To the Editor: Despite the risk of rapid respiratory failure1 and cardiac complications2 due to Covid-19, it is unclear whether there is an association between Covid-19 and out-of-hospital cardiac arrest. The Lombardy region of Italy was among the first areas to have an outbreak of Covid-19 outside China,3 and the first case there was diagnosed on February 20, 2020, in Lodi Province.4
Using the Lombardia Cardiac Arrest Registry (Lombardia CARe), we compared out-of-hospital cardiac arrests that occurred in the provinces of Lodi, Cremona, Pavia, and Mantua during the first 40 days of the Covid-19 outbreak (February 21 through March 31, 2020) with those that occurred during the same period in 2019 (February 21 through April 1, to account for the leap year). We reviewed daily reports of new Covid-19 cases recorded by the National Department of Civil Protection5 and cases of out-of-hospital cardiac arrest in the electronic database of the emergency medical system to identify either symptoms suggestive of Covid-19 (fever lasting ≥3 days before out-of-hospital cardiac arrest, with cough, dyspnea, or both) or positive results of testing to detect SARS-CoV-2 in pharyngeal swabs obtained before the out-of-hospital cardiac arrest or after death. (Details are provided in the Supplementary Appendix, available with the full text of this article at NEJM.org.)
During the study period in 2020, a total of 9806 cases of Covid-19 were reported in the study territory. During this period, 362 cases of out-of-hospital cardiac arrest were identified, as compared with 229 cases identified during the same period in 2019 (a 58% increase). Increases of various magnitudes in the numbers of cases of out-of-hospital cardiac arrest were seen in all four provinces (Table S1 in the Supplementary Appendix). The sex and age of the patients were similar in the 2020 and 2019 periods, but in 2020, the incidence of out-of-hospital cardiac arrest due to a medical cause was 6.5 percentage points higher, the incidence of out-of-hospital cardiac arrest at home was 7.3 percentage points higher, and the incidence of unwitnessed cardiac arrest was 11.3 percentage points higher (Table S2). The median arrival time of the emergency medical service was 3 minutes longer in 2020 than in 2019, and the proportion of patients who received cardiopulmonary resuscitation from bystanders was 15.6 percentage points lower. Among patients in whom resuscitation was attempted by the emergency medical service, the incidence of out-of-hospital death was 14.9 percentage points higher in 2020 than in 2019.
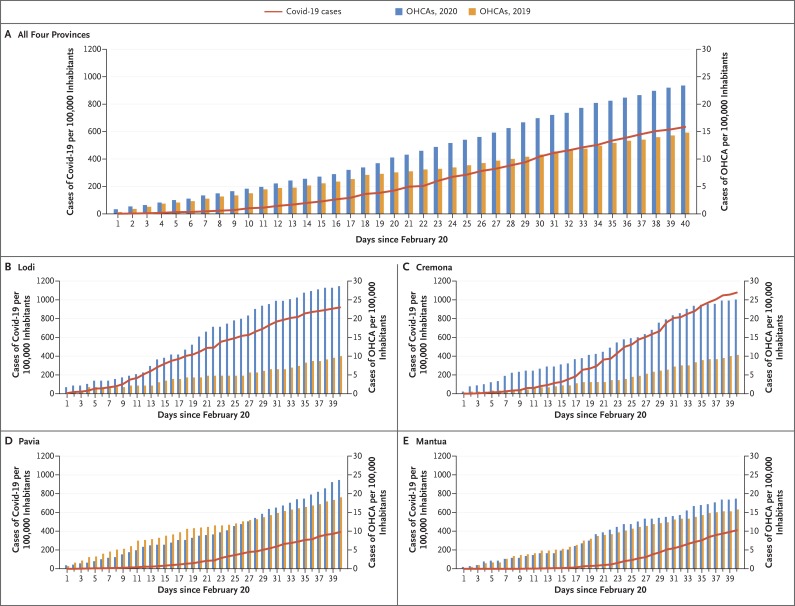
The cumulative incidence of out-of-hospital cardiac arrest in 2020 was strongly associated with the cumulative incidence of Covid-19 (Spearman rank correlation coefficient, 0.87; 95% confidence interval, 0.83 to 0.91; P<0.001), and the increase in the number of cases of out-of-hospital cardiac arrest over the number in 2019 (133 additional cases) followed the time course of the Covid-19 outbreak (Figure 1). A total of 103 patients who had out-of-hospital cardiac arrest (Table S3) were suspected to have or had received a diagnosis of Covid-19 (87 and 16 patients, respectively); these numbers account for 77.4% of the increase in cases of out-of-hospital cardiac arrest observed in these provinces in 2020.
Figure 1. Cumulative Incidences of Diagnosed Covid-19 and Cases of Out-of-Hospital Cardiac Arrest (OHCA) in Four Provinces in Lombardy, Italy, during the 40 days after February 20 in 2019 and 2020.
Panel A shows the data for all four provinces, and the other panels show the data for each individual province (Panel B, Lodi; Panel C, Cremona; Panel D, Pavia; and Panel E, Mantua). The vertical blue bars show the cumulative numbers of cases of OHCA per 100,000 inhabitants from February 21 through March 31, 2020, and the vertical orange bars show the cumulative numbers of cases of OHCA per 100,000 inhabitants from February 21 through April 1, 2019. The red line shows the cumulative number of cases of Covid-19 per 100,000 inhabitants in 2020.
Supplementary Appendix
Disclosure Forms
This letter was published on April 29, 2020, at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.MacLaren G, Fisher D, Brodie D. Preparing for the most critically ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation. JAMA 2020. February 19 (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 2.Clerkin KJ, Fried JA, Raikhelkar J, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation 2020. March 21 (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 3.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020. March 23 (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 5.Protezione Civile National Department Repository home page (https://github.com/pcm-dpc/COVID-19/tree/master/dati-province).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.