Abstract
Objectives. To examine indoor tanning trends among US adults, and the relation to indoor tanning youth access legislation.
Methods. This study analyzed the Health Information National Trends Survey (HINTS), a mailed survey, from the years 2007, 2011, 2013, 2014, 2017, and 2018 (combined n = 20 2019).
Results. Indoor tanning prevalence decreased significantly over time among all US adults from 2007 (10%) to 2018 (4%; P < .001), among young adults aged 18 to 34 years (14% to 4%; P < .001), and among both women (14% to 4%; P < .001) and men (5% to 4%; P < .05). Indoor tanning significantly decreased in states that enacted youth access legislation by 2018, but did not significantly decrease for other states. Frequent indoor tanning was common in 2018; about one quarter of respondents who reported any indoor tanning did so 25 times or more in the past year.
Conclusions. This study identifies several challenges in continuing to reduce indoor tanning in the United States. Youth access legislation may be effective for reducing tanning among the broader population of tanners; however, there remains a need for focus on highly frequent tanners, as well as men.
Approximately 5.4 million cases of skin cancer are diagnosed per year.1 Melanoma, the most deadly form of skin cancer, led to 9000 deaths in the United States in 2018.1 Incidence rates of melanoma in the United States have been rising for several decades and continue to rise.2,3 Ultraviolet radiation exposure, from outdoor sun exposure or artificial sources such as indoor tanning, is the main cause of most skin cancers.4–6
Indoor tanning—the intentional use of tanning beds or lamps to achieve a tan—is a major risk factor for the most common types of skin cancer: melanoma, basal cell carcinoma, and squamous cell carcinoma.7 In general, indoor tanners tend to be young, female, and non-Hispanic White.8,9 Of concern, indoor tanning before the age of 30 years is associated with developing melanoma at a young age,10,11 and about a third of indoor tanners begin tanning before the age of 18 years.12 In 2014, the Surgeon General’s Call to Action to Prevent Skin Cancer identified the need to reduce indoor tanning for skin cancer prevention.13 As such, young people are a key target group for indoor tanning reduction interventions, including age-restrictive legislation for indoor tanning facilities.
Indoor tanning rates are declining in the United States. Among adults, the trend has been examined from 2010 to 2015, during which indoor tanning prevalence significantly declined among both men and women.14 Understanding the factors related to this downward trend could galvanize enhanced prevention and cessation efforts. Potential explanations might include that implementation of state-level indoor tanning youth access legislation has been steadily increasing in recent years. Beginning in 2012 (with modal years of 2013–2014),15 43 states and Washington, DC, have passed legislation to regulate and restrict indoor tanning for older adolescents; this legislation included prohibition of indoor tanning for all minors younger than 18 years (15 states and the District of Columbia), prohibition of tanning for minors younger than 14 through 16 years (12 states), and requirement of parental permission or accompaniment to tanning for those aged younger than 14 through 17 years (16 states).15 Yet the relation between state legislation and indoor tanning prevalence is not well known and has not been examined for adult populations. To date, indoor tanning bans and other restrictive legislation pertain only to minors.
It is possible that these types of legislation may affect the wider community of indoor tanners. The Social Amplification of Risk Framework16 posits a theoretical approach to understanding how risk information may be amplified by factors such as media exposure. The passing of state legislation, coupled with corresponding media coverage of that legislation, could potentially act as a “risk signal”—for example, that indoor tanning is dangerous enough to be restricted for minors—which is then amplified as it passes through multiple information channels and social networks, such as parents, physicians, and both the traditional and social media. The consistency and volume of such information further amplify public risk perceptions. As such, social amplification of risk may explain a potential “spillover” effect of indoor tanning youth access legislation into the indoor tanning behavior of adults, leading to risk information being shared more broadly.
Existing research showing declining indoor tanning prevalence are positive developments; however, adult indoor tanning prevalence has not yet been reported using longer-term data, which could demonstrate a more complete picture of the indoor tanning public health problem. Through use of available longer-term data, including a snapshot of years preceding modern indoor tanning regulations and laws, a fuller picture of the indoor tanning public health problem can be demonstrated. The present study uses nationally representative, cross-sectional data from 6 time points over 11 years from the Health Information National Trends Survey (HINTS) to examine patterns of indoor tanning and other potentially associated variables among US adults. The study aims were (1) to examine indoor tanning prevalence from 2007 to 2018 (a) in the general population, (b) among those aged 18 to 34 years, (c) by gender, and (d) by tanning frequency, and (2) to examine the potential relationship between indoor tanning youth access legislation—the majority of which was enacted during the study period—and indoor tanning prevalence over time to consider the potential spillover effects of this legislation on adults.
METHODS
We obtained data from 6 cycles of HINTS, which is administered by the National Cancer Institute (NCI). HINTS measured indoor tanning frequency during several cycles, including HINTS 3 (2007), HINTS 4-Cycle 1 (2011), HINTS 4-Cycle 3 (2013), HINTS 4-Cycle 4 (2014), HINTS 5-Cycle 1 (2017), and HINTS 5-Cycle 2 (2018), all of which are included in this study. During HINTS 3, the survey transitioned to a paper mode that used random address sampling; the NCI simultaneously administered a telephone survey to a separate sample using random digit dialing. In this study, we utilized only samples using paper mode data collection modes; we excluded the telephone mode sample from HINTS 3 (n = 4092) because of detected mode differences such that the telephone sample reported a significantly lower prevalence of indoor tanning.
Variables
We examined indoor tanning in each of the 6 cycles. In the first 5 cycles, we used 1 item that asked, “How many times in the past 12 months have you used a tanning bed or booth?”; responses were categorized as “0 times,” “1 to 2 times,” “3 to 10 times,” “11 to 24 times,” and “25 or more times.” The last cycle (HINTS 5-Cycle 2) used an open response. We obtained data representing 2018 indoor tanning youth access legislation from the National Conference of State Legislatures.15 We coded each state according to the legislation enacted prior to the most recent HINTS data collection (January 2018), such that “under-18 access ban” was coded as 2 (16 states), “other youth access restrictions” was coded as 1 (28 states), and “no restriction” was coded as 0 (7 states). “Under-18 access ban” refers to exclusion of all individuals aged younger than 18 years from using indoor tanning; “other youth access restrictions” refers to parental permission or accompaniment requirements for various ages younger than 18 years, or access bans for some minors younger than 17 years (commonly ages 13–16 years); “no restrictions” refers to a state that has no such legislation for indoor tanning. We used these codes to assign participants to mutually exclusive groups to represent legislation categories for analysis rather than using individual states’ estimates.
Analytic Approach
We used percentages from weighted frequency calculations to describe indoor tanning prevalence overall and by cycle year. We used the Wald χ2 test to assess group differences (the Mantel–Haenszel test may also have been appropriate but was not available as a procedure that incorporated survey weights). We used linear regression to test for significant differences in prevalence over time: overall (including all years), within strata (e.g., ages 18–34 years and women), by the potential moderator of legislation category, and—for under-18 legislation for which dates were available—legislation implementation dates. We linked sampling weights (50 replicate weights, calculations, and procedure described elsewhere17) to each individual, then combined data into 1 final data set, with each cycle’s samples labeled.18 We tested nonlinear patterns with Joinpoint Version 4.7.0.0 (Bethesda, MD: Statistical Research and Applications Branch, NCI), an analysis program that tests for the fit of multisegmented line patterns. The unit of analysis was the individual participant level. We coded missing data as such and excluded them. We primarily used SAS version 9.4 programming (SAS Institute, Cary, NC) for analysis to account for sample weighting; all data reported are weighted and therefore representative of the US noninstitutionalized adult population.
RESULTS
The results of the 2 study aims are as follows.
Indoor Tanning Prevalence from 2007 to 2018
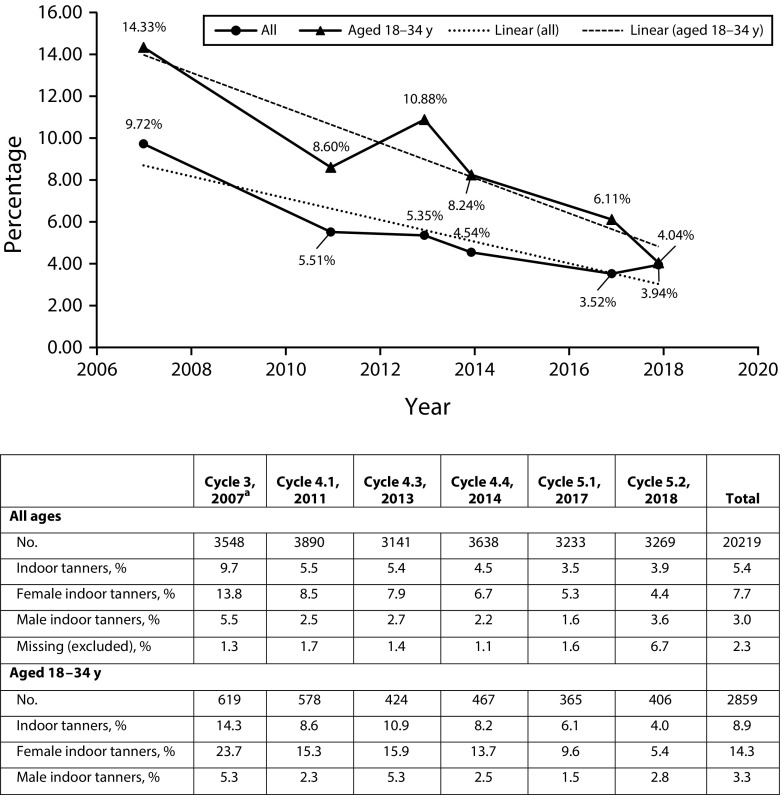
Weighted percentages of those reporting indoor tanning in the past 12 months in the general sample and among those aged 18 to 34 years are reported in Figure 1. In the general sample, for each measured year through 2017, the prevalence of indoor tanning decreased, falling from about 9.7% in 2007 to 3.9% in 2018. The linear regression model for indoor tanning over time from 2007 to 2018 demonstrated a significant decrease (P < .001; Table 1). The Joinpoint analysis did not detect a nonlinear trend. Women (51% of the population) reported higher levels of indoor tanning than men in each cycle, accounting for an average of 73% of tanners overall (P < .001). In 2007, 13.8% of women reported past-year indoor tanning; by 2018, only 4.4% did (Figure 1), with linear regression indicating a significant reduction over time (P < .001). For men, 5.4% reported indoor tanning in 2007 and 3.6% in 2018 (Figure 1); linear regression indicated a significant reduction over time (P < .05).
FIGURE 1—
Past-Year Indoor Tanning Prevalence Among US Adults: Health Information National Trends Survey (HINTS), United States, 2007–2018
Note. Includes at least 1 reported incident of indoor tanning. Percentages are weighted.
aHINTS Cycle 3 includes only the address sample.
TABLE 1—
Regression Results for US Adult Indoor Tanning (IT) Over Time by Type of Youth Access Legislation: Health Information National Trends Survey, United States, 2007–2018
| Parameter | Weighted Estimate (95% CI; SE) | IT Prevalence, % |
| Under-18 access ban | 5.1 | |
| Survey year | −0.005 (−0.007, −0.002; 0.001) | |
| Year legislation enacted | 0.012 (−0.001, 0.025; 0.006) | |
| Other youth access restrictions | 5.3 | |
| Survey year | −0.006 (−0.007, −0.004; 0.001) | |
| No youth access restrictions or bans | 7.4 | |
| Survey year | −0.002 (−0.008, 0.004; 0.003) | |
| All states | 5.4 | |
| Survey year | −0.005 (−0.007, −0.004; 0.001) | |
Note. CI = confidence interval.
Among participants aged 18 to 34 years, indoor tanning prevalence decreased in 2011, 2014, 2017, and 2018, with an overall downward trend from 14.3% in 2007 to 4.0% in 2018 (Figure 1). The linear regression model for a decrease among those aged 18 to 34 years from 2007 to 2018 was significant (P < .001). Female participants aged 18 to 34 years reported higher levels of indoor tanning than their male counterparts: although they accounted for only 51% of that age group, female participants accounted for an average of 82% of tanners aged 18 to 34 years (P < .001). In 2007, 23.7% of women aged 18 to 34 years reported past-year indoor tanning; by 2018, this figure decreased to 5.4% (P < .001). For men aged 18 to 34 years, 5.3% reported indoor tanning in 2007 and 2.8% in 2018, but the difference was not statistically significant (P = .16; Figure 1).
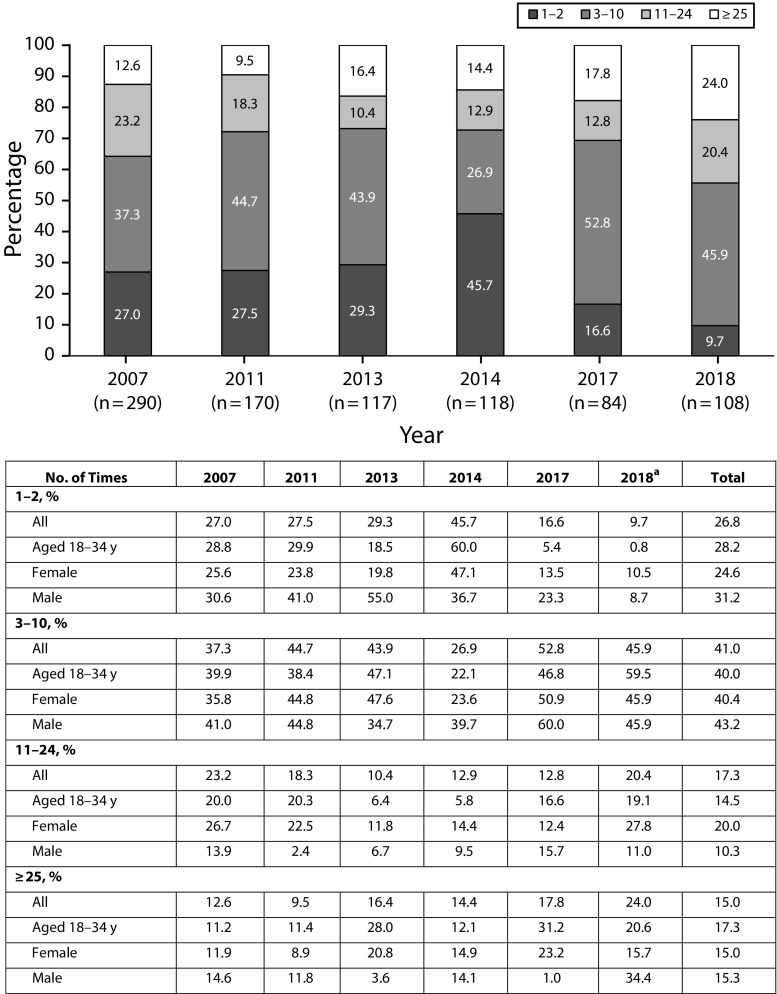
The frequency of tanning reported by indoor tanners in each cycle is reported in Figure 2. In all cycles except 2014, 3 to 10 times per year was the modal frequency. Indoor tanning frequency did not significantly differ by cycle (P = .14). In 2018, the only year for which an open response was used, the number of indoor tanning sessions per respondent ranged from 1 to 200, with a weighted mean of 27.4 and median of 9.2. In 2018, 44.4% of indoor tanning users reported 11 or more tanning sessions in the past 12 months and 24.0% reported 25 or more sessions, nearly double the 12.6% who reported 25 or more sessions in 2007.
FIGURE 2—
Indoor Tanning (IT) Frequency Among Those Reporting Past-Year IT: Health Information National Trends Survey, United States, 2007–2018
Note. Percentages are weighted.
aFor 2018, this question was posed in an open-ended manner. For this analysis, the open responses were collapsed into the previously used categories.
Indoor Tanning and Legislation
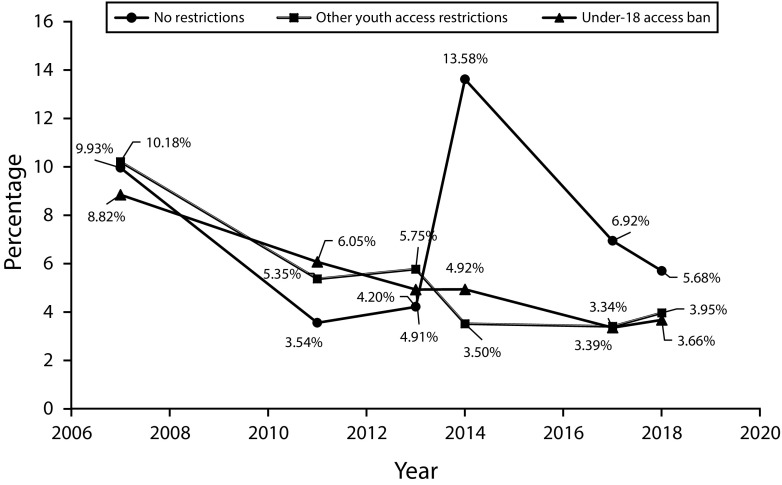
Table 1 reports overall indoor tanning prevalence for states’ respective indoor tanning youth access legislation category and regression results. Respondents in states with an under-18 access ban in 2018 averaged an indoor tanning prevalence rate of 5.1% across all years; those with some legislation averaged 5.3%, and those with no legislation averaged 7.4%. The linear regression model for indoor tanning over time from 2007 to 2018 among states with an under-18 access ban demonstrated a significant decrease (P < .001), with the moderator of legislation year also significant (P < .05). A significant decrease was also observed among states with some legislation (P < .001). Among states with no legislation, indoor tanning did not significantly decrease over time (P = .53). A test of the interaction effect of cycle year and legislation category was not statistically significant (P = .93). Figure 3 shows changes over time by legislation category.
FIGURE 3—
US Adult Indoor Tanning Prevalence (Weighted) by 2018 Indoor Tanning Youth Access Legislation Category: Health Information National Trends Survey, United States, 2007–2018
DISCUSSION
Results from this analysis demonstrate that indoor tanning significantly decreased over time among the US adult population from 2007 to 2018, a broad time frame that allows for an expansive examination of this encouraging development in public health. This decrease was also observed among the most frequent users—young adults aged 18 to 34 years. In 2007, about 1 in 7 US young adults reported using indoor tanning in the past year; in 2018, this figure decreased to 1 in 25. However, a remaining challenge is that today’s indoor tanning population is enriched with frequent users; 24% of indoor tanners reported high rates of indoor tanning in 2018 (≥ 25 times during the past year), compared with 13% in 2007. As such, very frequent tanning appears to be a significant problem among those who still use tanning beds. Emerging research on tanning addiction supports this result, according to a recent review that described excessive tanning among some users, as well as the addictive properties of ultraviolet radiation.19 This is also supported by the hardening hypothesis,20 which states that tobacco control has had the most success among those who found it easier to quit and were likely less addicted to nicotine. In the case of indoor tanning, it is possible that highly frequent, potentially addicted users are likely to continue tanning as indoor tanning regulations continue, whereas less committed or addicted users have ceased tanning over time. We agree that better interventions are critical to curb excessive tanning.
Most indoor tanners in this analysis were women. In 2007, nearly 1 in 4 adult women aged younger than 35 years reported past-year indoor tanning; in 2018, this figure decreased to 1 in 20. Appropriately, young women have been the subject of much indoor tanning research. Although men’s reported tanning prevalence was higher than reported elsewhere,14 in 2018 it was similar to that of women (about 4%). Additionally, men accounted for 27% of all adult indoor tanners; future interventions should recruit men as well as gender minorities to better understand and prevent tanning among all people.21,22
The findings of this study also demonstrate differences in reduction of adult indoor tanning over time by the presence or absence of indoor tanning youth access legislation. The interaction tested between legislation category and cycle year did not indicate that legislation category (under-18 access ban, other youth access restrictions, or no legislation) moderates the decrease of indoor tanning over time. However, analyses of the 7 states that have no age restrictions on indoor tanning use15 indicate no significant reduction over time; by contrast, significant reductions over time were found for the 28 states with some indoor tanning youth access legislation and for the 16 states with an under-18 access ban for indoor tanning. Thus, it is possible that over time, as states introduced indoor tanning youth access legislation (which typically became only more restrictive over time), the restrictions and the publicity about them led to steeper decreases in tanning over time. States with other youth access legislation did not appear to have a statistically different outcome in tanning over time compared with states with an under-18 access ban; these findings are consistent with the Social Amplification of Risk Framework,16 as it is possible that media coverage and interpersonal interactions following any legislation amplified perceptions of risk as a function of the attention that legislation garners. Public risk perceptions can be amplified by events or widely disseminated publicity.16 For example, California was the first state to implement an under-18 access ban on indoor tanning, and compared with before the legislation, long-term media coverage following the ban included significantly more skin cancer risk information disseminated widely.23 HINTS data sets include general cancer risk perception items and once included a skin cancer–specific risk perception item; a future analysis of skin cancer–specific risk perceptions over time may be valuable for understanding reduced indoor tanning behavior.
The association between adult indoor tanning and state indoor tanning youth access legislation has not been examined in prior research. A recent systematic review of 7 studies found that, overall, legislation was associated with a slight decrease in youth indoor tanning.24 One study by the Centers for Disease Control and Prevention found that indoor tanning youth access legislation, particularly legislation including age restrictions, has helped to significantly reduce indoor tanning among female high school students.25 However, a study of indoor tanning before and after the New Jersey access ban for ages 17 years and younger found no reduction in youth tanning following the ban26; lack of tanning facility compliance with age restrictions or parental accompaniment laws may contribute to mixed effects.27 Additionally, studies may require a longer time frame to find larger effects.24 Further work is needed to better understand the role of state youth access legislation in tanning prevalence.
Limitations
Several limitations must be considered in interpreting these findings. HINTS is a cross-sectional survey; this analysis lacked the ability to examine changes in individuals over time, and instead looked at changes at the population level over time. The incidence of missing data for indoor tanning was higher in 2018, which is likely a result of the open-ended format. Indoor tanning frequency in 2018 may not be comparable with the other data because of the open-ended format that was introduced in this cycle. Outdoor tanning data were not available to analyze over time; it is possible that outdoor tanning increases as a potential replacement for indoor tanning.28
Importantly, it is not possible to determine a causal relationship between legislation and reduced tanning prevalence. Historical shifts in indoor tanning regulation, such as the classification of indoor tanning as a group 1 carcinogen,7 the Food and Drug Administration’s regulation of indoor tanning, and a federal indoor tanning tax through the Affordable Care Act, may also partially explain lower indoor tanning prevalence over time. States that passed legislation may also differ from those that did not in ways that affect indoor tanning, such as geography. Additionally, examining legislation by implementation year for legislation other than under-18 bans, such as parental accompaniment and permission laws, was beyond the scope of the current study because of an inability to precisely confirm many implementation dates. However, tanning legislation typically changes to become more restrictive over time, and public perception and behavior may have shifted in association. Even unpassed legislation may communicate risk through media coverage. For example, a 2009 article from NBC News, titled “Cancer Fears Have States Mulling Teen Tan Bans,”29 described the dangers of indoor tanning in the context of several proposed state bills, many of which ultimately did not pass that year. These bills resulted in original media coverage about the dangers of indoor tanning in 2009; eventually, several of the 17 states referenced in the article passed restrictions and bans. Categorizing states according to their current legislation best captured the potential impact of these laws over time without compromising power and accuracy. The law-making process, media reporting, and public health have complicated connections that should be further explored.
Public Health Implications
The reduced adult indoor tanning prevalence reported here and elsewhere14 is a positive development for public health in the United States. This study uniquely contributes to the understanding of indoor tanning prevalence in the US population by reporting that rates of adult indoor tanning also went down in states with legislation restricting indoor tanning for minors, and by examining a period of 11 years, broader than previous studies. Findings demonstrate that indoor tanning prevalence decreased significantly among US adults as well as among young adults, women, and men, and decreased more in states that enacted indoor tanning legislation than in those that did not. Despite these positive developments over the past decade, melanoma rates are still rising.2 Potentially high levels of outdoor tanning,30 and the fact that many persons in the United States are former indoor tanners,31,32 are likely contributing factors. There are future opportunities in public health research to reduce all forms of tanning through interventions, to study appearance-based motives for all tanning, to prevent excessive tanning, and to strengthen legislative efforts for further reduction of indoor tanning.
ACKNOWLEDGMENTS
This work was supported by the National Cancer Institute, National Institutes of Health (grant no. P30 CA008748 and T32 CA009461).
We acknowledge the staff of HINTS, and in particular Richard P. Moser, PhD, for providing support in the planning stages of the study.
CONFLICTS OF INTEREST
No authors have conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not required because the study used de-identified, publicly available data.
REFERENCES
- 1.American Cancer Society. Cancer facts & figures 2018. Available at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf. Accessed December 19, 2019.
- 2.Noone A, Howlader N, Krapcho M SEER cancer statistics review, 1975–2015. National Cancer Institute, 2018. Available at: https://seer.cancer.gov/csr/1975_2015. Accessed December 19, 2019.
- 3.Thrift AP, Gudenkauf FJ. Melanoma incidence among non-Hispanic whites in all 50 United States from 2001 through 2015. J Natl Cancer Inst. 2019 doi: 10.1093/jnci/djz153. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. The known health effects of UV. Updated 2019. Available at: http://www.who.int/uv/faq/uvhealtfac/en. Accessed December 19, 2019.
- 5.Boniol M, Autier P, Boyle P et al. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ. 2012;345:e4757. doi: 10.1136/bmj.e4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wehner MR, Shive ML, Chren MM et al. Indoor tanning and non-melanoma skin cancer: systematic review and meta-analysis. BMJ. 2012;345:e5909. doi: 10.1136/bmj.e5909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Autier P. Carcinogenic to humans: why the International Agency for Research on Cancer added indoor ultraviolet (UV) tanning to group I. Melanoma Lett. 2010;28:1–5. [Google Scholar]
- 8.Gambla WC, Fernandez AM, Gassman NR et al. College tanning behaviors, attitudes, beliefs, and intentions: a systematic review of the literature. Prev Med. 2017;105:77–87. doi: 10.1016/j.ypmed.2017.08.029. [DOI] [PubMed] [Google Scholar]
- 9.Guy GP, Berkowitz Z, Holman DM et al. Recent changes in the prevalence of and factors associated with frequency of indoor tanning among us adults. JAMA Dermatol. 2015;151(11):1256–1259. doi: 10.1001/jamadermatol.2015.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghiasvand R, Rueegg CS, Weiderpass E et al. Indoor tanning and melanoma risk: long-term evidence from a prospective population-based cohort study. Am J Epidemiol. 2017;185(3):147–156. doi: 10.1093/aje/kww148. [DOI] [PubMed] [Google Scholar]
- 11.Cust AE, Armstrong BK, Goumas C et al. Sunbed use during adolescence and early adulthood is associated with increased risk of early-onset melanoma. Int J Cancer. 2011;128(10):2425–2435. doi: 10.1002/ijc.25576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watson M, Shoemaker M, Baker K. Indoor tanning initiation among tanners in the United States. JAMA Dermatol. 2017;153(5):470–472. doi: 10.1001/jamadermatol.2016.5898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Surgeon General’s Call to Action to Prevent Skin Cancer. Washington, DC: US Dept of Health and Human Services, Office of the Surgeon General; 2014. [Google Scholar]
- 14.Guy GP, Watson M, Seidenberg AB et al. Trends in indoor tanning and its association with sunburn among US adults. J Am Acad Dermatol. 2017;76(6):1191–1193. doi: 10.1016/j.jaad.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Conference of State Legislatures. Indoor tanning restrictions for minors: a state by state comparison. 2018. Available at: https://www.ncsl.org/research/health/indoor-tanning-restrictions.aspx. Accessed May 27, 2019.
- 16.Pidgeon N, Kasperson RE, Slovic P, editors. The Social Amplification of Risk. Cambridge, UK: Cambridge University Press; 2003. [Google Scholar]
- 17.HINTS 5 Cycle 2 Methodology Report. Bethesda, MD: National Cancer Institute; 2018. [Google Scholar]
- 18.Analytics Recommendations for HINTS 5, Cycle 2 Data. Bethesda, MD: National Cancer Institute; 2018. [Google Scholar]
- 19.Stapleton JL, Hillhouse J, Levonyan-Radloff K et al. Review of interventions to reduce ultraviolet tanning: need for treatments targeting excessive tanning, an emerging addictive behavior. Psychol Addict Behav. 2017;31(8):962–978. doi: 10.1037/adb0000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes JR. The hardening hypothesis: is the ability to quit decreasing due to increasing nicotine dependence? A review and commentary. Drug Alcohol Depend. 2011;117(2–3):111–117. doi: 10.1016/j.drugalcdep.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blashill AJ, Williams A, Grogan S et al. Negative appearance evaluation is associated with skin cancer risk behaviors among American men and women. Health Psychol. 2015;34(1):93–96. doi: 10.1037/hea0000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klimek P, Lamb KM, Nogg KA et al. Current and ideal skin tone: associations with tanning behavior among sexual minority men. Body Image. 2018;25:31–34. doi: 10.1016/j.bodyim.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Mayer JE, Swetter SM, Guild S et al. The impact of indoor tanning legislation: newspaper coverage of the risks of indoor tanning before and after the California indoor tanning ban for minors. J Cancer Educ. 2015;30(1):124–129. doi: 10.1007/s13187-014-0672-4. [DOI] [PubMed] [Google Scholar]
- 24.Reimann J, McWhirter JE, Cimino A et al. Impact of legislation on youth indoor tanning behaviour: a systematic review. Prev Med. 2019;123:299–307. doi: 10.1016/j.ypmed.2019.03.041. [DOI] [PubMed] [Google Scholar]
- 25.Guy GP, Berkowitz Z, Jones SE et al. State indoor tanning laws and adolescent indoor tanning. Am J Public Health. 2014;104(4):e69–e74. doi: 10.2105/AJPH.2013.301850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coups EJ, Stapleton JL, Delnevo CD. Indoor tanning among New Jersey high school students before and after the enactment of youth access restrictions. J Am Acad Dermatol. 2016;75(2):440–442. doi: 10.1016/j.jaad.2016.03.040. [DOI] [PubMed] [Google Scholar]
- 27.Reimann J, McWhirter JE, Papadopoulos A et al. A systematic review of compliance with indoor tanning legislation. BMC Public Health. 2018;18(1):1096. doi: 10.1186/s12889-018-5994-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hay JL, Riley KE, Geller AC. Tanning and teens: is indoor exposure the tip of the iceberg? Cancer Epidemiol Biomarkers Prev. 2017;26(8):1170–1174. doi: 10.1158/1055-9965.EPI-17-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cancer fears have states mulling teen tan bans. NBC News. 2009. Available at: http://www.nbcnews.com/id/29881127/ns/health-cancer/t/cancer-fears-have-states-mulling-teen-tan-bans. Accessed February 26, 2020.
- 30.Shoemaker ML, Berkowitz Z, Watson M. Intentional outdoor tanning in the United States: results from the 2015 Summer ConsumerStyles survey. Prev Med. 2017;101:137–141. doi: 10.1016/j.ypmed.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bowers JM, Moyer A. “I am happier with my fairer complexion”: factors associated with former indoor tanning and reasons for quitting in college women. Psychol Health Med. 2019;24(3):344–354. doi: 10.1080/13548506.2018.1537497. [DOI] [PubMed] [Google Scholar]
- 32.Banerjee SC, Hay JL, Geller AC et al. Quitting the “cancer tube”: a qualitative examination of the process of indoor tanning cessation. Transl Behav Med. 2014;4(2):209–219. doi: 10.1007/s13142-014-0257-0. [DOI] [PMC free article] [PubMed] [Google Scholar]