Abstract
Objectives. To quantify the number of people in the US who delay medical care annually because of lack of available transportation and to examine the differential prevalence of this barrier for adults across sociodemographic characteristics and patient populations.
Methods. We used data from the National Health Interview Survey (1997–2017) to examine this barrier over time and across groups. We used joinpoint regression analysis to identify significant changes in trends and multivariate analysis to examine correlates of this barrier for the year 2017.
Results. In 2017, 5.8 million persons in the United States (1.8%) delayed medical care because they did not have transportation. The proportion reporting transportation barriers increased between 2003 and 2009 with no significant trends before or after this window within our study period. We found that Hispanic people, those living below the poverty threshold, Medicaid recipients, and people with a functional limitation had greater odds of reporting a transportation barrier after we controlled for other sociodemographic and health characteristics.
Conclusions. Transportation barriers to health care have a disproportionate impact on individuals who are poor and who have chronic conditions. Our study documents a significant problem in access to health care during a time of rapidly changing transportation technology.
The generally poor performance of the US health care system, relative to that of its peer countries, has been well-documented.1 Increasingly, attention has turned to the role of social determinants of health as 1 potential explanatory factor. While there are many demonstrated barriers to health care access including socioeconomic constraints and health literacy limitations, a lack of viable transportation inhibits a patient’s ability to travel to health-promoting institutions like doctors’ offices and pharmacies. Transportation barriers interrupt adherence with medical appointments and can prevent people from seeking care at all. This is challenging for chronic illness management as nonattendance can lead to exacerbation of chronic disease and disease-related outcomes.2,3
An oft-cited study from 2005 estimates that approximately 3.6 million people in the United States miss or delay nonemergency medical treatment every year despite having health care coverage because of lack of transportation to care facilities.4 Thirteen years later, this figure likely underestimates the magnitude of the problem given the suburbanization of poverty, the aging baby boomer population, and the general increase in population. Across the United States, low-density development patterns and lack of public transit coupled with high rates of chronic conditions reinforce this issue.
To update this estimate, we used data from the National Health Interview Survey (NHIS) to conduct a descriptive analysis of the prevalence of transportation barriers to health care in the United States. First, we looked at longitudinal trends in this outcome over time, from 1997 to 2017. Second, we assessed the prevalence of this barrier across demographic groups in 2017. Third, we examined correlates—both health conditions and sociodemographic characteristics—of transportation barriers among the US population.
TRANSPORTATION BARRIERS TO CARE
In a review of 61 studies on transportation barriers to health care, Syed at al. found that transportation barriers are a significant impediment to health care access, especially for those with lower incomes or those who are underinsured or uninsured.5 This population of people, frequently referred to as “transportation-disadvantaged,” often shift their care-seeking to more costly, acute-care settings (e.g., the emergency department [ED]) based on preference or convenience.6–9
Transportation barriers disproportionately affect specific patient groups. Wallace et al. found that individuals carrying the highest burden of disease faced the greatest transportation barriers and were more likely to be older, poorer, less-educated, female, people of color, and people with chronic illnesses or disabilities.4 Probst et al. found that African Americans had higher burdens of travel to health care than did Whites after the authors controlled for mode and socioeconomic status.10 A 2017 survey of health centers found that older patients, patients who are homeless, people with young children, chronically ill patients, public housing residents, people with disabilities, and pregnant women were all reported to be disproportionately negatively affected by transportation barriers.11 Several studies have identified unique transportation barriers for veterans despite the fact that veterans have access to federal health care and some receive transportation service through the Veterans Health Administration.12,13 Another study that used NHIS data from 1997 to 2006 found that American Indian veterans were more likely to delay care because of transportation issues than were White veterans.14
Research suggests that having access to a vehicle is positively associated with the ability to reach health facilities, even after controlling for socioeconomic status.15–17 Vehicle access may be especially important in rural areas, where missed or delayed nonemergency medical treatment is often attributable to lack of access to a vehicle.18 Some studies have found that patients who live in nonurban areas face greater transportation barriers to health care access than do their urban counterparts.10,19,20 Compared with people living in urban areas, rural residents reported longer travel time to see a physician, particularly a specialist.21
Even in urban areas where health care facilities may be closer, low-income neighborhoods often rely on aging transportation infrastructure, unreliable service, or fixed routes with service areas that do not align with medical facility destinations.5 Urban residents may struggle to understand how to access public transit or even how to get to health care when transportation is provided to them.22 This is especially true for people who are obese or chronically ill, or who have a disability, wherein riding the bus or the subway can be physically challenging. For individuals with mobility- or financial-related barriers, there are various specialized transportation options for such trips, including Americans with Disabilities Act (ADA) Paratransit (flexibly routed passenger transportation that supplements fixed-route systems run by public transit agencies) as well as Medicaid’s nonemergency medical transportation, which is a Medicaid benefit that facilitates access to medical services for beneficiaries.
Taken together, there are many possible transportation barriers presenting to rural and urban residents alike, with potentially larger barriers for those of disadvantaged health, social, and economic status that can exacerbate existing health inequities. While current health care transportation services exist, various eligibility requirements (such as individual ADA Paratransit eligibility determination processes set by transit agencies) may prevent these services from being available to some individuals.
IMPACTS OF MISSED CARE
Patients who miss health care appointments experience adverse health outcomes. These include complications of chronic illness, increased hospital readmissions, and disrupted continuity of care.23–27 Appointment nonattendance undermines opportunities for diagnostic testing and early detection of disease.28,29 Transportation barriers affect access to pharmacies and, thus, medication (re)fills and adherence.30–32
Missed appointments also have a negative impact on clinical productivity. Unused clinical space, equipment, and staff time equate to loss of revenue.33 Missed or cancelled appointments also prevent or delay other patients from being able to schedule appointments.34 Because of the fragmented nature of the US health care system (i.e., mix of public and private providers), however, it is very difficult to identify the average rate of missed appointments system-wide and there is great variation depending on the health care site.
Since this 2005 study cited previously, there has been little research to quantify a nationally representative estimate of the population that forgoes medical care because of transportation barriers. It is especially challenging to understand why people miss appointments. This is largely attributable to the fact that health-related data lack sufficient detail on transportation, and transportation data lack sufficient detail on health conditions.
METHODS
We used data from the NHIS to investigate the prevalence of transportation barriers to care in the United States. The NHIS is an annual, cross-sectional survey that monitors a broad range of health topics collected through personal household interviews. The NHIS provides nationally representative estimates of various health status and health care utilization measures among the civilian, noninstitutionalized population since 1957. The National Center for Health Statistics (of the Centers for Disease Control and Prevention) designs the NHIS, and the US Census Bureau is the data collection agent. Because NHIS data are obtained through a complex sample design that involves stratification, clustering, and oversampling of populations of interest, we used appropriate sampling weights in Stata version 13.1 (StataCorp LP, College Station, TX) for all analyses.
We leveraged a particular question asked of the sample adult and child cores: “There are many reasons people delay getting medical care. Have you delayed getting care for any of the following reasons in the past 12 months? . . . you didn’t have transportation?” We examined responses to this question in 3 ways. First, we looked longitudinally from 1997 to 2017 at the weighted proportion of people who delayed medical care because of lack of transportation over time. From each wave of data, we excluded only those respondents who were not asked about transport barriers to care because they were not part of the adult or child samples (n = 1 090 240) or who did not provide a valid answer to this question (n = 6674) leaving a total pooled unweighted sample of 892 235 children and adults across 21 years. We assessed changes in trends over time by using joinpoint regression analysis software, version 4.7.0.0 (US National Cancer Institute, Bethesda, MD). Using the grid search model-fitting method with heteroskedastic errors and a minimum of zero and maximum of 3 joinpoints, the permutation test showed that a model with 2 joinpoints was optimal.
Next, we took an in-depth look at patterns of transportation barriers to care for adults in the year 2017. We evaluated transport-delayed care across various sociodemographic subgroups and for people with various health conditions through bivariate analysis. We conducted omnibus tests of group differences to examine differential rates of this barrier across groups and we report F-statistics as they correct for complex sampling design. Finally, we examined what factors might make someone more likely to report a transportation barrier to care. For the same 2017 adult sample, we specified a binary logistic regression model to look at correlates of this outcome adjusting for age, gender, race, ethnicity, educational attainment, poverty status, insurance status, employment status, and geographic region. It is important to note that respondents answered “yes” to the question of interest if and only if they both needed medical care and did not have transportation to that care. Therefore, respondents who did not seek care in the past 12 months would not report a barrier, which could lead to conservative estimates of this particular barrier to care and contribute to disparities across some demographic characteristics (e.g., if older people seek care more often, they may be more likely to report a barrier to this care).
All analyses accounted for features of the complex sampling strategy of the NHIS, including stratification, clustering, and weights. Unweighted counts, including weighted and unweighted characteristics of the 2017 sample, are available in Table A (available as a supplement to the online version of this article at http://www.ajph.org). We excluded respondents from analysis if they were younger than 18 years (n = 18 054) or if they were missing the outcome of interest (either because they were not asked the question or they did not provide a valid answer; n = 33 552), sociodemographic characteristics (n = 1404), or key health characteristics (n = 175). The final unweighted sample size was 24 947. The majority of the sample was female (54.6%) and non-Hispanic White (70.7%). Nearly 34% of the sample had a bachelor’s degree or higher, while 14% lived below the federal poverty threshold. A quarter of the sample reported being in “excellent” health, a third reported being in “very good” health, and just over a quarter reported being in “good” health. More than one third of the sample had ever had hypertension, and 42% reported a functional limitation because of a health problem.
RESULTS
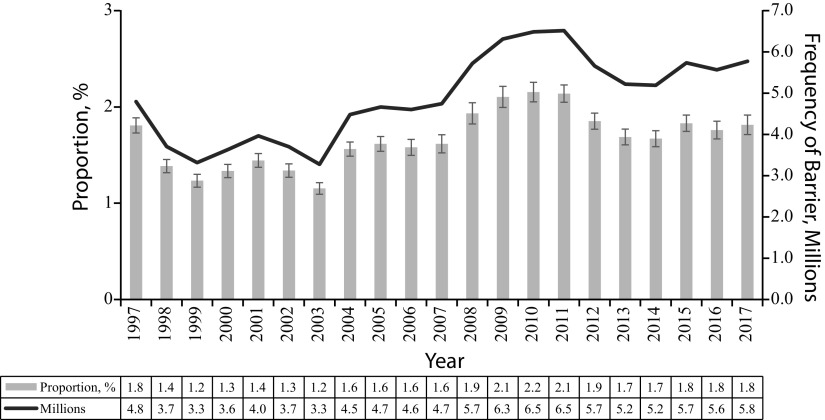
The number of people in the United States who delayed medical care because they did not have transportation grew over time, from 4.8 million in 1997 to 5.8 million in 2017. While the proportion of people of all ages in the United States reporting this barrier was 1.8% in both 1997 and 2017, joinpoint regression analysis showed that this proportion increased at a significant rate from 2003 to 2009 (b = 0.0014; P = .03), but showed no significant trend from 1997 to 2003 or 2009 to 2017. Figure 1 reflects the weighted frequency and proportion of this transportation barrier over time for all ages at the population level.
FIGURE 1—
Transportation Barriers to Health Care: United States, 1997–2017
Note. Annual proportions and frequencies used weighted data. The average annual unweighted sample was 42 487, and the average annual weighted sample was 292 576 684.
Prevalence of Transport Barriers Across Groups
In 2017, 1.9% (95% confidence interval [CI] = 1.7, 2.1) of US adults aged 18 years and older delayed medical care because of a transportation barrier. The prevalence of this barrier to care, along with differences between groups, is shown in Table 1. Overall, 2.2% of women and 1.5% of men reported delaying care because of transportation, and this difference was statistically significant (P < .001). There is variation across age groups; however, the difference between groups is not significant (F = 2.37; P = .08). Rates of transport-delayed care varied significantly across race and ethnicity groups (F = 10.31; P < .001) with non-Hispanic Black respondents reporting the highest rates. Transport barriers to care varied significantly by educational attainment of respondents, with nearly 3% of those with a high-school diploma or less reporting a transport barrier, and only 0.6% of those with a bachelor’s degree or higher reporting the same barrier.
TABLE 1—
Prevalence and Group Differences of Transportation Barriers to Care Among US Adults: 2017
| % (95% CI) | F | P | |
| Overall population of adults | 1.9 (1.7, 2.1) | . . . | . . . |
| Sociodemographics | |||
| Gender | 12.77 | < .001 | |
| Female (52%) | 2.2 (2.0, 2.6) | ||
| Male (48%) | 1.5 (1.2, 1.8) | ||
| Age group, y | 2.37 | .08 | |
| 18–44 | 1.7 (1.4, 2.0) | ||
| 45–64 | 2.2 (1.8, 2.6) | ||
| 65–74 | 1.7 (1.3, 2.2) | ||
| ≥ 75 | 1.8 (1.3, 2.4) | ||
| Race/ethnicity | 10.31 | < .001 | |
| Hispanic | 2.7 (2.1, 3.6) | ||
| Non-Hispanic White | 1.5 (1.3, 1.7) | ||
| Non-Hispanic Black | 3.0 (2.3, 3.7) | ||
| Non-Hispanic Asian, multiracial, or other | 1.8 (1.2, 2.7) | ||
| Educational attainment | 37.82 | < .001 | |
| ≤ high school | 2.7 (2.4, 3.2) | ||
| Some college | 2.2 (1.8, 2.7) | ||
| ≥ bachelor’s degree | 0.6 (0.5, 0.9) | ||
| Family income, $ | 61.36 | < .001 | |
| 0–34 999 | 4.8 (4.3, 5.4) | ||
| 35 000–74 999 | 1.1 (0.8, 1.4) | ||
| 75 000–99 999 | 0.6 (0.3, 1.5) | ||
| ≥ 100 000 | 0.5 (0.3, 0.8) | ||
| Below poverty levela | 7.0 (6.0, 8.2) | 305.32 | < .001 |
| Medicaid | 5.6 (4.8, 6.6) | 229.04 | < .001 |
| No health insurance | 2.6 (1.9, 3.6) | 5.56 | .019 |
| Unemployed | 4.5 (3.1, 6.5) | 24.64 | < .001 |
| Veteran status | 1.3 (1.0, 1.9) | 4.27 | .039 |
| Region | 4.18 | .006 | |
| Northeast | 1.1 (0.8, 1.5) | ||
| North Central or Midwest | 2.1 (1.7, 2.7) | ||
| South | 2.1 (1.8, 2.5) | ||
| West | 1.8 (1.4, 2.3) | ||
| Health | |||
| Self-reported health status | 107.12 | < .001 | |
| Excellent | 0.8 (0.5, 1.1) | ||
| Very good | 0.9 (0.6, 1.2) | ||
| Good | 1.8 (1.5, 2.2) | ||
| Fair | 5.8 (4.8, 7.0) | ||
| Poor | 11.6 (9.1, 14.6) | ||
| Currently pregnant | 0.6 (0.1, 2.5) | 2.75 | .10 |
| Diabetes or prediabetes | 3.8 (3.1, 4.6) | 48.91 | < .001 |
| Asthma | 3.5 (2.8, 4.2) | 42.93 | < .001 |
| Ever told have cancer | 1.9 (1.4, 2.5) | 0.01 | .93 |
| Heart condition or disease | 3.7 (2.8, 4.8) | 24.62 | < .001 |
| Hypertension | 3.0 (2.6, 3.5) | 56.71 | < .001 |
| Weak or failing kidneys | 7.1 (4.9, 10.3) | 54.89 | < .001 |
| Ever had stroke | 6.9 (5.0, 9.5) | 74.54 | < .001 |
| Functional limitation | 3.7 (3.2, 4.2) | 141.31 | < .001 |
| No. of ER/ED visits in past 12 mo | 147.34 | < .001 | |
| 0 | 1.3 (1.1, 1.5) | ||
| 1–3 | 3.6 (3.0, 4.4) | ||
| ≥ 4 | 11.9 (9.3, 15.2) | ||
Note. CI = confidence interval; ER/ED = emergency room/emergency department. Proportions reflect weighted prevalence estimates. The unweighted sample size for 2017 was 24 947.
To determine poverty status, the National Health Interview Survey compares reported total family income with the US Census Bureau’s poverty thresholds for the year in question (2017). These thresholds are based not only on income but also on family size and the number of children younger than 18 years.
Poorer people were more likely to report transport-delayed care, with 7% of those living below the federal poverty threshold, according to the US Census Bureau in 2017, and 5.6% of those receiving Medicaid doing so in 2017. Transportation barriers also varied by employment status (F = 24.64; P < .001), with 4.5% of unemployed people reporting transport-delayed care. There was also significant variation in this barrier across census regions (F = 4.18; P = .01), with people in the Midwest and South reporting transportation barriers more often than those in the Northeast and West.
Rates of transport-delayed care varied with self-reported health status (F = 107.12; P < .001). Among those in “poor” health, 11.6% reported delaying care because of lack of transportation, while less than 1% of those in “excellent” health reported the same. Among health conditions we examined, people with weak or failing kidneys or those with a history of stroke had the highest rates of transport-delayed care in 2017, at 7.1% and 6.9%, respectively. Transport barriers varied significantly across ED utilization. People who made zero visits to the ED in the past year reported lower rates of transport barriers compared with the national level (1.3% compared with 1.9%, respectively), while those who made 4 or more ED visits reported transport barriers at a rate of 11.9%.
Correlates of Transport Barriers to Care
Results of the logistic regression are displayed in Table 2. Adjusted odds ratios (AORs) with their 95% CIs are presented along with the average marginal effect of each variable.
TABLE 2—
Correlates of Transportation Barriers to Care Among US Adults in 2017
| Covariate | AOR (95% CI) | Average Differential Effecta |
| Sociodemographics | ||
| Female | 1.18 (0.90, 1.55) | 0.003 |
| Age group, y | ||
| 18–44 (Ref) | 1 | . . . |
| 45–64 | 0.82 (0.59, 1.14) | −0.004 |
| 65–74 | 0.62 (0.42, 0.92) | −0.008 |
| ≥ 75 | 0.48 (0.31, 0.73) | −0.011 |
| Race/ethnicity | ||
| Non-Hispanic White (Ref) | 1 | . . . |
| Hispanic | 1.54 (1.08, 2.20) | 0.008 |
| Non-Hispanic Black | 1.09 (0.80, 1.49) | 0.001 |
| Non-Hispanic Asian, multiracial, or other | 1.2 (0.79, 1.98) | 0.004 |
| Educational attainment | ||
| High school or less (Ref) | 1 | . . . |
| Some college | 1.27 (0.98, 1.67) | 0.004 |
| Bachelor’s degree or higher | 0.75 (0.50, 1.13) | −0.004 |
| Family income, $ | ||
| 0–34 999 (Ref) | 1 | . . . |
| 35 000–74 999 | 0.47 (0.33, 0.68) | −0.013 |
| 75 000–99 999 | 0.34 (0.15, 0.79) | −0.016 |
| ≥ 100 000 | 0.38 (0.23, 0.63) | −0.015 |
| Below poverty levelb | 1.67 (1.28, 2.18) | 0.009 |
| Medicaid | 1.60 (1.17, 2.20) | 0.009 |
| No health insurance | 1.24 (0.84, 1.84) | 0.004 |
| Unemployed | 1.54 (0.97, 2.43) | 0.009 |
| Veteran status | 0.82 (0.55, 1.22) | −0.003 |
| Region | ||
| Northeast (Ref) | 1 | . . . |
| North Central or Midwest | 1.93 (1.26, 2.95) | 0.010 |
| South | 1.61 (1.12, 2.33) | 0.007 |
| West | 1.49 (0.97, 2.30) | 0.006 |
| Health | ||
| Self-reported health status | ||
| Poor | 2.92 (1.59, 5.36) | 0.023 |
| Fair | 2.30 (1.38, 3.83) | 0.016 |
| Good | 1.16 (0.71, 1.89) | 0.002 |
| Very good | 0.93 (0.56, 1.55) | −0.001 |
| Excellent (Ref) | 1 | . . . |
| Currently pregnant | 0.21 (0.05, 0.92) | −0.014 |
| Diabetes or prediabetes | 1.02 (0.78, 1.33) | 0.000 |
| Asthma | 1.18 (0.91, 1.54) | 0.003 |
| Ever told have cancer | 0.77 (0.56, 1.07) | −0.004 |
| Heart condition or disease | 1.13 (0.75, 1.71) | 0.002 |
| Hypertension | 1.20 (0.92, 1.56) | 0.003 |
| Weak or failing kidneys | 1.34 (0.87, 2.04) | 0.005 |
| Ever had stroke | 1.48 (1.02, 2.16) | 0.008 |
| Functional limitation | 2.58 (1.75, 3.82) | 0.015 |
| No. of ER/ED visits in last 12 mo | ||
| 0 (Ref) | 1 | . . . |
| 1–3 | 1.47 (1.12, 1.94) | 0.007 |
| ≥ 4 | 2.41 (1.63, 3.56) | 0.019 |
Note. AOR = adjusted odds ratio; CI = confidence interval; ER/ED = emergency room/emergency department. Analysis accounted for features of complex sampling strategy including stratification, clustering, and weights. The unweighted sample size for 2017 was 24 947.
The average marginal effect (or “differential effect” for categorical variables) is the average change in the predicted probability of reporting a transportation barrier by a unit increase in the variable of interest (or by a relative change from the reference category for categorical variables).
To determine poverty status, the National Health Interview Survey compares reported total family income with the US Census Bureau’s poverty thresholds for the year in question (2017). These thresholds are based not only on income but also on family size and the number of children younger than 18 years.
Women’s predicted probability of delaying care because of a transport barrier was 0.3 percentage points higher than it was for men after we controlled for other sociodemographic and health factors; however, this difference was not statistically significant (P = .22). A person older than 75 years had a 1.1-percentage-point decrease in the predicted probability of delaying care because of lack of transportation compared with a person aged 18 to 44 years with otherwise similar characteristics (P < .001).
Hispanic people had 1.5 times the odds of having a transportation barrier to care compared with non-Hispanic Whites after we controlled for other sociodemographic and health characteristics (P = .02). Those who lived below the poverty threshold were more likely to report a transport barrier than were those above the threshold (AOR = 1.7; P < .001) and Medicaid beneficiaries were more likely to report the barrier than were their peers who did not receive Medicaid (AOR = 1.6; P < .001). People who were unemployed were more likely to report the barrier than people with similar characteristics who may be employed or who were not in the labor force, though the strength of the association was not significant (AOR = 1.5; P = .07). Compared with people living in the Northeast, people in the Midwest and South regions of the United States had 1.9 and 1.6 times the odds, respectively, of delaying care because of this barrier (P < .001 and P = .01, respectively).
Self-reporting “poor” health, on average, was associated with a 2.3-percentage-point increase in the predicted probability of transport-delayed care compared with self-reporting “excellent” health (P < .001). After we accounted for sociodemographic and other health characteristics, people with a history of stroke were more likely to report a transport barrier to care (AOR = 1.5; P = .04) as were people with a functional limitation (AOR = 2.6; P < .001). Compared with people who had zero ED visits in a year, those who made 1 to 3 visits had 1.5 times the odds of delaying care because of lack of transportation, and those who made 4 or more visits had 2.4 times the odds (P = .01 and P < .001, respectively).
DISCUSSION
We estimate that 5.8 million people in the United States delayed medical care because of a lack of available transportation in 2017. Our estimate provides an update to the limited amount of published literature quantifying the population affected by this barrier to care on a nationally representative scale.
Consistent with previous research,4 we found that people with lower incomes, especially those living below the poverty threshold, were more likely to report a transport barrier to care. Similarly, we found that racial and ethnic minorities reported higher rates of this barrier compared with non-Hispanic Whites; however, the association remained significant only for Hispanics after we controlled for other sociodemographic and health characteristics. The same is true for educational attainment and gender, for which we found no significant association with transport barriers after we controlled for these other factors.
Unlike previous research,4,11 we found a negative association between age and rates of transport-delayed care, such that older people were less likely to report a transport barrier to care in our study year. Though the magnitude of the negative association was rather small, we posit that this may be attributable to other explanatory variables in our model.
Importantly, we found a strong association between functional limitation status and transport-delayed care above and beyond any sociodemographic or other health characteristics (AOR = 2.6; P < .001). Almost half of our sample (42%) reported a functional limitation—indicating that they have difficulty doing specific activities because of a health problem, including things like going out shopping, walking a quarter mile (or 3 city blocks), or lifting something that weighs 10 pounds. This measure is not wholly representative of a physical disability, but it likely reflects important nuance in the way that we account for mobility independence and (in)ability to travel outside of the home. Interestingly, despite Medicaid’s mandatory nonemergency medical transportation benefit, we found that Medicaid beneficiaries were more likely to report a transportation barrier to care in 2017 compared with those who did not receive Medicaid.
Our findings regarding ED utilization are noteworthy, as visits to such acute care settings are highly costly. Within our sample, 1.3% of adults with zero ED visits reported transport-delayed care while a stark 12% of those with 4 or more visits per year reported the same. While there is no way to tease out the temporal sequence in which these events occur for each respondent—that is, whether transportation barriers lead to increases in ED use or high-frequency users are more likely to report barriers—the association is compelling as insurance companies are perpetually interested in abating the high costs of high-utilizing, frequent visitors to the ED.
Limitations
It is likely that our estimate of the number of persons in the United States who delay medical care because of lack of transportation is a conservative one. Any sampling biases arising from the NHIS carry over to our estimate; for example, there is often nonresponse of those who are poor, homeless, and in very poor health, and the NHIS excludes Native Americans living on reservations who are part of the Indian Health Service.4 Our estimate is potentially further downwardly biased because the outcome of interest was only partially observable, such that even though all respondents in the sample were asked this question, we did not observe affirmative outcomes (i.e., presence of transportation barriers) for people who did not seek care in the past 12 months. This is a limitation of how the construct is measured in this data set—by answering “yes” or “no” to just 1 question about transportation barriers to care rather than assessing whether people needed care but could not access it.
This analysis was limited by the lack of geographic information available within the publicly available NHIS data set. Census region was the only place-based variable; with more detailed information about respondents’ residence, we could learn more about implications of distance to care facilities, transportation mode availability, and potential transportation barrier differences between urban and nonurban dwellers.
Public Health Implications
Lack of transportation delays medical care for millions of US persons every year, with this number nearing 6 million in 2017. There is a separate and robust literature that describes how increased patient access to routine and preventive care leads to improved overall health outcomes as well as avoidance of costly ambulance bills and ED visits. For many people, driving oneself, getting a ride from friends or family, or taking public transportation are viable modal options to travel to medical appointments. For individuals with mobility- or financial-related barriers, such as lack of a personal vehicle, there are various specialized transportation options for these trips, such as paratransit options that include demand-responsive buses, van services, hospital- and care provider–based shuttles, and vehicles for hire including livery vehicles and taxis.
These trips can be covered by nonemergency medical transportation—the mandatory benefit of Medicaid and supplementary benefit of some Medicare Advantage plans.1 The Veterans Administration offers mileage reimbursement and transportation services for disabled veterans that meet qualifying criteria, and some accountable care organizations, who receive bonuses for meeting quality and cost targets while incurring penalties for falling short of targets, provide beneficiaries with transportation—recognizing it as a social determinant of health. Even with these various current offerings, however, our finding that nearly 2% of the population reports transport-delayed care is evidence that current transportation options do not work for a large number of people.
Our study documents a significant problem in access to health care during a time of rapid change in transportation technology. The United States has seen a proliferation of new mobility solutions in recent years, and ride-sourcing services have been proposed as an alternative to nonemergency medical transportation.35 These new services promise cost-saving potential for insurers, reduced no-shows, increased treatment adherence, greater bed turnover for health care providers, and more reliable access for patients; however, it is unclear whether these services could be financially viable in low-density, nonurban areas. There is a need for further research on transportation barriers to care that is more nuanced in relation to various health conditions and patient populations and that incorporates greater place-based information. With additional research, transportation solutions can be tailored to target patients by geographic region or by diagnosis.
ACKNOWLEDGMENTS
This work was supported by the Southeastern Transportation Research, Innovation, Development and Education (STRIDE) Center at the University of Florida. The STRIDE Center is funded through the US Department of Transportation’s University Transportation Centers Program.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This project was exempted by the University of North Carolina at Chapel Hill’s institutional review board (IRB 19-1604).
Footnotes
See also Henning-Smith, p. 763.
REFERENCES
- 1.Osborn R, Doty MM, Moulds D, Sarnak DO, Shah A. Older Americans were sicker and faced more financial barriers to health care than counterparts in other countries. Health Aff (Millwood) 2017;36(12):2123–2132. doi: 10.1377/hlthaff.2017.1048. [DOI] [PubMed] [Google Scholar]
- 2.Murdock A, Rogers C, Lindsay H, Tham T. Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. J R Soc Med. 2002;95:284–286. doi: 10.1258/jrsm.95.6.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karter AJ, Parker MM, Moffet HH et al. Missed appointments and poor glycemic control: an opportunity to identify high‐risk diabetic patients. Med Care. 2004;42(2):110–115. doi: 10.1097/01.mlr.0000109023.64650.73. [DOI] [PubMed] [Google Scholar]
- 4.Wallace R, Hughes-Cromwick P, Mull H, Khasnabis S. Access to health care and nonemergency medical transportation: two missing links. Transp Res Rec. 2005;1924(1):76–84. [Google Scholar]
- 5.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood) 2013;32(7):1196–1203. doi: 10.1377/hlthaff.2012.0825. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen DL, Dejesus RS. Increased frequency of no-shows in residents’ primary care clinic is associated with more visits to the emergency department. J Prim Care Community Health. 2010;1(1):8–11. doi: 10.1177/2150131909359930. [DOI] [PubMed] [Google Scholar]
- 8.Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med. 2017;24(9):1137–1149. doi: 10.1111/acem.13220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hwang AS, Atlas SJ, Cronin P et al. Appointment “no-shows” are an independent predictor of subsequent quality of care and resource utilization outcomes. J Gen Intern Med. 2015;30(10):1426–1433. doi: 10.1007/s11606-015-3252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Probst JC, Laditka SB, Wang JY, Johnson AO. Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US National Household Travel Survey. BMC Health Serv Res. 2007;7(1):40. doi: 10.1186/1472-6963-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Health Outreach Partners. Rides to Wellness community scan project. 2017. Available at: https://outreach-partners.org/wp-content/uploads/2017/06/FTA-Comm-Profiles-2.pdf. Accessed January 27, 2018.
- 12.Zullig LL, Jackson GL, Provenzale D, Griffin JM, Phelan S, Van Ryn M. Transportation—a vehicle or roadblock to cancer care for VA patients with colorectal cancer? Clin Colorectal Cancer. 2012;11(1):60–65. doi: 10.1016/j.clcc.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Washington DL, Bean-Mayberry B, Riopelle D, Yano EM. Access to care for women veterans: delayed healthcare and unmet need. J Gen Intern Med. 2011;26(suppl 2):655–661. doi: 10.1007/s11606-011-1772-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson PJ, Carlson KF, Hearst MO. Healthcare disparities for American Indian veterans in the United States: a population-based study. Med Care. 2010;48(6):563–569. doi: 10.1097/MLR.0b013e3181d5f9e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guidry JJ, Aday LA, Zhang D, Winn RJ. Transportation as a barrier to cancer treatment. Cancer Pract. 1997;5(6):361–366. [PubMed] [Google Scholar]
- 16.Yang S, Zarr RL, Kass-Hout TA, Kourosh A, Kelly NR. Transportation barriers to accessing health care for urban children. J Health Care Poor Underserved. 2006;17(4):928–943. doi: 10.1353/hpu.2006.0137. [DOI] [PubMed] [Google Scholar]
- 17.Silver D, Blustein J, Weitzman BC. Transportation to clinic: findings from a pilot clinic-based survey of low-income suburbanites. J Immigr Minor Health. 2012;14(2):350–355. doi: 10.1007/s10903-010-9410-0. [DOI] [PubMed] [Google Scholar]
- 18.Arcury TA, Preisser JS, Gesler WM, Powers JM. Access to transportation and health care utilization in a rural region. J Rural Health. 2005;21(1):31–38. doi: 10.1111/j.1748-0361.2005.tb00059.x. [DOI] [PubMed] [Google Scholar]
- 19.Skinner AC, Slifkin RT. Rural/urban differences in barriers to and burden of care for children with special health care needs. J Rural Health. 2007;23(2):150–157. doi: 10.1111/j.1748-0361.2007.00082.x. [DOI] [PubMed] [Google Scholar]
- 20.Henning-Smith C, Evenson A, Corbett A, Kozhimannil K, Moscovice I. Rural transportation: challenges and opportunities. University of Minnesota Rural Health Research Center. November 2017. Available at: https://rhrc.umn.edu/wp-content/uploads/2019/01/1518734252UMRHRCTransportationChallenges.pdf. Accessed May 16, 2019.
- 21.Reschovsky JD, Staiti AB. Access and quality: does rural America lag behind? Health Aff (Millwood) 2005;24(4):1128–1139. doi: 10.1377/hlthaff.24.4.1128. [DOI] [PubMed] [Google Scholar]
- 22.Wizemann T, Baciu A, editors. Exploring Data and Metrics of Value at the Intersection of Health Care and Transportation. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 23.Murray M, Berwick DM. Advanced access: reducing waiting and delays in primary care. JAMA. 2003;289(8):1035–1040. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- 24.Salameh E, Olsen S, Howard D. Nonattendance with clinic follow-up appointments: diabetes as exemplar. J Nurse Pract. 2012;8(10):797–803. [Google Scholar]
- 25.Karter AJ, Parker MM, Moffet HH et al. Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care. 2004;42(2):110–115. doi: 10.1097/01.mlr.0000109023.64650.73. [DOI] [PubMed] [Google Scholar]
- 26.Schectman JM, Schorling JB, Voss JD. Appointment adherence and disparities in outcomes among patients with diabetes. J Gen Intern Med. 2008;23(10):1685–1687. doi: 10.1007/s11606-008-0747-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hernandez AF, Greiner MA, Fonarow GC et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 28.Weingarten N, Meyer DL, Schneid JA. Failed appointments in residency practices: who misses them and what providers are most affected? J Am Board Fam Pract. 1997;10(6):407–411. [PubMed] [Google Scholar]
- 29.Siminoff LA, Hausmann LRM, Ibrahim S. Barriers to obtaining diagnostic testing for coronary artery disease among veterans. Am J Public Health. 2008;98(12):2207–2213. doi: 10.2105/AJPH.2007.123224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levine DA, Kiefe CI, Howard G, Howard VJ, Williams OD, Allison JJ. Reduced medication access: a marker for vulnerability in US stroke survivors. Stroke. 2007;38(5):1557–1564. doi: 10.1161/STROKEAHA.106.478545. [DOI] [PubMed] [Google Scholar]
- 31.Welty TE, Willis SL, Welty EA. Effect of limited transportation on medication adherence in patients with epilepsy. J Am Pharm Assoc (2003) 2010;50(6):698–703. doi: 10.1331/JAPhA.2010.09081. [DOI] [PubMed] [Google Scholar]
- 32.Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008;83(5):529–535. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- 33.Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2016;16(1):13. doi: 10.1186/s12913-015-1243-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crutchfield TM, Kistler CE. Getting patients in the door: medical appointment reminder preferences. Patient Prefer Adherence. 2017;11:141–150. doi: 10.2147/PPA.S117396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaiyachati KH, Hubbard RA, Yeager A et al. Association of rideshare-based transportation services and missed primary care appointments: a clinical trial. JAMA Intern Med. 2018;178(3):383–389. doi: 10.1001/jamainternmed.2017.8336. [DOI] [PubMed] [Google Scholar]