1. Covid-19: the problem statement
The Coronavirus disease 2019 (COVID-19) has threatened the world with a public health crisis. It took hardly a month for more than a million to be affected and nearly 80,000 fatalities after being declared as a pandemic by the World Health Organization (WHO). International borders have been locked down, travel restricted, economies slashed and billions are isolated at their own homes, as a measure to contain the outbreak (WHO Situation report as on 9 April 2020). Pandemics can extend beyond just the purview of medicine. The psychological and economic consequences of biological disasters have shown to outlast the infection itself. As the therapeutic focus is mainly restricted to biological therapies worldwide to develop an effective cure for the virus, the deep-rooted psycho-social repercussions are often neglected (Singhal, 2020). The widespread lockdown, uncertainty of the infection, prevalent misinformation on the media and lack of a definitive cure are driving mass-hysteria, anxiety, fear and stigmatization. Research on pandemic protocols in the past have shown the role of psycho-social preparedness in improving the resilience during a ‘biological disaster’ like such large-scale infections. Though there are well-known international guidelines for disaster management in general, specific ones guided to pandemic-preparedness are lacking, though some countries have formulated their own policies (Colizza et al., 2007). Psychological preparedness for COVID-19 has shown to affect the response and spread, based on perspectives from India (Banerjee, 2020). Effectiveness, applicability and feasibility are attributes which indicate that the psychosocial interventions are going to be more appropriate in the community as the knowledge, attitude and practice (KAP) regarding any new infection improves the preparedness in both the health-care professionals and the general public.
2. The proposed intervention: a community tool-kit
Preparedness towards any form of disasters is vital to reduce their impact. As the global situation related to COVID-19 is changing rapidly each day, ‘Community Based Disaster Preparedness’(CBDP) is perhaps the method of management. CBDP is a response mechanism in an attempt to save the maximum and effective community triage (Troy et al., 2008). This leads to multi-pronged but flexible interventions to reduce vulnerability and build a self-reliant and resilient society. It is true that pandemics of such epic proportions cannot be fully controlled by any degree of preparedness but the goal here is more of harm-reduction. Earlier outbreaks have highlighted important areas. During the Zika outbreak in Brazil that eventually spread to North and South America, WHO had declared it too as a public health emergency of international concern, just like COVID-19 (World Health Organization, 2017). Smith (2006) has spoken about the long-lasting effects of the SARS outbreak in China and the increase in prevalence of mental disorders as well as increased unemployment, poverty, overcrowding, homelessness, chaos and violence in the aftermath. These factors can get more vital during COVID-19 as it is extremely contagious with increased human-human transmission. Research had been conducted to understand the preparedness of community-based psychosocial toolkit for ZIKA virus affected-areas (Nair et al., 2020), wherein it was understood that the lack of understanding about a new condition and uncertainty about it has a direct correlation with the preparedness among the healthcare professionals, and thereby implying policy planning and training needs to gear up towards this. As health-care professionals we mostly include the general physicians and nurses at the community level, as they form the backbone of primary healthcare in most countries.
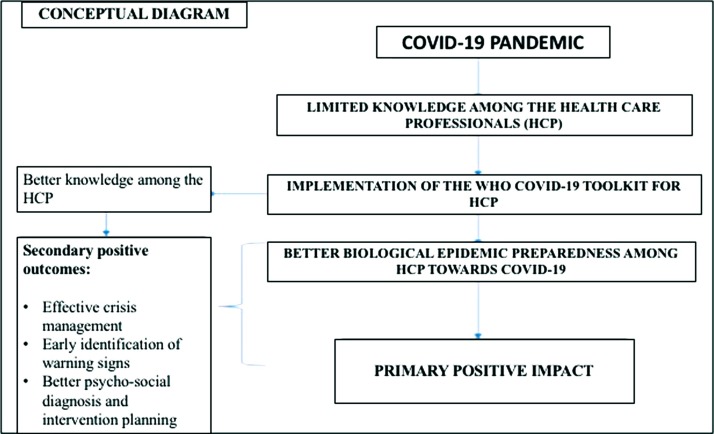
The purpose of this proposed intervention toolkit is to aid facilitators to bring about ownership for sustainability of the process during a pandemic. Better preparedness during an infection leads to better resource allocation which in turn helps better intervention planning and community integration (Fig. 1 ). Here we use the model of the Zika virus preparedness toolkit to propose a similar one for the ongoing COVID-19.
Fig. 1.
Conceptual Diagram of the Proposed Program Implementation (Attached separately).
3. A stepped-approach to psycho-social interventions
3.1. Step 1: collection of basic information
Before planning any intervention, the first step is always gauging the problem statement and understanding the basic attitudes and beliefs of the people towards the crisis. Considering the pandemic as an ongoing process, regular updated data should be collected and assimilated from the global health agencies like WHO, CDC, and regional health ministries (like the ICMR and Ministry of Health and Family Welfare in India, CDC in China, etc.). Collaboration with the media to provide unbiased information will be helpful. As social distancing makes field visit difficult, online surveys or telephonic communication might yield valuable information. The content of queries from the helplines and crisis intervention at the hospital emergency settings will help understand the various types of psycho-social problems. People with pre-existing mental disorders, people in isolation, the elderly and those institutionalized are more vulnerable and thus need to be contacted separately to ensure that their physical and medical needs are met. Liaison with nearby health-care centres and integration of alternative medicine specialists will be helpful.
3.2. Step 2: Crisis management: knowledge, attitude and practices in the advent of a biological disaster
Table 1.
Crisis Management Modules.
| Module # | Session Name | Methodology |
|---|---|---|
| Pre-assess | Introduction of the Intervention programme | Ice Breaking games |
| Module 1.1 | Supportive Communication | Lecture Method, Games |
| Module 1.2 | Health & Antenatal care of pregnant women | Audio-Visual Aids |
| Module 1.3 | Clinical evaluation and management of elderly | Lecture Method |
| Module 2.1 | Defining, assessing risk factors for immunocompromised conditions. | Lecture Method, Case Vignette explanation |
| Module 2.2 | Method of communication with affected people | Audio-Visual Aids |
| Module 2.3 | History taking methodology and identification | Role Play, Lecture Method |
| Module 2.4 | Method of Monitoring and supportive care | Lecture Method |
| Module 3.1 | Assessing current stressors, coping strategies and social support | Audio-Visual Aids, Lecture Method |
| Module 3.2 | Preparing an effective treatment management | Group brainstorming activity |
| Module 3.3 | Management of mental health conditions | Lecture method |
| Module 3.4 | Awareness of the phases of the Covid19 | Lecture Method, Role Play |
| Post-Assessment | Termination - Feedback | Summarization |
3.3. Step 3: Communication amongst all
In this section post the interventions, the goals are
-
•
To understand that situation, focussing on current ‘crisis at hand’ and hence survival, protection and sustenance are necessary.
-
•
Minimise the contact, maintain the essential services and to maximise the help to others but maintaining the prevention.
-
•
Immediate ideal response might not be possible but to reduce the infection, exposure needs to be reduced and insight needs to be improved.
-
•
Authentic sources of information like WHO, Centre for Disease Control and Prevention (CDC), etc.
-
•
Debunking misinformation: suggested distance from social media
-
•
Community awareness camps through audio-visual or print media (relevant update about the precautionary measures and pandemic situation)
-
•
Channels of communication to those in isolation/quarantined
3.4. Step 4: individual
-
•
Self-Isolation and restrict travel
-
•
Physical but not ‘social’ distancing
-
•
Protection of self (hand and respiratory hygiene)
-
•
Reduce ‘digital screen time’
-
•
Address panic, uncertainty and fear: encourage active usage of helplines
3.5. Step 5: Friends/Family
-
•
Share safe spaces
-
•
Have mutual help
-
•
Isolate from individuals who have the symptoms
3.6. Step 6: community
-
•
Identifying Zones and Guarding boundaries
-
•
Organize no-contact delivery of necessities
-
•
Certify safe individuals and screen members for symptoms
-
•
Provide no-contact care for those isolated
-
•
Expand shared safe space facilities and services
-
•
Organize 24 * 7 helplines for counselling
3.7. Step 7: organizations
In this section communication is stressed on:
-
•
Work from Home
-
•
Ensure continuation of employment
-
•
Encourage social distancing
-
•
Safe space workshops
-
•
Separate containment wards (if necessary)
-
•
Compulsory masks for patients and healthcare members
-
•
Quarantine for new individuals/those with history of travel for at least 14–21 days
-
•
Training the security and other ground level staff for screening of symptoms
-
•
Constant cleaning/disinfecting and replacing of the floors
-
•
Sanitizing the tables and floors or any touch surfaces with alcohol rubs
-
•
Providing hand sanitizers at entrance and exits
-
•
Sensitization to the mental health of the employees (webinar or helpline interaction)
The steps mentioned above can be organized in the form of pamphlets and other IEC materials to ensure the sustenance and easy dissemination of the module. IT liaison can be sought for to even incorporate them in smart-phone applications and software for easy accessibility. Module training can also be done online for the paramedical personnel and health-care support staff.
4. Lessons learnt and the way forward
During the period of a global outbreak, especially in the context of a biological disaster, an individuals’ initial instinct is to come to a clinic for a consultation and the first point of contact are the nurses and the general physicians. It has been mentioned that nurses and primary health-care workers are in a stature where they are able to identify the early signs and symptoms of an infection and help in early interventions (Gould, 2013). They are uniquely equipped with the ability to integrate psycho-social health into the public health, thus sensitizing the other specialities. Early and simple step-wise flexible social interventions provided by primary health-care workers are effective in improving the long-term effects. Such community based stepped interventions using precautionary and psychological strategies have been used for emergency care workers, health-care staff and quarantined people in Wuhan, China and found to increase the degree of work satisfaction, decrease absenteeism and increase the compliance to quarantine instructions (Chau et al., 2016). Earlier studies during the Nipah and Influenza virus outbreaks, also impress upon the need for useful communication techniques, as reaching out to the masses is the key (Kumar and Kumar, 2018). Our module proposes to include the same.
The World Health Organization has standard protocols during periods of epidemics and pandemics which work the best in accordance with the set rules of any country, but the focus remains that for a long period of time various administrative agencies have not implemented or modified the strategies to suit the crisis needs (Melnychuk and Kenny, 2006). Sadly we keep needing a new threat to revise our policies! Given the recent trajectory of the Kerala Floods in India, Zika in Brazil, Ebola in Africa and, finally COVID-19 globally, it is important we realize the need for simple tools to guide pandemic preparedness and containment, besides dedicated search for virus-specific biological therapies.
At times when an unknown infection threatens community transmission in many countries, causing panic and hysteria at the societal level, it is important to have structured psychosocial interventions to improve awareness and ensure that the first level steps taken by the primary health-care workers, can provide some degree of damage control. We expect the proposed toolkit to serve this purpose. Challenges can be its effective implementation, standardisation of the steps, impediment by social distancing as well as comparability in different countries and socio-economic strata. However, as our studies are in progress in India using the tool-kit at the community level, we expect more consistent findings to supplement this literature in the near future.
Financial disclosure
Nil.
Declaration of Competing Interest
None.
Acknowledgement
Nil.
References
- Banerjee Debanjan. Psychological preparedness for the COVID-19 pandemic, perspectives from India. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau W., et al. The Psychosocial Aspects of a Deadly Epidemic: What Ebola Has Taught Us About Holistic Healing: What Ebola Has Taught Us About Holistic Healing. ABC-CLIO; California: 2016. SARS epidemic on Chinese health professionals: implications for epidemics including Ebola. [Google Scholar]
- Colizza V., et al. Modelling the worldwide spread of pandemic influenza: baseline case and containment interventions. PLoS Med. 2007;4(1) doi: 10.1371/journal.pmed.0040013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould D. Outbreaks of infection in community settings: The nursing implications. Primary Health Care. 2013;23(3) [Google Scholar]
- Kumar A., Kumar A. Deadly Nipah outbreak in Kerala: lessons learned for the future. India. J. Crit. Care Med. 2018;22(7):475. doi: 10.4103/ijccm.IJCCM_282_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnychuk R., Kenny N. Pandemic triage: the ethical challenge. Cmaj. 2006;175(11):1393. doi: 10.1503/cmaj.061322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair V., Sekar K., Thomas P. Knowledge among nursing students on zika preparedness. Acta Sci. Neurol. 2020;3(3) [Google Scholar]
- Smith R.D. Responding to global infectious disease outbreaks: lessons from SARS on the role of risk perception, communication and management. Social Sci. Med. 2006;63(12):3113–3123. doi: 10.1016/j.socscimed.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singhal T. A review of coronavirus disease-2019 (COVID-19) The Indian Journal of Pediatrics. 2020:1–6. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troy D.A., Carson A., Vanderbeek J., Hutton A. Enhancing community-based disaster preparedness with information technology. Disasters. 2008;32(1):149–165. doi: 10.1111/j.1467-7717.2007.01032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO; 2017. WHO Toolkit for the Care and Support of People Affected by Complications Associated With Zika Virus, s.l. [Google Scholar]
- World Health Organization . WHO; 2020. Coronavirus Disease 2019 (COVID-19): Situation report., s.l. [Google Scholar]