 17.Yelland J., Sutherland G., Brown S. J. Postpartum anxiety, depression and social health: findings from a population-based survey of Australian women. BMC Public Health. 2010;10(1):9. doi: 10.1186/1471-2458-10-771.771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kunwar D., Corey E. K., Sharma P., Risal A. Screening for postpartum depression and associated factors among women who deliver at a university hospital, Nepal. Kathmandu University Medical Journal. 2015;13(1):44–48. doi: 10.3126/kumj.v13i1.13752. [DOI] [PubMed] [Google Scholar]
- 19.Muneer A., Minhas F. A., Nizami A. T., Mujeeb F., Usmani A. T. Frequency and associated factors for postnatal depression. Journal of the College of Physicians and Surgeons Pakistan. 2009;19(4):236–9. [PubMed] [Google Scholar]
- 20.Prinsloo M., Matzopoulos R., Laubscher R., Myers J., Bradshaw D. Validating homicide rates in the Western Cape Province, South Africa: findings from the 2009 injury mortality survey. South African Medical Journal. 2016;106(2):193–5. doi: 10.7196/samj.2016.v106i2.10211. [DOI] [PubMed] [Google Scholar]
- 21.Ali N. S., Ali B. S., Azam I. S. Post partum anxiety and depression in peri-urban communities of Karachi, Pakistan: a quasi-experimental study. BMC Public Health. 2009;9(1) doi: 10.1186/1471-2458-9-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vigod S. N., Villegas L., Dennis C.-L., Ross L. E. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG: An International Journal of Obstetrics & Gynaecology. 2010;117(5):540–550. doi: 10.1111/j.1471-0528.2009.02493.x. [DOI] [PubMed] [Google Scholar]
- 23.Khublb A. prevalance of post partum depression among recently deliverying mother in Nablus and associated factors. ResearchGate. 2014:1–153. [Google Scholar]
- 24.Nakku J. N., Nakasi G., Mirembe F. Postpartum major depression at six weeks in primary health care: prevalence and associated factors. African Health Sciences. 2006;6(4) doi: 10.5555/afhs.2006.6.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sulyman D., Ayanda K. A., Dattijo L. M., Aminu B. M. Postnatal depression and its associated factors among Northeastern Nigerian women. Annals of Tropical Medicine and Public Health. 2016;9(3):p. 184. doi: 10.4103/1755-6783.179099. [DOI] [Google Scholar]
- 26.Jennifer G., Swathy S., Jenn L. Antenatal physical activity: investigating the effects on postpartum depression. Health. 2012;4(12):1276–1286. doi: 10.4236/health.2012.412188. [DOI] [Google Scholar]
- 27.Khalifa D. S., Glavin K., Bjertness E., Lien L. Determinants of postnatal depression in sudanese women at 3 months postpartum: a cross-sectional study. BMJ Open. 2016;6(3):1–8. doi: 10.1136/bmjopen-2015-009443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ayele T. A., Azale T., Alemu K., Abdissa Z., Mulat H., Fekadu A. Prevalence and associated factors of antenatal depression among women attending antenatal care service at gondar university hospital, Northwest Ethiopia. Plos One. 2016;11(5):1–13. doi: 10.1371/journal.pone.0155125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gebrekiros G., Manaye Y., Dessalegn A., Desta H., Genet G. Perinatal depression and associated factors among mothers in Southern Ethiopia: evidence from arba minch zuria health and demographic surveillance site. Psychiatry Journal. 2018;2018:12. doi: 10.1155/2018/7930684.7930684 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


