Abstract
Objectives. To estimate the economic burden of untreated perinatal mood and anxiety disorders (PMADs) among 2017 births in the United States.
Methods. We developed a mathematical model based on a cost-of-illness approach to estimate the impacts of exposure to untreated PMADs on mothers and children. Our model estimated the costs incurred by mothers and their babies born in 2017, projected from conception through the first 5 years of the birth cohort’s lives. We determined model inputs from secondary data sources and a literature review.
Results. We estimated PMADs to cost $14 billion for the 2017 birth cohort from conception to 5 years postpartum. The average cost per affected mother–child dyad was about $31 800. Mothers incurred 65% of the costs; children incurred 35%. The largest costs were attributable to reduced economic productivity among affected mothers, more preterm births, and increases in other maternal health expenditures.
Conclusions. The US economic burden of PMADs is high. Efforts to lower the prevalence of untreated PMADs could lead to substantial economic savings for employers, insurers, the government, and society.
Perinatal mood and anxiety disorders (PMADs)—defined as mood and anxiety disorders during pregnancy and the year following birth—are common in the United States, affecting at least 1 in 7 pregnant and postpartum women,1–12 yet they often go undiagnosed and untreated. Although screening tools and effective treatments exist, 60% of perinatal women with depressive symptoms do not receive a clinical diagnosis, and 50% with a diagnosis do not receive treatment.13 If left untreated, PMADs can have serious health and social consequences for both mother and child, including lower productivity—defined as lost earnings because of the inability to work or suboptimal performance while at work—for the mother and worse health for both the mother and child.14
Policymakers and health care payers have paid scant attention to PMADs in the United States, in part because of the lack of published evidence on costs of untreated PMADs. Health insurers, employers, and policymakers need credible and transparent estimates of the economic burden of PMADs. Several studies have examined the costs of untreated PMADs in other countries, such as the United Kingdom and Australia,15,16 but, to our knowledge, this study is the first to provide a comprehensive picture of the economic burden of PMADs in the United States.
We developed a mathematical model to quantify the societal costs of untreated PMADs and used recent data and estimates from peer-reviewed literature. We concentrated on the mother–child dyad’s costs during the first several years of life (conception through age 5 years) to highlight the most pressing concerns relevant to the public and decision makers. Although other studies have documented long-term impacts of exposure to untreated PMADs on children, these effects do not manifest themselves for many years. Limiting the model timeframe to 6 years enabled us to generate more concrete estimates than would be possible over a longer period.
METHODS
Our model considered impacts of exposure to untreated PMADs on mother and child. It estimated societal costs, including health care payer and employer costs, incurred by mothers and their babies born in 2017, projected forward for 6 years. The model focused on outcomes shown in the literature and recognized by subject matter experts as linked to PMADs (e.g., preterm birth). We looked at direct and indirect costs of untreated PMADs in 3 key domains: (1) income loss because of reduced maternal productivity and labor force participation; (2) greater use of public sector services, including safety net programs and Medicaid; and (3) higher health care costs attributable to worse maternal and child health.
The model used a cost-of-illness approach to synthesize existing evidence from multiple data sources about the effects of untreated PMADs on mother and child. We relied on literature and secondary data sources to inform model inputs, including (1) impact estimates, which measure incremental effects associated with exposure to untreated PMADs (vs no exposure); (2) prevalence estimates of PMADs in the United States; and (3) associated costs and baseline rates of each outcome. We did not estimate costs of prenatal and postnatal PMADs separately, nor mood disorders versus anxiety disorders.
Literature Review
We extracted effect sizes from literature on exposure to untreated PMADs on outcomes of interest. We identified original articles published in peer-reviewed scientific journals by using the MEDLINE, PsycINFO, CINAHL, and EconLit databases and key search terms. We augmented our literature search with (1) references from articles found through our literature search, (2) references from other publications that discuss costs and effects of PMADs, and (3) literature that subject matter experts in our advisory group recommended (Appendix A, Table A, available as a supplement to the online version of this article at http://www.ajph.org, lists the members of our advisory group). We focused on articles published over an approximately 10-year period: January 1, 2008, to August 22, 2018. For PMAD-related outcomes that had appeared in few articles, we conducted additional targeted searches to fill evidence gaps, including articles published before 2008. Appendix B (available as a supplement to the online version of this article at http://www.ajph.org) describes our literature review process and search terms used.
After excluding papers based on titles, we reviewed abstracts to determine each paper’s relevance to our study. We identified 170 candidate papers and used the following inclusion criteria to assess each study and determine its appropriateness for use in the model. Each study (1) included controls for confounders or used a matched-comparison group design to strengthen the evidence of associations between PMAD exposure and the effects of interest, (2) used outcomes relevant to the 6-year timeframe of our model, and (3) quantified outcomes in monetary terms.
Next, we extracted impact estimates for relevant outcomes. Each impact estimate measures the expected change in a given outcome attributed to exposure to untreated PMADs. We used systematic reviews or meta-analyses to inform a range of estimates when possible. We prioritized studies conducted with a population in the United States. For the few outcomes that had limited evidence from US-based studies, we included evidence from studies conducted in other high-income countries, such as Canada. Table 1 shows the impact estimates from the final set of papers. Appendix C (available as a supplement to the online version of this article at http://www.ajph.org) describes the studies used to inform the impact estimates.
TABLE 1—
Parameters and Costs Used in the Model of the Financial Toll of Untreated Perinatal Mood and Anxiety Disorders Among 2017 Births: United States
| Parameter | Point Estimate (Range for Sensitivity Analysis) | Source |
| Baseline demographic characteristics | ||
| No. of births | 3 855 500 | 17 |
| No. of pregnanciesa | 5 908 600 | 18 |
| Prevalence of PMADs, % | 11.50 (7.40–23.80) | 2–12 |
| Other inputs | ||
| Medical care inflation, % | 2.03 | 19 |
| Discount rate, % | 3.00 | 20 |
| Women who do not achieve remission without treatment by end of first y postpartum, % | 33.33 (20.00–60.00) | 21 |
| Maternal outcomes | ||
| Maternal productivity | ||
| Labor force participation among women with children aged younger than 6 y, % | 62.20 | 22 |
| Per-capita expected cost of job absenteeism, $ | 888 (397–1 715) | 23–26 |
| Per-capita expected cost of job presenteeism, $ | 2 871 (392–5 554) | 24-26 |
| Baseline rate of unemployment, % | 4.90 | 27 |
| Likelihood of unemployment among women with PMADs, % | 6.37 (5.88–6.86) | 28 |
| Cost per unemployed woman, $ | 40 478 | 29 |
| Suicide | ||
| Baseline incidence among women, % | 0.01 | 30 |
| Likelihood among women with depression, % | 0.16 (0.14–0.19) | 31 |
| Annual cost per case, $ | 74 666 | 32,33 |
| Maternal obstetric health | ||
| Baseline incidence of preeclampsia, % | 3.80 | 34 |
| Likelihood of preeclampsia among women with PMADs, % | 7.32 (6.08–8.53) | 35,36 |
| Annual cost per case of preeclampsia, $ | 1 285 | 37 |
| Baseline incidence of cesarean delivery, % | 31.90 | 38 |
| Likelihood of cesarean delivery among women with PMADs, % | 39.61 (38.56–40.61) | 35,39 |
| Incremental cost per case of cesarean delivery, $ | 11 693 | 40 |
| Average peripartum stay, d | 2.60 | 41 |
| Average peripartum stay for women with PMADs, d | 2.86 (2.64–3.08) | 42 |
| Daily cost per inpatient stay, $ | 2 340 | 43 |
| Maternal health expenditures | ||
| Individual out-of-pocket expenditures for women without PMADs, $ | 616 (392–654) | 23 |
| Individual out-of-pocket expenditures for women with PMADs, $ | 934 (596–993) | 23 |
| Individual insurer expenditures for women without PMADs, $ | 3 615 (2 304–3 840) | 23 |
| Individual insurer expenditures for women with PMADs, $ | 5 234 (3 336–5 560) | 23 |
| Benefit receipt | ||
| SNAP receipt among families with children aged younger than 18 y, % | 50.10 | 44 |
| Likelihood of SNAP receipt among women with PMADs, % | 50.33 (50.24–50.42) | 45 |
| Cost per person on SNAP, $ | 1 599 | 46 |
| WIC receipt among women with children aged 5 y and younger, % | 27.30 | 47 |
| Likelihood of WIC receipt among women with PMADs, % | 27.48 (27.39–27.56) | 45 |
| Cost per WIC case, $ | 767 | 48 |
| Medicaid receipt among women aged 15–44 y, % | 18.20 | 49 |
| Likelihood of Medicaid among women with PMADs, % | 18.44 (18.35–18.54) | 45 |
| Cost per case of Medicaid, $ | 6 747 | 50,51 |
| TANF receipt among families with children aged younger than 18 y, % | 3.20 | 52,53 |
| Likelihood of TANF receipt among women with PMADs, % | 3.40 (3.29–3.51) | 45 |
| Cost per TANF case, $ | 10 146 | 54,55 |
| Child outcomes | ||
| Preterm birth | ||
| Baseline incidence, % | 9.80 | 56 |
| Probability among infants born to women with PMADs, % | 23.58 (7.16–35.06) | 57 |
| Incremental cost per infant with preterm birth, $ | 48 118 | 58 |
| Suboptimal breastfeeding | ||
| Baseline prevalence, % | 72.10 | 59 |
| Likelihood among women with PMADs, % | 67.12 (64.40–69.46) | 60 |
| Incremental cost per infant, $ | 1 864 | 61 |
| SIDS | ||
| Baseline incidence, % | 0.04 | 62 |
| Probability among babies born to mothers with PMADs, % | 0.15 (0.12–0.19) | 63,64 |
| Annual cost per case, $ | 21 066 | 65 |
| Child behavioral and developmental disorders | ||
| Baseline prevalence among children aged 2–8 y, % | 6.83 | 66 |
| Likelihood among children born to women with PMADs, % | 12.31 (11.06–13.52) | 67 |
| Incremental annual cost per child, $ | 10 892 | 68 |
| Childhood obesity | ||
| Baseline prevalence among children aged 2–5 y, % | 13.90 | 69 |
| Likelihood among children born to women with PMADs, % | 18.97 (4.32–29.72) | 70,71 |
| Incremental annual cost per child, $ | 233 | 72 |
| Child asthma | ||
| Baseline prevalence among children aged 0–4 y, % | 3.80 | 73 |
| Likelihood among children born to women with PMADs, % | 7.32 (6.08–8.53) | 74,75 |
| Incremental annual cost per child, $ | 2 867 | 76 |
| Child nonfatal injury | ||
| Baseline incidence among children aged 0–4 y, % | 12.90 | 77 |
| Likelihood among children born to women with PMADs, % | 16.37 (13.54–19.02) | 78,79 |
| Annual cost per injury, $ | 7 522 | 80 |
| Child emergency department visits | ||
| Baseline incidence among children aged 1–4 y, % | 46.20 | 81 |
| Likelihood among children born to women with PMADs, % | 65.54 (51.37–73.32) | 82,83 |
| Cost per visit for child, $ | 875 | 84 |
| Nonattendance of well-child care visits | ||
| Baseline likelihood among children aged 0–6 y, % | 35.00 | 85 |
| Likelihood among children born to women with PMADs, % | 51.22 (35.00–60.96) | 86 |
| Cost per visit, $ | 525 | 87 |
Note. PMAD = perinatal mood and anxiety disorder; SIDS = sudden infant death syndrome; SNAP = Supplemental Nutrition Assistance Program; TANF = Temporary Assistance for Needy Families; WIC = Special Supplemental Nutrition Program for Women, Infants, and Children.
The estimate applies to intended and unintended pregnancies in US women aged 15–44 y that resulted in abortion, fetal loss, or live birth in 2014.
We also conducted a literature search on the prevalence of PMADs in the United States. We defined perinatal mood and anxiety disorders to include depression, anxiety, panic disorders, obsessive–compulsive disorders, mood disorders, posttraumatic stress disorders, and psychiatric disorders in pregnant and postpartum women during the prenatal, postnatal, and postpartum periods. For our main model, we chose to use a recent estimate of 11.5%, which we identified based on data from the Pregnancy Risk Assessment Monitoring System, a Centers for Disease Control and Prevention (CDC) surveillance project.88 We used a range of prevalence estimates (7% to 25% of recent mothers) from literature in our sensitivity analyses.2–12 Appendix D (available as a supplement to the online version of this article at http://www.ajph.org) describes the studies we included to inform the prevalence estimates. Altogether, we included 10 studies to inform the prevalence of PMADs and 34 studies to inform the impact estimates.
Cost Estimates
Calculating the economic burden of PMADs required us to estimate the incremental costs of each outcome attributable to exposure to untreated PMADs. We collected cost data from the CDC, peer-reviewed literature, and government reports. We made assumptions to standardize costs to annual units, distinguish between downstream and upfront costs, and include direct and indirect cost estimates from the literature. We sought to avoid double counting of costs by disaggregating cost estimates into their subcomponents and excluded overlapping subcomponents. For example, the costs of suboptimal breastfeeding from the literature included costs attributable to higher risks of obesity, asthma, and sudden infant death syndrome (SIDS; among other worse health outcomes). Because we separately examined the costs of obesity, asthma, and SIDS in our model, we subtracted the costs of these categories from the “unit” cost of suboptimal breastfeeding, even though there is evidence that PMADs influence these outcomes independently of suboptimal breastfeeding. We adjusted all cost estimates to 2017 dollars by using the medical care component of the consumer price index for year 0. Table 1 provides estimate values and sources. Appendix E (available as a supplement to the online version of this article at http://www.ajph.org) describes the studies and data sources used to inform the cost estimates.
Baseline Rates
We identified the baseline rate of each outcome—that is, the outcome rate in the general population—relying on data from the CDC and other government agencies. We used the most recent statistic available and, when available, focused on statistics for the most relevant population (such as the rates of labor force participation among women with young children). Table 1 provides estimate values and sources.
Modeling
First, for each impact estimate, we defined a range of plausible values. If multiple high-quality, rigorous studies or sources examined the same outcome, we aggregated point estimates from these sources to define the range; we then used the mean value for the main model. However, if we had only a single study with an estimate, we used the confidence interval around the point estimate from that paper to define the range; if we could not locate a confidence interval, we varied the impact estimate by 25% in sensitivity analyses. If there were no rigorous studies for a given outcome, we estimated a range of values by using studies of depression among women broadly (rather than PMAD-specific studies). These outcomes included maternal suicide, presenteeism (suboptimal performance at work), and unemployment.
We added the impact estimate (standardized to a percentage-point change)—which measures the expected change in the outcome attributable to exposure to PMADs—to the rate of the outcome among the general population. This approach enabled us to calculate the expected rate of the outcomes among women with PMADs. For example, the impact estimate for preterm birth would measure incremental risk of a preterm birth for a woman with untreated PMADs relative to a woman without PMADs. Adding this estimate to the baseline rate of preterm birth for the general population yields an approximate likelihood of preterm birth for women with untreated PMADs.
To calculate aggregate excess costs of PMADs in a year, we multiplied individual incremental risk of the outcome by expected number of women with PMADs, then multiplied the product by incremental unit cost. We treated each outcome as separate and costs as additive.
To extrapolate costs from 1 year to 5 years postpartum, we made several assumptions:
We assumed that the following costs occurred only once during the model timeframe, either in year 0 or in the first year postpartum: increased rates of preeclampsia, increased rates of cesarean delivery, longer peripartum hospital stay, increased rates of preterm birth, increased rates of SIDS, and higher rates of suboptimal breastfeeding.
We assumed that costs occurred annually for the following outcomes, as long as the mother had PMADs: productivity losses, economic losses from suicide, increased health expenditures, increased child injuries, increased emergency department visits, and reduced attendance at well-child care visits. For these outcomes, we assumed that once the mother achieved remission, the negative impact of exposure to PMADs would drop to zero.
To calculate the number of mothers who recovered from untreated PMADs in the years following the birth, we assumed that about two thirds of women achieved remission by the end of the first year postpartum, even without treatment, and that this proportion remained constant in subsequent years, based on a meta-analysis by Vliegen et al.21
For the remaining outcomes, including child behavioral and developmental disorders and asthma, we assumed that the impact of exposure to untreated PMADs remained constant throughout the model timeframe. For example, we did not expect the child to recover from asthma, even if the mother recovered from PMADs.
Finally, following a US Public Health Service Task Force recommendation, we discounted costs at an annual rate of 3% to reflect the lower economic value of a delayed expense.20 We adjusted for inflation in costs when extrapolating beyond year 0 to 5 years postpartum, assuming that medical costs increased by 2.03% each year after year 0, based on the annual change in the medical care component of the consumer price index from 2017 to 2018. We organized the data and programmed the model in Microsoft Excel by using Visual Basic (Office 365, Microsoft, Redmond, WA).
RESULTS
The model estimated that the cost of untreated PMADs for the 2017 birth cohort, projected from conception to 5 years postpartum, was about $14.0 billion. There were 3 855 500 US births in 2017,17 which suggests that, among mothers who gave birth in 2017, about 443 383 mothers had PMADs (3 855 500 * 11.5% = 443 383). The average cost per affected woman was roughly $32 300. Slightly more than half of the costs occurred in year 0, the year of conception through birth, because there were several outcomes relevant in the first year only (e.g., obstetric expenditures). The mother incurred about 65% of the total costs and the child incurred 35%. Table 2 shows these model results.
TABLE 2—
Model Results for Costs of Untreated Perinatal Mood and Anxiety Disorder for the 2017 Birth Cohort, by Year (in Millions of Dollars): United States
| Outcomes | Total | Year 0 | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
| Maternal costs | |||||||
| Productivity losses | 4635 | 1769 | 602 | 614 | 626 | 639 | 652 |
| Suicide | 200 | 76 | 26 | 26 | 27 | 28 | 28 |
| Preeclampsiaa | 20 | 20 | 0 | 0 | 0 | 0 | 0 |
| Cesarean deliverya | 400 | 400 | 0 | 0 | 0 | 0 | 0 |
| Peripartum staya | 270 | 270 | 0 | 0 | 0 | 0 | 0 |
| Health expenditures | 3449 | 1316 | 448 | 457 | 466 | 475 | 485 |
| Benefit receipt | 166 | 28 | 29 | 30 | 30 | 31 | 31 |
| Child costs | |||||||
| Preterm birtha | 2 940 | 2 940 | 0 | 0 | 0 | 0 | 0 |
| Suboptimal breastfeedinga | 41 | 41 | 0 | 0 | 0 | 0 | 0 |
| SIDSa | 11 | 11 | 0 | 0 | 0 | 0 | 0 |
| Behavioral and developmental disorders | 1 551 | 265 | 270 | 276 | 281 | 287 | 293 |
| Obesity | 31 | 5 | 5 | 5 | 6 | 6 | 6 |
| Asthma | 262 | 45 | 46 | 47 | 48 | 49 | 50 |
| Injury | 18 | 7 | 2 | 2 | 2 | 2 | 2 |
| Emergency department visits | 197 | 75 | 26 | 26 | 27 | 27 | 28 |
| Nonattendance of well-child care visits | −99 | −38 | −13 | −13 | −13 | −14 | −14 |
| Total societal costs for 1 birth cohort | 14 090 | 7 230 | 1 440 | 1 469 | 1 499 | 1 530 | 1 561 |
| Cost per mother–child dyad with PMAD, over 0–5 y postpartum | 31 778 | ||||||
| Cost per mother–child dyad with PMAD, per y, averaged over 0–5 y postpartum | 5 296 |
Note. PMAD = perinatal mood and anxiety disorder; SIDS = sudden infant death syndrome.
Costs are assessed only once in the year of conception and birth. We assumed the other costs incurred annually for the 6 y of the model.
Maternal Outcomes
The expected annual costs per person with untreated PMADs attributable to absenteeism (inability to work while employed) and presenteeism (suboptimal performance while at work) were about $888 and $2871, respectively. The expected loss in economic output attributable to increased unemployment among mothers with untreated PMADs was about $40 478. Estimated productivity losses amounted to increased societal costs of $4.6 billion over the 6 years from the cohort’s birth to age 5 years.
Untreated PMADs increased suicide risk more than 20-fold, as the model estimated an excess of 1049 suicides among mothers of the birth cohort associated with PMADs. This estimate led to an increase of $200 million in societal costs over the 6 model years. Untreated PMADs were associated with an additional 15 615 women developing preeclampsia,34–36 34 168 women having cesarean deliveries, and 115 280 additional hospital days during delivery among mothers of the birth cohort, together amounting to an increase of $689 million in costs incurred during the birth year.
Individual out-of-pocket expenditures for health care (excluding obstetric care) were $318 higher per year for women with untreated PMADs, and insurer-paid expenditures were $1619 higher for each woman with untreated PMADs,23 leading to a $3.4 billion increase in societal health expenditures over the 6 years. Untreated PMADs were associated with an annual increase of 1651 women enrolled in Medicaid, 1570 women enrolled in the Supplemental Nutrition Assistance Program, 1359 women enrolled in Temporary Assistance for Needy Families, and 1196 women enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children, leading to a total increase in public assistance costs of $166 million over the 6 model years.
Child Outcomes
An additional 61 098 preterm births in the birth cohort were associated with untreated PMADs, leading to an increase in total societal costs of $2.9 billion incurred in the birth year. Untreated PMADs were associated with an additional 22 072 women per year not breastfeeding or breastfeeding suboptimally, leading to an increase of $41 million in total societal costs in the birth year. The cost associated with suboptimal breastfeeding is primarily attributable to higher incidence of preventable infant diseases and deaths.89 An estimated 516 additional infant deaths attributable to SIDS were associated with untreated PMADs in the birth cohort, which increased societal costs by $11 million in the birth year.
The number of children in the birth cohort who had behavioral and developmental disorders increased by an estimated 24 297 attributable to untreated PMADs, raising societal costs by $1.6 billion over 6 model years. An estimated 22 473 additional children in the cohort developed obesity attributable to untreated PMADs, costing society $31 million over 6 model years. Another 15 615 children in the cohort were estimated to develop asthma attributable to untreated PMADs, costing society $262 million over the 6 model years. Untreated PMADs led to an estimated 15 513 additional child injuries per year, costing society $18 million over the 6 model years.
Untreated PMADs increased emergency department visits by children aged 5 years and younger by an estimated 85 760 each year—an increase of $197 million in societal costs over the 6 model years. Because children of mothers with PMADs are more likely to miss well-child care visits than children of mothers without PMADs, untreated PMADs contributed to 71 914 fewer well-child visits each year, reducing total societal costs by $99 million. Moreover, this outcome most likely resulted in worse overall child health, as reflected in higher costs in other child health categories.
Sensitivity Analyses
We conducted deterministic 1-way sensitivity analyses to examine which model parameters were most sensitive. These analyses varied impact estimates, prevalence of PMADs, and rate of remission from untreated PMADs, as they had a higher degree of uncertainty than other parameters (e.g., in the literature, the estimates of the prevalence of PMADs in the United States range from 7% to 25%).2–12 We did not test model sensitivity to parameters such as baseline rates of outcomes because there is more certainty about those outcomes in the literature. Table 1 presents the range of input parameters we tested.
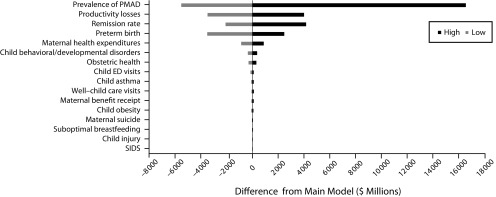
The tornado diagram (Figure 1) summarizes results of our 1-way sensitivity analysis. It shows the difference in costs (in dollars) from the main model as we varied each parameter, from lowest to highest value. The prevalence of PMADs had the strongest influence on model results ($8.6 to $30.5 billion) because we incorporated PMAD prevalence into almost all parts of the model. Furthermore, estimates of PMAD prevalence among US women varied substantially. The impact estimate on maternal productivity was the second most influential parameter, followed by the impact estimate on preterm birth and the remission rate from untreated PMADs. Not only did these parameters have large ranges in the literature, but also the associated costs of these outcomes were high, and therefore they caused large fluctuations in the model results.
FIGURE 1—
Tornado Diagram From 1-Way Sensitivity Analysis of the Financial Toll of Untreated Perinatal Mood and Anxiety Disorders Among 2017 Births: United States
Note. ED = emergency department; PMAD = perinatal mood and anxiety disorder; SIDS = sudden infant death syndrome.
The remainder of impact parameters did not appear to have a substantial effect on the results. This lack of impact was because the baseline rate of the outcome was low (e.g., suicide), the associated costs incurred during the model timeframe were low (e.g., child obesity), or the range of impact estimates was narrow (e.g., benefit receipt).
When we varied all model estimates from the low to the high end of the estimate ranges simultaneously, we found that costs of untreated PMADs for the 2017 birth cohort could range from $2.5 to $63.4 billion.
DISCUSSION
This study produced estimates of the economic burden of PMADs in the United States to inform the financial and public policy rationale for treatment. Our model estimated that the societal cost of untreated PMADs from conception through 5 years postpartum was $14 billion for the 2017 birth cohort. The cost per affected mother–child dyad over the 6 years of the model timeframe was close to $31 800, and the average annual cost of a mother–child dyad with PMADs was $5300. Approximately half of these costs occurred in the year of conception through birth. About two thirds of the costs of untreated PMADs from birth through the first 5 years of a child’s life were attributable to maternal outcomes, whereas one third were attributable to child outcomes.
We identified few other studies that focused on costs of untreated PMADs. One peer-reviewed study from the United Kingdom concluded that the lifetime cost of perinatal depression for 1 birth cohort was around £75 728 (or $95 000) per affected woman.16 This study used lifetime costs—whereas we focused on conception to 5 years postpartum—so its final cost estimates are not directly comparable with ours. An Australian study estimated the cost for the 2012 birth cohort over a 20-year period of untreated perinatal depression and anxiety to be $518 million in US dollars, which would be about $11 000 per affected woman.15 A report on the costs of untreated maternal depression in Minnesota estimated that the 2-generational annual economic cost of not treating 1 mother with maternal depression is $22 647, but the authors did not describe their methodology or sources.90
Limitations
Our model was subject to several limitations. First, although we conducted a systematic literature search, it was not feasible to include every possible outcome or cost in our review. Our cost results may therefore be downward biased. Second, although we designed inclusion criteria to include methodologically sound papers with adequate controls, the included studies may still not fully isolate the impact of PMADs because of unobserved confounders. Third, most of the existing evidence on the relationship between PMADs and the studied outcomes focused on perinatal depression rather than anxiety, with the majority of papers focusing on postpartum depression. To the extent that anxiety may predict the outcomes examined independently of depression, and women with both anxiety and depression may have even worse outcomes,91 our model estimates could be considered conservative. Furthermore, there are more studies on certain outcomes than others, so our confidence in each outcome is not uniform. Our limited use of literature from other countries with similar populations but different health care systems and care-seeking behaviors may introduce bias into the cost estimates. Fourth, although we worked to limit cost double-counting, we acknowledge that aggregate costs may still be overestimated because of remaining overlap of costs between outcomes. Fifth, model results are sensitive to the prevalence estimate of PMADs, which reflects the uncertainty in the prevalence of PMADs in the literature. When we varied the prevalence estimate to the lowest end of the range (7%) to the highest (25%), aggregate costs varied from $8.6 to $30.6 billion.
In addition, our model examined conception to 5 years postpartum, as this timeframe may be most relevant to policymakers. It may not capture other child outcomes outside that timeframe. For example, the effect of toxic stress on early childhood delinquency might not lead to costs captured during the model timeframe, although it may lead to higher costs in the future, such as reduced educational attainment or worse long-term health. Lifetime costs of PMADs are undoubtedly higher than the costs we found over a 6-year period.
Nonmaternal caregivers may also experience PMAD outcomes similar to those for mothers and children, such as paternal depression and absenteeism.92,93 We recognize that such outcomes have important societal costs, but our model focused only on the mother–child dyad. Had we included these other costs in our model, the overall burden on society would likely have been higher, so our results may underestimate the true societal burden of PMADs.
Finally, our model estimated the economic burden of untreated PMADs but did not explore the economic case for or costs of intervention. We did not incorporate treatment options, nor did we differentiate between no treatment and inadequate treatment of PMADs. Furthermore, we did not explore variations in treatment of PMADs or the impacts of treatment type on costs. These important areas for future research were beyond the scope of this study.
Public Health Implications
Untreated PMADs represent a heavy economic burden in the United States. Given that the United States underdiagnoses and undertreats these conditions, we sought to highlight the importance of addressing PMADs as a public health concern. Several medical societies—including the American College of Obstetricians and Gynecologists; the American Academy of Pediatrics; the Association of Women’s Health, Obstetric, and Neonatal Nurses; and the American Psychiatric Association94–97—recommend consistently screening perinatal women in obstetric or pediatric clinical settings and providing comprehensive treatment of PMADs, if indicated. Furthermore, the US Preventive Services Task Force recommends primary care screening for depression during pregnancy and postpartum98 and counseling interventions to prevent perinatal depression.99
Efforts to curb PMADs would not only benefit women’s and children’s health but would also improve women’s productivity and decrease their use of social services. This improvement would in turn benefit governments, employers, and health insurance payers. Stakeholders should support consistent screening during pregnancy through the first year postpartum and facilitate access to effective and affordable treatments.
ACKNOWLEDGMENTS
California Health Care Foundation, the Zoma Foundation, and the Perigee Fund provided funding for Mathematica to conduct this study.
CONFLICTS OF INTEREST
The authors have no conflicts to report.
HUMAN PARTICIPANT PROTECTION
Institutional board review was not required because there were no human participants involved in this study.
Footnotes
See also Ko and Haight, p. 765.
REFERENCES
- 1.US Preventive Services Task Force. Curry SJ, Krist AH et al. Interventions to prevent perinatal depression: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;321(6):580–587. doi: 10.1001/jama.2019.0007. [DOI] [PubMed] [Google Scholar]
- 2.Abbasi S, Chuang CH, Dagher R, Zhu J, Kjerulff K. Unintended pregnancy and postpartum depression among first-time mothers. J Womens Health (Larchmt) 2013;22(5):412–416. doi: 10.1089/jwh.2012.3926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol. 2004;103(4):698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- 4.Byatt N, Xiao RS, Dinh KH, Waring ME. Mental health care use in relation to depressive symptoms among pregnant women in the USA. Arch Womens Ment Health. 2016;19(1):187–191. doi: 10.1007/s00737-015-0524-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ertel KA, Rich-Edwards JW, Koenen KC. Maternal depression in the United States: nationally representative rates and risks. J Womens Health (Larchmt) 2011;20(11):1609–1617. doi: 10.1089/jwh.2010.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairbrother N, Janssen P, Antony MM, Tucker E, Young AH. Perinatal anxiety disorder prevalence and incidence. J Affect Disord. 2016;200:148–155. doi: 10.1016/j.jad.2015.12.082. [DOI] [PubMed] [Google Scholar]
- 7.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 pt 1):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 8.Ko JY, Rockhill KM. Trends in postpartum depressive symptoms—27 states, 2004, 2008, and 2012. MMWR Morb Mortal Wkly Rep. 2017;66(6):153–158. doi: 10.15585/mmwr.mm6606a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lépine JP, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011;7(suppl 1):3–7. doi: 10.2147/NDT.S19617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA. 2010;303(19):1961–1969. doi: 10.1001/jama.2010.605. [DOI] [PubMed] [Google Scholar]
- 11.Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burt VK. Mood disorders in women: focus on the postpartum. Women’s Health in Primary Care. 2006. 12–24. Available at: http://drvivienburt.com/2006/02/mood-disorders-in-women-focus-on-the-postpartum. Accessed April 7, 2019.
- 13.Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The perinatal depression treatment cascade: baby steps toward improving outcomes. J Clin Psychiatry. 2016;77(9):1189–1200. doi: 10.4088/JCP.15r10174. [DOI] [PubMed] [Google Scholar]
- 14.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Valuing perinatal health: the consequences of not treating perinatal depression and anxiety. London, England: PriceWaterhouseCoopers; 2014.
- 16.Bauer A, Knapp M, Parsonage M. Lifetime costs of perinatal anxiety and depression. J Affect Disord. 2016;192:83–90. doi: 10.1016/j.jad.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton BE, Martin JA, Osterman MJK, Driscoll AK, Rossen LM. Births: provisional data for 2017. Vital Statistics Rapid Release; no. 4. Hyattsville, MD: National Center for Health Statistics; 2018.
- 18.Frost JJ, Frohwirth LF, Zolna MR. Contraceptive needs and services, 2014 update. New York, NY: Guttmacher Institute; 2016.
- 19. Consumer price index for all urban consumers: medical care services. Washington, DC: US Bureau of Labor Statistics; 2019.
- 20.Sanders GD, Neumann PJ, Basu A et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–1103. doi: 10.1001/jama.2016.12195. [DOI] [PubMed] [Google Scholar]
- 21.Vliegen N, Casalin S, Luyten P. The course of postpartum depression: a review of longitudinal studies. Harv Rev Psychiatry. 2014;22(1):1–22. doi: 10.1097/HRP.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 22. The Economics Daily: Married mothers less likely to participate in labor force in 2017 than other moms. Washington, DC: US Bureau of Labor Statistics; 2018.
- 23.Ammerman RT, Chen J, Mallow PJ, Rizzo JA, Folger AT, Van Ginkel JB. Annual direct health care expenditures and employee absenteeism costs in high-risk, low-income mothers with major depression. J Affect Disord. 2016;190:386–394. doi: 10.1016/j.jad.2015.10.025. [DOI] [PubMed] [Google Scholar]
- 24.Evans-Lacko S, Knapp M. Global patterns of workplace productivity for people with depression: absenteeism and presenteeism costs across eight diverse countries. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1525–1537. doi: 10.1007/s00127-016-1278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rost K, Smith JL, Dickinson M. The effect of improving primary care depression management on employee absenteeism and productivity. A randomized trial. Med Care. 2004;42(12):1202–1210. doi: 10.1097/00005650-200412000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) J Clin Psychiatry. 2015;76(2):155–162. doi: 10.4088/JCP.14m09298. [DOI] [PubMed] [Google Scholar]
- 27. US Department of Labor, Women’s Bureau. Unemployment rates of mothers and fathers by age of youngest child (2016 annual averages). Washington, DC: US Department of Labor; 2016.
- 28.Lerner D, Henke RM. What does research tell us about depression, job performance, and work productivity? J Occup Environ Med. 2008;50(4):401–410. doi: 10.1097/JOM.0b013e31816bae50. [DOI] [PubMed] [Google Scholar]
- 29. Usual weekly earnings of wage and salary workers, fourth quarter 2018. Report 19-0077. Washington, DC: US Bureau of Labor Statistics; 2019.
- 30. Fatal injury reports, national, regional and state, 1981–2016. Atlanta, GA: Centers for Disease Control and Prevention; 2019.
- 31.Ösby U, Brandt L, Correia N, Ekbom A, Sparen P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58(9):844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- 32.Shepard DS, Gurewich D, Lwin AK, Reed GA, Jr, Silverman MM. Suicide and suicidal attempts in the United States: costs and policy implications. Suicide Life Threat Behav. 2016;46(3):352–362. doi: 10.1111/sltb.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Earnings in the past 12 months (in 2017 inflation-adjusted dollars). 2017 American Community Survey 1-year estimates. Washington, DC: US Census Bureau; 2017.
- 34.Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ. 2013;347:f6564. doi: 10.1136/bmj.f6564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bansil P, Kuklina EV, Meikle SF et al. Maternal and fetal outcomes among women with depression. J Womens Health (Larchmt) 2010;19(2):329–334. doi: 10.1089/jwh.2009.1387. [DOI] [PubMed] [Google Scholar]
- 36.Qiu C, Sanchez SE, Lam N, Garcia P, Williams MA. Associations of depression and depressive symptoms with preeclampsia: results from a Peruvian case–control study. BMC Womens Health. 2007;7(1):15. doi: 10.1186/1472-6874-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stevens W, Shih T, Incerti D et al. Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol. 2017;217(3):237–248.e16. doi: 10.1016/j.ajog.2017.04.032. [DOI] [PubMed] [Google Scholar]
- 38.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep. 2018;67(1):1–55. [PubMed] [Google Scholar]
- 39.Paul IM, Downs DS, Schaefer EW, Beiler JS, Weisman CS. Postpartum anxiety and maternal–infant health outcomes. Pediatrics. 2013;131(4):e1218–e1224. doi: 10.1542/peds.2012-2147. [DOI] [PubMed] [Google Scholar]
- 40. The cost of having a baby in the United States. Ann Arbor, MI: Truven Health Analytics; 2013.
- 41. Maternity length of stay rules. Denver, CO: National Conference of State Legislatures; 2018.
- 42.Lancaster CA, Flynn HA, Johnson TRB, Marcus SM, Davis MM. Peripartum length of stay for women with depressive symptoms during pregnancy. J Womens Health (Larchmt). 2010;19(1):31–37. doi: 10.1089/jwh.2009.1383. [DOI] [PubMed] [Google Scholar]
- 43. Healthcare Cost and Utilization Project (HCUP) Fast Stats. November 2017. Rockville, MD: Agency for Healthcare Research and Quality; 2019. [PubMed]
- 44.Food Stamps/Supplemental Nutrition Assistance Program (SNAP) 2017. American Community Survey 1-year estimates. Washington, DC: US Census Bureau; 2017.
- 45.Noonan K, Corman H, Reichman NE. Effects of maternal depression on family food insecurity. Econ Hum Biol. 2016;22:201–215. doi: 10.1016/j.ehb.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 46. National level annual summary: Supplemental Nutrition Assistance Program participation and costs. Silver Spring, MD: US Food and Drug Administration; 2018.
- 47.Trippe C, Tadler C, Johnson P, Giannarelli L, Betson D. National- and state-level estimates of WIC eligibles and WIC program reach in 2015. Washington, DC: US Department of Agriculture, Food and Nutrition Service; 2018.
- 48. US Department of Agriculture, Food and Nutrition Service. WIC program participation and costs. Washington, DC: US Department of Agriculture; 2018.
- 49. Count of women ages 15–44 by race/ethnicity and Medicaid status, United States, 2015. Rockville, MD: Agency for Healthcare Research and Quality; 2018.
- 50. Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group. Health expenditures by state of residence, 1991–2014. Baltimore, MD: Centers for Medicare and Medicaid Services; 2017.
- 51. Medicaid spending per full-benefit enrollee, timeframe: FY2014. Washington, DC: Kaiser Family Foundation; 2019.
- 52. US Department of Health and Human Services. Characteristics and financial circumstances of TANF recipients, fiscal year (FY) 2016. Washington, DC: Office of Family Assistance; 2017.
- 53. Poverty status in the past 12 months of families. 2012–2016 American Community Survey 5-year estimates. Washington, DC: US Census Bureau; 2019.
- 54. US Department of Health and Human Services, Administration for Children and Families, Office of Family Assistance. TANF financial data—FY 2016. Washington, DC: US Department of Health and Human Services; 2018.
- 55. US Department of Health and Human Services, Administration for Children and Families, Office of Family Assistance. TANF caseload data 2016. Washington, DC: US Department of Health and Human Services; 2017.
- 56. Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Vital Statistics. Natality public-use data, 2007–2017. Atlanta, GA: Centers for Disease Control and Prevention; 2019.
- 57.Jarde A, Morais M, Kingston D et al. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73(8):826–837. doi: 10.1001/jamapsychiatry.2016.0934. [DOI] [PubMed] [Google Scholar]
- 58.Behrman RE, Butler AS, editors. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 59. Breastfeeding report card: United States, 2018. Atlanta, GA: Centers for Disease Control and Prevention; 2018.
- 60.Wouk K, Stuebe AM, Meltzer-Brody S. Postpartum mental health and breastfeeding practices: an analysis using the 2010–2011 Pregnancy Risk Assessment Monitoring System. Matern Child Health J. 2017;21(3):636–647. doi: 10.1007/s10995-016-2150-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: a pediatric cost analysis. Pediatrics. 2010;125(5):e1048–e1056. doi: 10.1542/peds.2009-1616. [DOI] [PubMed] [Google Scholar]
- 62. About compressed mortality, 1999–2016. Atlanta, GA: Centers for Disease Control and Prevention; 2019.
- 63.Howard LM, Kirkwood G, Latinovic R. Sudden infant death syndrome and maternal depression. J Clin Psychiatry. 2007;68(8):1279–1283. doi: 10.4088/jcp.v68n0816. [DOI] [PubMed] [Google Scholar]
- 64.Sanderson CA, Cowden B, Hall DMB, Taylor EM, Carpenter RG, Cox JL. Is postnatal depression a risk factor for sudden infant death? Br J Gen Pract. 2002;52(481):636–640. [PMC free article] [PubMed] [Google Scholar]
- 65.Fox M, Cacciatore J, Lacasse JR. Child death in the United States: productivity and the economic burden of parental grief. Death Stud. 2014;38(6-10):597–602. doi: 10.1080/07481187.2013.820230. [DOI] [PubMed] [Google Scholar]
- 66.Bitsko RH, Holbrook JR, Robinson LR et al. Health care, family, and community factors associated with mental, behavioral, and developmental disorders in early childhood—United States, 2011–2012. MMWR Morb Mortal Wkly Rep. 2016;65(9):221–226. doi: 10.15585/mmwr.mm6509a1. [DOI] [PubMed] [Google Scholar]
- 67.O’Donnell KJ, Glover V, Barker ED, O’Connor TG. The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev Psychopathol. 2014;26(2):393–403. doi: 10.1017/S0954579414000029. [DOI] [PubMed] [Google Scholar]
- 68.Beecham J. Annual Research Review: Child and adolescent mental health interventions: a review of progress in economic studies across different disorders. J Child Psychol Psychiatry. 2014;55(6):714–732. doi: 10.1111/jcpp.12216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Nutrition, physical activity, and obesity: data, trends, and maps. Atlanta, GA: Centers for Disease Control and Prevention; 2018.
- 70.Wojcicki JM, Holbrook K, Lustig RH et al. Chronic maternal depression is associated with reduced weight gain in Latino infants from birth to 2 years of age. PLoS One. 2011;6(2):e16737. doi: 10.1371/journal.pone.0016737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Benton PM, Skouteris H, Hayden M. Does maternal psychopathology increase the risk of pre-schooler obesity? A systematic review. Appetite. 2015;87:259–282. doi: 10.1016/j.appet.2014.12.227. [DOI] [PubMed] [Google Scholar]
- 72.Finkelstein EA, Graham WCK, Malhotra R. Lifetime direct medical costs of childhood obesity. Pediatrics. 2014;133(5):854–862. doi: 10.1542/peds.2014-0063. [DOI] [PubMed] [Google Scholar]
- 73. Table 4-1: Current asthma prevalence percents by age, United States: 2016 National Health Interview Survey. Atlanta, GA: Centers for Disease Control and Prevention; 2018.
- 74.Cookson H, Granell R, Joinson C, Ben-Shlomo Y, Henderson AJ. Mothers’ anxiety during pregnancy is associated with asthma in their children. J Allergy Clin Immunol. 2009;123(4):847–853.e11. doi: 10.1016/j.jaci.2009.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Giallo R, Bahreinian S, Brown S, Cooklin A, Kingston D, Kozyrskyj A. Maternal depressive symptoms across early childhood and asthma in school children: findings from a longitudinal Australian population based study. PLoS One. 2015;10(3):e0121459. doi: 10.1371/journal.pone.0121459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sullivan PW, Ghushchyan V, Navaratnam P et al. The national cost of asthma among school-aged children in the United States. Ann Allergy Asthma Immunol. 2017;119(3):246–252.e1. doi: 10.1016/j.anai.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 77. Nonfatal injury reports, 2000–2017. Atlanta, GA: Centers for Disease Control and Prevention; 2019.
- 78.Schwebel DC, Brezausek CM. Chronic maternal depression and children’s injury risk. J Pediatr Psychol. 2008;33(10):1108–1116. doi: 10.1093/jpepsy/jsn046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yamaoka Y, Fujiwara T, Tamiya N. Association between maternal postpartum depression and unintentional injury among 4-month-old infants in Japan. Matern Child Health J. 2016;20(2):326–336. doi: 10.1007/s10995-015-1832-9. [DOI] [PubMed] [Google Scholar]
- 80. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System of the National Center for Injury Prevention and Control. Atlanta, GA: Centers for Disease Control and Prevention; 2019.
- 81.Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2015 emergency department summary tables. 2015. Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2015_ed_web_tables.pdf. Accessed April 7, 2019.
- 82.Flynn HA, Davis M, Marcus SM, Cunningham R, Blow FC. Rates of maternal depression in pediatric emergency department and relationship to child service utilization. Gen Hosp Psychiatry. 2004;26(4):316–322. doi: 10.1016/j.genhosppsych.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 83.Sills MR, Shetterly S, Xu S, Magid D, Kempe A. Association between parental depression and children’s health care use. Pediatrics. 2007;119(4):e829–e836. doi: 10.1542/peds.2006-2399. [DOI] [PubMed] [Google Scholar]
- 84. Emergency room services—mean and median expenses per person with expense and distribution of expenses by source of payment: United States, 2014. Medical Expenditure Panel Survey Household Component Data. Rockville, MD: Agency for Healthcare Research and Quality; 2019.
- 85.Wolf ER, Hochheimer CJ, Sabo RT et al. Gaps in well-child care attendance among primary care clinics serving low-income families. Pediatrics. 2018;142(5):e20174019. doi: 10.1542/peds.2017-4019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Minkovitz CS, Strobino D, Scharfstein D et al. Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- 87. MEPSnet household component for 2015. Rockville, MD: Agency for Healthcare Research and Quality; 2015.
- 88.Shulman HB, D’Angelo DV, Harrison L, Smith RA, Warner L. The Pregnancy Risk Assessment Monitoring System (PRAMS): overview of design and methodology. Am J Public Health. 2018;108(10):1305–1313. doi: 10.2105/AJPH.2018.304563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bartick MC, Schwarz EB, Green BD et al. Suboptimal breastfeeding in the United States: maternal and pediatric health outcomes and costs. Matern Child Nutr. 2017;13(1) doi: 10.1111/mcn.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Diaz JY, Chase R. The cost of untreated maternal depression: St Paul, MN: Wilder Research; 2010.
- 91.Field T, Diego M, Hernandez-Reif M et al. Comorbid depression and anxiety effects on pregnancy and neonatal outcome. Infant Behav Dev. 2010;33(1):23–29. doi: 10.1016/j.infbeh.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ramchandani PG, Psychogiou L, Vlachos H et al. Paternal depression: an examination of its links with father, child and family functioning in the postnatal period. Depress Anxiety. 2011;28(6):471–477. doi: 10.1002/da.20814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wee KY, Skouteris H, Pier C, Richardson B, Milgrom J. Correlates of ante- and postnatal depression in fathers: a systematic review. J Affect Disord. 2011;130(3):358–377. doi: 10.1016/j.jad.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 94. Position statement on screening and treatment of mood and anxiety disorders during pregnancy and postpartum. Washington, DC: American Psychiatric Association; 2018.
- 95. ACOG Committee Opinion No. 630: Screening for perinatal depression. Washington, DC: American College of Obstetricians and Gynecologists; 2015. [DOI] [PubMed]
- 96. Maternal depression screening: Medicaid and EPSDT Coverage. Washington, DC: American Academy of Pediatrics; 2016.
- 97.Association of Women’s Health, Obstetric, and Neonatal Nurses. Mood and anxiety disorders in pregnant and postpartum women. J Obstet Gynecol Neonatal Nurs. 2015;44(5):687–689. [Google Scholar]
- 98.O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(4):388–406. doi: 10.1001/jama.2015.18948. [DOI] [PubMed] [Google Scholar]
- 99.O’Connor E, Senger CA, Henninger ML, Coppola E, Gaynes BN. Interventions to prevent perinatal depression: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(6):588–601. doi: 10.1001/jama.2018.20865. [DOI] [PubMed] [Google Scholar]